Abstract
Artificial intelligence-based prediction technologies have allowed definition of T-cell epitopes presented by Major Histocompatibility Complex (MHC) molecules with allele-specificity of presentation. While some have utilized these technologies on a smaller scale, recent work has expanded the workable proteome size, leveraged both classes of Major Histocompatibility (MHC) molecules, extended the range of host species assessed during comparative analysis, and incorporated pathogen genetic diversity to highlight broadly useful epitopes. A recent study focused on the zoonotic pathogen Coxiella burnetii exemplifying themes and possibilities for future analyses. These data suggest an expanding role for epitope prediction in rational vaccine design for a very broad range of pathogen and host systems.
Keywords
T-cell epitope, Machine-learning, Artificial intelligence, Major histocompatibility complex, Proteome-wide
Commentary
Vaccine development began in the 1790’s when Edward Jenner used cowpox to confer protection against the smallpox virus [1]. The field of vaccinology has greatly expanded since then, wherein vaccination has been a valuable tool in the decline of many diseases [1,2]. While Jenner’s use of cowpox shares attributes to a live-attenuated vaccine, there are alternate methods of vaccination, which include subunit, conjugate, mRNA, viral vector, and toxoid vaccines [2-4]. Development of these methods was facilitated through greater understanding of the immune response, elucidation of both host and pathogen genetic diversity, and advancement of laboratory techniques [1-3]. The most recent notable advancement in vaccine production was the development of a nucleic acid vaccine to combat the SARS-CoV-2 virus [1]. While advancement in vaccine methodology can be readily seen, many subunit-based vaccines end up generating a predominantly B-cell driven response [1,5].
B-cells are responsible for differentiating into plasma cells and mediating antibody production [1,6,7]. Antibodies are important during the immune response as they mediate opsonization for complement and innate immune cells;however, they can also inactivate circulating viruses [8]. Identification of B-cell immunogens typically relies on antibody responses seen in patients that have survived previous infection with the agent of interest [9-11].
In addition, it is well known that T-cell immunity plays an important role in host defense against infection, and it is becoming increasingly evident that vaccine production needs to incorporate T-cell recognition of pathogens [1,12]. This idea is inherently important to infectious agents that require a T-cell helper 1 (Th1) phenotype, as cellular immunity is the cornerstone to agent clearance [13-15]. It is possible that the ability to use whole cell inactivated or live-attenuated strains has previously limited the requirement to assess T-cell epitopes, or peptides that allow T-cell recognition of a pathogen [1,3]. Still, the need to generate vaccines against agents that are either difficult to culture or those that require a high-level containment facility suggests the necessity of accurately defining T-cell epitopes [1,3,16].
Recognition of agent presence by T-cells relies on the major histocompatibility complexes (MHC) present on the surface of other cell types [17-19]. There are two classes of MHC alleles, namely MHC Class I (MHCI) and MHC Class II (MHCII) [17].MHCI exists on the surface of most cell types and as such is important in the designation of compromised host cells to cytotoxic T-cells, or CD8+ T-cells [17-20]. Therefore, MHCI is inherently responsible for alerting the immune system to an intracellular pathogen [7,18]. In contrast, MHCII marks antigen presenting cells (APCs) consisting of dendritic cells, macrophages, and B-cells [7]. Recognition of a loaded MHCII by CD4+ T-cells, or T-helper cells, initiates the production of an organized adaptive immune response, so it is required for response to most pathogens [7,17].
Bioinformatic programs delineating T-cell epitopes started to be developed in 2007 [3,20,21]. Labs studying virology-based interaction with the immune system were able to use these programs to identify T-cell epitopes within the entire viral proteome [22]. Due to the size difference between viral and bacterial proteomes, bacteriology-based research continued to narrow the proteins of interest based on other constraints [23-26]. While this methodology can identify proteins that interact with T-cells over the course of infection, there are likely highly qualified immunogens that will be missed by limiting queried proteins. Recently published work has achieved one of the two known proteome-wide T-cell epitope analyses within a bacterium [22,27] while advancing numerous other aspects of larger-scale analysis, such as avoiding induction of autoimmune responses, improved capture of pathogen genetic diversity, leveraging diversity within hosts, and comparing results across different hosts of the same pathogen.
