Introduction
Peripheral pancytopenia is not a disease by itself; rather it describes simultaneous presence of anemia, leucopenia and thrombocytopenia resulting from a number of disease processes. Detailed clinical history and meticulous physical examination along with baseline hematological investigations, provides invaluable information in the complete workup of pancytopenic patients, helping in systematic planning of further investigations to diagnose and ascertain the cause, avoiding a battery of unnecessary tests [1].
Peripheral pancytopenia is reduction in all three major formed elements of blood to levels below their lower normal limit leading to simultaneous presence of anemia, leucopenia and thrombocytopenia [2]. Thus, it is not a disease entity by itself, but rather a triad of findings. As the severity of pancytopenia and the underlying pathology determines the management and prognosis of these patients, identifying the correct etiopathology in a given case is crucial and helps in implementing timely and appropriate treatment [3].
Detailed clinical history and meticulous physical examination along with baseline hematological investigations provide invaluable information in the evaluation of pancytopenic patients, helping in systematic planning of further investigations to diagnose and ascertain the cause, avoiding unnecessary tests which not only add to the expense of treatment but sometimes also may result in delayed diagnoses and treatment [4].
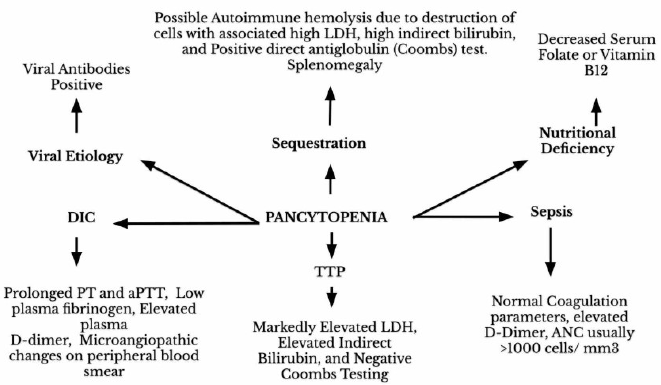
Figure 1. Diagnostic approach for patients presenting with pancytopenia of unknown etiology. HIV: Human Immunodeficiency Virus; CMV: Cytomegalovirus; EBV: Epstein-Barr Virus; HBV: Hepatitis B Virus; HCV: Hepattits C Virus (Adapted from Rodak’s Hematology 5th Edition) [6].
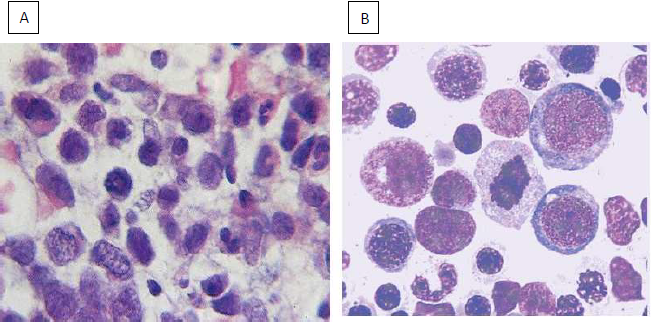
Figure 2. LDH: Lactate Dehydrogenase; TTP: Thrombotic Thrombocytopenic Pupura; aPTT: Activated Partial Thromboplastin Time; ANC: Absolute Neutrophil Count (Adapted from Rodak’s Hematology 5th Edition) [6].
As a large proportion of causes for pancytopenia are treatable and reversible, accurate diagnoses and timely intervention maybe lifesaving and will certainly have impact on the morbidity and mortality in these vulnerable patients. Knowing the exact etiology is thus important for specific and timely treatment and for prognostication [5].
A pre-designed proforma should be used to record history, examination details and investigation reports in a systematic manner. All patients should be thoroughly examined with special attention on history of prior drug intake, exposure to chemical agents and radiation either by occupational, accidental or by medical treatment. History of recent viral infections, fever, weight loss, bleeding from various sites (gums, nose, mouth, vagina) should be noted. Dietary history in detail including on type of food, intake animal products e.g. meat milk, eggs should be taken. History of abdominal pain and bowel habits should be noted. History of previous blood transfusions should be noted. A detailed meticulous physical examination of every patient should be done for pallor, icterus, pedal oedema, mouth ulcers, hepatosplenomegaly, lymphadenopathy, sternal tenderness, and gum hypertrophy should be done. Evidence of hypersplenism and primary malignancy should be searched wherever necessary [7].