Pathogen protein conservation has been of specific concern during vaccine development, especially when considering profoundly variable genomes or rapidly mutating agents [4,18]. Previous work with bacterial agents has completed proteome-wide alignments to identify the core- and pangenome. However, while these studies have used a large pool of bacterial isolates, they have not fully considered bacterial groupings within certain species [24,26,28]. Choice isolates will include factors like alternate virulence during inoculation studies, isolation from differing host species, or large genomic rearrangements [27]. Leveraging phylogenetically diverse isolates is recommended [27,29], and this step can be enhanced by choosing isolates which arose from diverse hosts and capture a range of the most important virulence phenotypes [29-32].
While prior vaccine design studies have commonly employed agent conservation to narrow the proteins of interest, there are many investigations that do not consider host homology [22,24,25]. Homology of agent proteins to the proteins found in host species is important to recognize as sensitization of the host immune system to these macromolecules could cause an autoimmune reaction [28]. Previous work examining either allergy responses or autoimmune reactions can suggest acceptable cut-off values for homology between agent and host [28,33]. Genome-wide analysis for each host of interest generates a dataset that is better viewed in matrices rather than individual records, and numerous programs can accomplish such matrix analyses, including BLASTGrabber, BlastViewer, BlasterJS, and JAMBLAST [34-36]. At this stage many previous studies have limited the proteins of interest based on antibody responses, surface localization, or secretion of proteins [3,23-26,28,37,38]. However, this technique can fail to identify strong immunogens during initial screening. Therefore, to enhance the outcome of predicted T-cell epitopes, no further protein limitation should be performed.
Bioinformatic tools have been developed to model each processing step for T-cell recognition of an antigen. These levels of processing include proteasomal cleavage, TAP interaction, MHCI/MHCII binding, and T-cell recognition [17,20,39,40]. Of these events, binding of antigens to MHC alleles is the most selective stage for antigen recognition [17]. Tools which define MHC loading of antigen consist of both binding affinity matrices and machine-learning. In silico identification of T-cell epitopes began by using matrices that examined the ability of the MHC binding groove to interact with the R-side groups of amino acids present in agent peptides. This methodology was expanded into machine-learning through generation of support vector machine (SVM) and artificial neural network (ANN) based bioinformatic tools [17,18]. With these programs, data pools that contained either experimentally defined antigens or random peptides were exploited to train tools on alleles of interest [18,20]. Once trained, these programs were able to expand into delineating T-cell epitopes for MHC alleles that had not been directly studied previously [20,21]. Available tools that encompass machine-learning include ANNPRED, MHC2Pred, ConvMHC, NN_Align 2.3, NetMHC, SVMHC, KISS, SVRMHC, DeepHLAPan, and IEDB binding [18,41].
As with the pathogen proteins, maintaining diversity is also imperative when it comes to the host side of vaccine production. Human sequencing of MHC alleles has thus far defined approximately 13,000 different sequences worldwide. This information is organized on the Allele Frequency Net Database (AFND) by geographic region, genomic locus, and data collection standards [42]. This allows investigators to better refine alleles of interest by generation of phylogenetic trees to accomplish preservation of host allele heterogeny, while encompassing a worldwide distribution. Prior to this work, many researchers would focus on the known supertype alleles, which are suggested to be present in 88% of the population and bind similar antigens compared to one another [18,25,38]. Extending the allelic pool tested from the known supertype alleles not only allows for a decrease in the number of false positives returned from analysis but also permits a larger representation of populations.