The laboratory analysis includes Complete Blood Count (CBC) with absolute values should be conducted on an automated blood analyzer. All hematological parameters should be obtained. Values of hemoglobin, red blood cell count, total leucocyte count, differential leucocyte count, platelet count, Mean Corpuscular Volume (MCV), Mean Corpuscular Hemoglobin (MCH), Mean Corpuscular Hemoglobin Concentration (MCHC), Packed Cell Volume (PCV) and reticulocyte count should be noted and analyzed [8].
Peripheral blood smear examination should be done systematically under low, high and oil immersion microscope for RBC morphology i.e., microcytosis, macrocytosis, anisocytosis, poikilocytosis, polychromasia, nucleated red blood cells and presence of inclusions. Differential leucocyte count should be done. Neutrophils should be studied in detail for defective granulation and hyper segmentation. Platelet count and morphology should be analyzed. Bone marrow aspiration studies along with trephine biopsy should be done wherever indicated from anterior superior iliac spine using standard methods and under all aseptic precautions after obtaining written consent from the patient or guardian. The bone marrow aspiration smears and the biopsy sections should be studied in detail. As and when required, bone marrow aspiration and bone marrow biopsy slides should be stained with Perl’s stain, periodic acid Schiff stain, Zeihl– Neelsen stain or Reticulin stain [9].
Iron profile (serum iron and ferritin), serum folic acid and serum vitamin B12 level should be done in all cases.
Figure 3. (A) Megaloblasts- Bone marrow aspiration. (B) Megaloblasts-Trephine biopsy.
|
Condition |
Peripheral Blood |
Bone Marrow |
Laboratory Test Results |
Clinical Findings |
|---|---|---|---|---|
|
Failure of Bone Marrow to Produce Blood Cells |
||||
|
Aplastic Cinema |
No immature WBCs or RBCs; ↓reticulocytes; MCV ↑ or normal |
Hypocellular; blasts and abnormal cells absent; reticulin normal; RBC dyspoiesis may be present; WBC and platelet dyspoiesis absent |
Acquired: PNH cells* may be present; chromosome abnormalities may be present |
Splenomegaly absent |
|
Increased Destruction of Blood Cells |
||||
|
PNH |
Reticulocytes ↑; MCV normal or ↑; nucleated RBCs present or absent |
Erythroid hyperplasia; may be hypocellular |
PNH cells* present; hemoglobinuria +/-; chromosome abnormalities may be present |
Splenomegaly absent; thrombosis may be present |
|
Ineffective Hematopoiesis |
||||
|
Myelodysplastic Syndrome |
Variable pancytopenia; reticulocytes ↓; MCV normal or ↑; blasts and abnormal WBCs RBCs and platelets may be present |
Hypercellular; 20% of cases hypocellular; dyspoiesis in one or more cell lines present; blasts and immature cells present; reticulin ↑ |
Chromosome abnormalities usually present |
Splenomegaly uncommon |
|
Megaloblastic anemias |
MCV ↑; oval macrocytes; hypersegmented neutrophils |
Hypercellular with megaloblastic features |
Serum vitamin B12 or folate or both ↓ |
Splenomegaly absent |
|
Bone Marrow Infiltration |
||||
|
Acute leukemia |
Blasts present |
Hypercellular; blasts ↑ reticulin ↑ |
Chromosome abnormalities may be present |
Splenomegaly may be present |
|
Hairy cell leukemia |
Hairy cells present; monocytes ↓ |
Hairy cells and fibrosis present; reticulin ↑ |
Hairy cells* present; TRAP + |
Splenomegaly present (60-70% of cases) |
|
↑ Increased: ↓ decreased: + positive result: +/- positive or negative result: MCV mean cell volume; PNH paroxysmal nocturnal hemoglobinuria: RBC red blood cell: TRAP tartrate-resistant acid phosphatase: WBC white blood cell. *PNH erythrocytes are detected by flow cytometry by their lack of expression of CD59: PNH granulocytes and monocytes lack expression of CD24 CD16 and CD14 (Chapter 24). *Hairy cells are detected by flow cytometry by their expression of CD19 CD20 CD22 CD11c CD25 CD103 and FMC7. |
||||
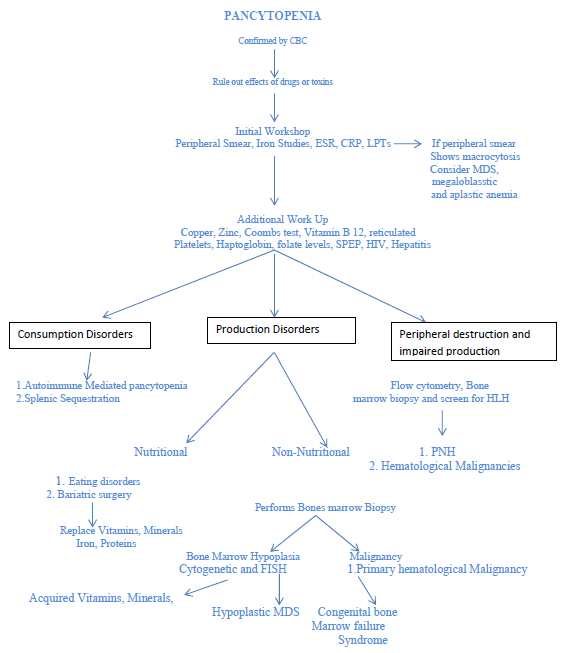
Figure 4. Diagnostic logarithm for evaluation of Pancytopenia. (adopted from Gannaraj et al. [11]).
Other investigations should be performed as and when indicated which includes erythrocyte sedimentation rate, liver function tests, renal function tests, serological investigations for enteric fever, blood culture, ELISA for HIV, hepatitis B and C viruses and serum protein E electrophoresis. Urine examination including, urinary Bence Jones proteins and stool examination should be advised depending on the case. Chest and bone radiographs, abdominal and pelvis ultrasonography must be carried out. The investigative work up being directed by the pancytopenia profile developed by us and the suspected underlying pathology [10].
Conclusion
Pancytopenia is a common hematological entity encountered in our day to day clinical practice. This should put the physicians on high alert demanding further investigations to look for the possible cause. Since the underlying pathology determines the management and prognosis of these patients, identification of the cause is crucial. Pancytopenia and aplastic anaemia are not synonymous anymore as was thought earlier. There is a definite change in trend from aplastic to megaloblastic anaemia over the years. Megaloblastic anaemia is quite common in Indian population possibly due to nutritional factors and is easily reversible with appropriate treatment. Thus, megaloblastic anaemia should always be considered in the evaluation of pancytopenia in Indian and other Asian countries.
The evaluation of patient with pancytopenia requires a holistic approach and the proper identification of the underlying cause remains a challenge because of variable etiopathological factors and inheritable conditions. Recent advances in molecular pathology including genomic profiling and next generation sequencing has great potential in providing cost effective diagnostic options in such cases and needs to be explored with proper emphasis [11].
References
2. Gayathri BN, Rao KS. Pancytopenia: a clinico hematological study. Journal of Laboratory Physicians. 2011 Jan;3(1):15-20.
3. Varma N, Dash S. A reappraisal of underlying pathology in adult patients presenting with pancytopenia. Tropical and Geographical Medicine. 1992 Oct;44(4):322-7.
4. Raphael V, Khonglah Y, Dey B, Gogoi P, Bhuyan A. Pancytopenia: an etiological profile. Turkish Journal of Hematology. 2012 Mar;29(1):80-1.
5. Khunger JM, Arulselvi S, Sharma U, Ranga S, Talib VH. Pancytopenia--a clinico haematological study of 200 cases. Indian Journal of Pathology & Microbiology. 2002 Jul;45(3):375-9.
6. Mahapatra M. Pancytopenia; aplastic anemia. In: Saxena R, Pati HP, Mahapatra M, editors. de Gruchy’s Clinical Hematology in Medical Practice. 6th Adapted Edition. Greater Noida: Wiley India Pvt. Ltd. 2013; pg.106- 19.
7. Makheja KD, Maheshwari BK, Arain S, Kumar S, Kumari S. The common causes leading to pancytopenia in patients presenting to tertiary care hospital. Pakistan Journal of Medical Sciences. 2013 Sep;29(5):1108-11.
8. Pathak R, Jha A, Sayami G. Evaluation of bone marrow in patients with pancytopenia. Journal of Pathology of Nepal. 2012 Sep 25;2(4):265-71.
9. Dasgupta S, Mandal PK, Chakrabarti S. Etiology of Pancytopenia: An observation from a referral medical institution of Eastern Region of India. Journal of Laboratory Physicians. 2015 Jul;7(2):90-5.
10. Jain A, Naniwadekar M. An etiological reappraisal of pancytopenia-largest series reported to date from a single tertiary care teaching hospital. BMC Blood Disorders. 2013 Dec 1;13(1):10.
11. Gnanaraj J, Parnes A, Francis CW, Go RS, Takemoto CM, Hashmi SK. Approach to pancytopenia: Diagnostic algorithm for clinical hematologists. Blood Reviews. 2018 Sep 1;32(5):361-7.