Along with the profound list of human alleles available on most T-cell epitope defining databases, there are certain databases which strive to encompass alternate vertebrate species. The most common of these being murine alleles of inbred strains of mice [18]. Recent work within the lab has pushed these limits further by incorporating bovine MHCI alleles into the analysis. The importance of expanding host alleles of interest rests in both the zoonotic nature of certain pathogens and in the development of veterinary vaccines. Inclusion of alternate species MHC alleles into machine-learning programs requires two steps. The first of these is expanding the vertebrate allelic sequences available to represent, not only alternate organisms, but breeds and regions specific to these species [43-45]. The second step to increase species representation is to generate elution data based on defined MHC alleles of interest [20,21]. The difficulty in these efforts regards the structural differences between the MHCI and MHCII molecules. MHCI molecules generally bind 9-mer long peptide sequences and have a binding pocket that is closed, making delineation of allele specificity easier to define. In comparison, MHCII molecules have an open binding pocket, increasing the complexity of elucidating the core binding region of studied peptides [17,18]. Reynisson et al. have attempted to solve this problem by using motif deconvolution methods, wherein evaluation of the new program determined a decrease in false positive data [21,46]. At the moment, NetMHCpan 4.1 maintains the largest selection of host species alleles, encompassing human, nonhuman primates, mouse, swine, bovine, canine, and equine species [18,20]. Furthermore, there is the possibility to use self-defined alleles of interest within certain bioinformatic tools [20]. This may help surpass the initial issue of training data availability for alternate vertebrate species, but one must keep in mind that increasing the evolutionary distance will inevitably affect the predictive value of the program [21].
Beyond the call for increased training on alternate host MHC alleles, there is the paradigm shift to proteome-wide assessment of multiple MHC varieties. Of the two existing proteome-wide T-cell epitope studies, one focused on MHCI based T-cell epitopes and the other determined T-cell epitopes for MHCI and MHCII [22,27]. Assessing MHCII loading of antigens is of major importance as this mediates adaptive immunity organization and response [17]. As mentioned previously, this cellular immunity priming is required for elimination of certain pathogens [1,13,47]. The results obtained from assimilating each of these methods will require alternate evaluation strategies as compared to previous bioinformatic techniques. This is due to previous analysis producing a manageable number of records in relation to the big data produced previously [37,39,48]. Analytical approaches may be comprised of isolating T-cell epitopes which interact with a high number of tested alleles, proteins that have a certain number of T-cell epitopes present, and T-cell epitopes returned during inquiry of both MHC classes [27,39,40]. Notably, this examination should be derived based on the pathogen of interest and the desired vaccine methodology. Following identification of T-cell epitopes, it should be ascertained whether the identified peptides elicit a cellular response when host or model organisms are exposed to the peptides of interest. A method frequently employed during this analysis is the ELISpot assay, which can assess the production of cytokines by isolated T-cells [23,38,49]. This will promote validation or disqualification of the T-cell epitopes previously defined bioinformatically.
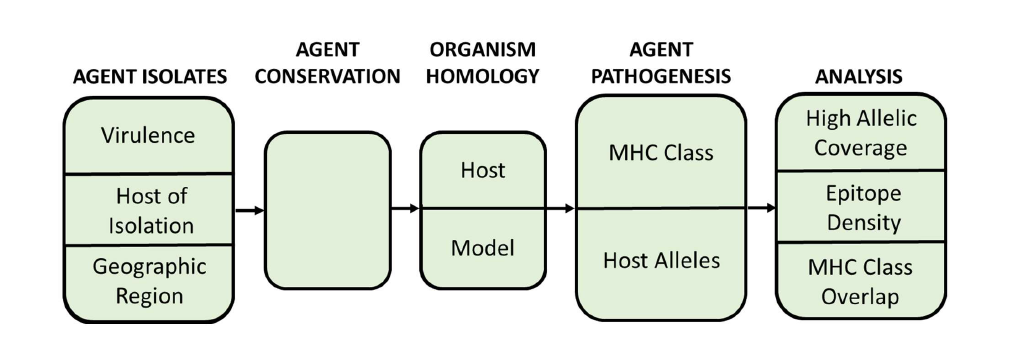
A flow-chart encompassing an overview of the presented methodology is depicted in Figure 1. Expansion of this methodology may allow for analysis of pathogens with substantially larger genome sizes, such as apicomplexans [50]. Work on apicomplexan vaccinations has become progressively more important due to the emergence of drug resistance [51]. Generation of an apicomplexan database examining peptide:allele interactions would be of considerable size; however, there are multiple questions that can be considered and answered through use of such a database.
In cases where pathogens can infect multiple hosts, the ability to analyze many hosts simultaneously can harmonize vaccine design efforts to achieve efficiencies in testing and overall cost savings [27]. There are many opportunities for application of proteome-wide epitope prediction analyses in rational vaccine design of pathogens with large proteomes. The benefits can include de novo vaccine situations, as well as T-cell response optimization of older designs. Thus, proteomewide epitope prediction will be a useful tool in rational vaccine design for a wide variety of pathogens.
References
2. Jorge S, Dellagostin OA. The development of veterinary vaccines: a review of traditional methods and modern biotechnology approaches. Biotechnology Research and Innovation. 2017 Jan 1;1(1):6-13.
3. Movahedi AR, Hampson DJ. New ways to identify novel bacterial antigens for vaccine development. Veterinary Microbiology. 2008 Sep 18;131(1-2):1-3.
4. Rajão DS, Pérez DR. Universal vaccines and vaccine platforms to protect against influenza viruses in humans and agriculture. Frontiers in Microbiology. 2018 Feb 6;9:123.
5. Garg R, Babiuk L, Gerdts V. A novel combination adjuvant platform for human and animal vaccines. Vaccine. 2017 Aug 16;35(35):4486-9.
6. Cyster JG, Allen CD. B cell responses: cell interaction dynamics and decisions. Cell. 2019 Apr 18;177(3):524-40.
7. Pennock ND, White JT, Cross EW, Cheney EE, Tamburini BA, Kedl RM. T cell responses: naive to memory and everything in between. Advances in Physiology Education. 2013 Dec;37(4):273-83.
8. Forthal DN. Functions of antibodies. Microbiology Spectrum. 2014 Aug 15;2(4):2-4.
9. Beare PA, Chen C, Bouman T, Pablo J, Unal B, Cockrell DC, et al. Candidate antigens for Q fever serodiagnosis revealed by immunoscreening of a Coxiella burnetii protein microarray. Clinical and Vaccine Immunology. 2008 Dec;15(12):1771-9.
10. Miller HK, Kersh GJ. Analysis of recombinant proteins for Q fever diagnostics. Scientific Reports. 2020 Dec 1;10(1):1-8.
11. Vigil A, Ortega R, Nakajima-Sasaki R, Pablo J, Molina DM, Chao CC, et al. Genome-wide profiling of humoral immune response to Coxiella burnetii infection by protein microarray. Proteomics. 2010 Jun;10(12):2259-69.
12. Read AJ, Erickson S, Harmsen AG. Role of CD4+ and CD8+ T cells in clearance of primary pulmonary infection with Coxiella burnetii. Infection and Immunity. 2010 Jul;78(7):3019-26.
13. Andoh M, Zhang G, Russell-Lodrigue KE, Shive HR, Weeks BR,Samuel JE. T cells are essential for bacterial clearance, and gamma interferon, tumor necrosis factor alpha, and B cells are crucial for disease development in Coxiella burnetii infection in mice. Infection and Immunity. 2007 Jul;75(7):3245-55.
14. Schoenlaub L, Elliott A, Freches D, Mitchell WJ, Zhang G. Role of B cells in host defense against primary Coxiella burnetii infection. Infection and Immunity. 2015 Dec;83(12):4826-36.
15. Lee JY, Chang J. Recombinant baculovirus-based vaccine expressing M2 protein induces protective CD8+ T-cell immunity against respiratory syncytial virus infection. Journal of Microbiology. 2017 Nov;55(11):900-8.
16. Marmion BP, Ormsbee RA, Kyrkou M, Wright J, Worswick DA, Izzo AA, et al. Vaccine prophylaxis of abattoir-associated Q fever: eight years’ experience in Australian abattoirs. Epidemiology & Infection. 1990 Apr;104(2):275-87.
17. Sanchez-Trincado JL, Gomez-Perosanz M, Reche PA. Fundamentals and methods for T-and B-cell epitope prediction. Journal of Immunology Research. 2017 Oct;2017.
18. Soria-Guerra RE, Nieto-Gomez R, Govea-Alonso DO, Rosales- Mendoza S. An overview of bioinformatics tools for epitope prediction: implications on vaccine development. Journal of Biomedical Informatics. 2015 Feb 1;53:405-14.
19. Turvey SE, Broide DH. Innate immunity. Journal of Allergy and Clinical Immunology. 2010 Feb 1;125(2):S24-32.
20. Nielsen M, Connelley T, Ternette N. Improved prediction of bovine leucocyte antigens (BoLA) presented ligands by use of massspectrometry- determined ligand and in vitro binding data. Journal of Proteome Research. 2018 Jan 5;17(1):559-67.
21. Reynisson B, Barra C, Kaabinejadian S, Hildebrand WH, Peters B, Nielsen M. Improved prediction of MHC II antigen presentation through integration and motif deconvolution of mass spectrometry MHC eluted ligand data. Journal of Proteome Research. 2020 Apr 18;19(6):2304-15.
22. Zvi A, Rotem S, Zauberman A, Elia U, Aftalion M, Bar-Haim E, et al. Novel CTL epitopes identified through a Y. pestis proteome-wide analysis in the search for vaccine candidates against plague. Vaccine. 2017 Oct 20;35(44):5995-6006.
23. Chen C, Dow C, Wang P, Sidney J, Read A, Harmsen A, et al. Identification of CD4+ T cell epitopes in C. burnetii antigens targeted by antibody responses. PLoS One. 2011 Mar 15;6(3):e17712.
24. Ali A, Soares SC, Santos AR, Guimarães LC, Barbosa E, Almeida SS, et al. Campylobacter fetus subspecies: comparative genomics and prediction of potential virulence targets. Gene. 2012 Oct 25;508(2):145-56.
25. Fiuza TS, Lima JP, de Souza GA. EpitoCore: mining conserved epitope vaccine candidates in the core proteome of multiple bacteria strains. Frontiers in Immunology. 2020 May 5;11:816.
26. Hisham Y, Ashhab Y. Identification of cross-protective potential antigens against pathogenic Brucella spp. through combining pan genome analysis with reverse vaccinology. Journal of Immunology Research. 2018 Dec 9;2018.
27. Piel LM, Durfee CJ, White SN. Proteome-wide analysis of Coxiella burnetii for conserved T-cell epitopes with presentation across multiple host species. BMC Bioinformatics. 2021 Dec;22(1):1-26.
28. Ali A, Naz A, Soares SC, Bakhtiar M, Tiwari S, Hassan SS, et al. Pangenome analysis of human gastric pathogen H. pylori: comparative genomics and pathogenomics approaches to identify regions associated with pathogenicity and prediction of potential core therapeutic targets. BioMed Research International. 2015 Oct;2015.
29. Hemsley CM, O’Neill PA, Essex-Lopresti A, Norville IH, Atkins TP, Titball RW. Extensive genome analysis of Coxiella burnetii reveals limited evolution within genomic groups. BMC Genomics. 2019 Dec;20(1):1-7.
30. Long CM, Beare PA, Cockrell DC, Larson CL, Heinzen RA. Comparative virulence of diverse Coxiella burnetii strains. Virulence. 2019 Jan 1;10(1):133-50.
31. Ammerdorffer A, Kuley R, Dinkla A, Joosten LA, Toman R, Roest HJ, et al. Coxiella burnetii isolates originating from infected cattle induce a more pronounced proinflammatory cytokine response compared to isolates from infected goats and sheep. Pathogens and Disease. 2017 Jun 1;75(4).
32. Seshadri R, Samuel JE. Genome sequencing of phylogenetically and phenotypically diverse Coxiella burnetii isolates. GenBank Accession. 2013(010117).
33. McClain S. Bioinformatic screening and detection of allergen cross-reactive IgE-binding epitopes. Molecular Nutrition & Food Research. 2017 Aug;61(8):1600676.
34. Neumann RS, Kumar S, Haverkamp TH, Shalchian-Tabrizi K. BLASTGrabber: a bioinformatic tool for visualization, analysis and sequence selection of massive BLAST data. BMC Bioinformatics. 2014 Dec;15(1):1-1.
35. Lagnel J, Tsigenopoulos CS, Iliopoulos I. NOBLAST and JAMBLAST: New Options for BLAST and a Java Application Manager for BLAST results. Bioinformatics. 2009 Mar 15;25(6):824-6.
36. Blanco-Míguez A, Fdez-Riverola F, Sánchez B, Lourenço A. BlasterJS: A novel interactive JavaScript visualisation component for BLAST alignment results. PLoS One. 2018 Oct 9;13(10):e0205286.
37. Xiong X, Qi Y, Jiao J, Gong W, Duan C, Wen B. Exploratory study on Th1 epitope-induced protective immunity against Coxiella burnetii infection. PLoS One. 2014 Jan 30;9(1):e87206.
38. Scholzen A, Richard G, Moise L, Baeten LA, Reeves PM, Martin WD, et al. Promiscuous Coxiella burnetii CD4 epitope clusters associated with human recall responses are candidates for a novel T-cell targeted multi-epitope Q fever vaccine. Frontiers in Immunology. 2019 Feb 15;10:207.
39. Jaydari A, Forouharmehr A, Nazifi N. Determination of immunodominant scaffolds of Com1 and OmpH antigens of Coxiella burnetii. Microbial Pathogenesis. 2019 Jan 1;126:298-309.
40. Maman Y, Nir-Paz R, Louzoun Y. Bacteria modulate the CD8+ T cell epitope repertoire of host cytosol-exposed proteins to manipulate the host immune response. PLoS Computational Biology. 2011 Oct 13;7(10):e1002220.
41. Prachar M, Justesen S, Steen-Jensen DB, Thorgrimsen S, Jurgons E, Winther O, et al. Identification and validation of 174 COVID-19 vaccine candidate epitopes reveals low performance of common epitope prediction tools. Scientific Reports. 2020 Nov 24;10(1):1-8.
42. Gonzalez-Galarza FF, McCabe A, Santos EJ, Jones J, Takeshita L, Ortega-Rivera ND, et al. Allele frequency net database (AFND) 2020 update: gold-standard data classification, open access genotype data and new query tools. Nucleic Acids Research. 2020 Jan 8;48(D1):D783-8.
43. Vasoya D, Law A, Motta P, Yu M, Muwonge A, Cook E, et al. Rapid identification of bovine MHCI haplotypes in genetically divergent cattle populations using next-generation sequencing. Immunogenetics. 2016 Nov;68(10):765-81.
44. Mikko S, Anderson L. Extensive MHC class II DRB3 diversity in African and European cattle. Immunogenetics. 1995 Sep;42(5):408-3.
45. Ballingall KT, Tassi R. Sequence-based genotyping of the sheep MHC class II DRB1 locus. Immunogenetics. 2010 Jan;62(1):31-9.
46. Reynisson B, Alvarez B, Paul S, Peters B, Nielsen M. NetMHCpan-4.1 and NetMHCIIpan-4.0: improved predictions of MHC antigen presentation by concurrent motif deconvolution and integration of MS MHC eluted ligand data. Nucleic Acids Research. 2020 Jul 2;48(W1):W449-54.
47. Buttrum L, Ledbetter L, Cherla R, Zhang Y, Mitchell WJ, Zhang G. Both major histocompatibility complex class I (MHC-I) and MHCII molecules are required, while MHC-I appears to play a critical role in host defense against primary Coxiella burnetii infection. Infection and Immunity. 2018 Mar 22;86(4):e00602-17.
48. Ghasemi A, Ranjbar R, Amani J. In silico analysis of chimeric TF, Omp31 and BP26 fragments of Brucella melitensis for development of a multi subunit vaccine candidate. Iranian Journal of Basic Medical Sciences. 2014 Mar;17(3):172.
49. Kalyuzhny AE. Handbook of ELISPOT. Methods in Molecular Biology. 2005;302:1-323.
50. Cornillot E, Hadj-Kaddour K, Dassouli A, Noel B, Ranwez V, Vacherie B, et al. Sequencing of the smallest Apicomplexan genome from the human pathogen Babesia microti. Nucleic Acids Research. 2012 Oct 1;40(18):9102-14.
51. Seeber F, Steinfelder S. Recent advances in understanding apicomplexan parasites. F1000Research. 2016;5.