Abstract
Introduction: Climate change presents an important threat to human health and wellbeing. Paradoxically, many facets of healthcare provision contribute significantly to greenhouse gas emissions. An important example of this is the use of single use, disposable orthopedic orthotics, widely dispensed in emergency departments and fracture clinics.
This study aimed to understand patients’ attitudes towards climate change, single use plastics, and recycling of orthotics.
Materials and methods: Fracture clinic patients wearing orthotics were invited to complete a questionnaire examining attitudes toward climate change and the recycling of orthotics. Questions explored patient attitudes towards climate change, single use plastics and re-use of orthotics. Free text was also included to identify any patient’s perceived concerns regarding brace re-use.
Results: 93 out of 211 patients in clinic wore orthoses (44.1%). 40 completed the questionnaire giving a 43% response rate. 95% of patients were aware of climate change, attributing an average importance of 7.7 on a Likert scale of 0 (least important) to 10 (most important). 92.5% understood the issue of single use plastics, ascribing an average score of 8 to this. 90% of patients were willing to recycle their orthosis, with 90% also willing to use a recycled orthosis. Free text analysis revealed concerns with infection and brace integrity.
Conclusions: Orthopedic trauma patients recognize the danger of climate change and welcome efforts to address the issue of single use plastic in orthoses by recycling braces. Further research is required to facilitate the production of reusable orthoses and the reprocessing of current orthoses.
Keywords
Recycling, Recycling orthotics, Orthopedic outpatients, Fracture clinic
Introduction
Climate change has been described by the Lancet as the “biggest global risk to human health in the 21st Century” [1] with over 800 million people worldwide likely to be directly affected by its impact. Paradoxically, healthcare and its provision contribute enormously to climate change from the use of single use plastics, the production, and distribution of medication to personal transport of healthcare staff [2]. The British National Health Service creates 133,000 tons of plastic annually, only 5% of this is able to be recycled [3].
Surgery may be a notable culprit. Rizan et al. [4] examined the carbon footprint of surgical operations, discovering 814 kg of carbon dioxide equivalents can be generated per procedure. The literature examining the subject of plastic waste in orthopedics focuses on the waste generated in the operating theatre [2,5,6]. Operating theatres may generate up to 70% of hospital waste with 26% of waste by weight being plastic [7]. A recent literature review by Phoon et al. suggests that up to 43.9% of waste generated in orthopedic procedures may be recyclable [8].
Few studies have investigated the impact of single use plastics in the outpatient setting, whilst those that have concluded that the environmental waste outweighs any realized benefits [9,10]. No studies have specifically examined the outpatient orthopedic population.
Single use items are abundant in surgical treatment but also in non-surgical treatment in orthopedics. Further to this, these are wrapped in multiple layers of non-recyclable plastic packaging. Vast amounts of patients in trauma and orthopedics are managed with single use orthopedic braces. These are often made of plastic and fabric components. The rigid components of orthotic braces are typically composed of thermoplastics such as polypropylene or carbon fiber [11]. These components are also recyclable.
There is a clear need to reduce plastic waste in Orthopedics, and across all surgical specialties. This change in behavior required the appropriate mindset of those involved. The aim of our study was to examine attitudes of fracture clinic outpatients towards climate change, single-use plastics, and recycling.
Materials and Methods
A custom questionnaire was created (Appendix 1) to examine patient attitudes towards the issues of climate change, single use plastics, and the re-use of orthopedic braces. A Likert scale was utilized grading this from 0-10 with 10 indicating highest importance and 0 being lowest importance. Similarly, thoughts on re-using orthoses were graded on a 4-point Likert scale from ‘strongly agree, to strongly disagree’. Patient potential drawbacks to orthoses were also examined in the same manner. Free text was provided for qualitative feedback.
Data was collected prospectively in fracture clinics using questionnaires. All patients with orthopedic braces were offered a questionnaire. The questionnaire collected demographic details and assessed patient awareness of climate change and single use plastics.
Inclusion criteria were all patients wearing orthoses who attended fracture clinic. Patients under 16 years of age and those not wearing braces were excluded.
The questionnaire was conducted on a voluntary basis, following the decision for treatment, and was not deemed to influence the management plans nor confound patient responses. The study was thus approved by the ethics committee of our institution.
Results
Data was collected from fracture clinics over a 2-week period. 211 patients attended, 93 of which were using orthopedic braces (44.1%). 40 responses were received in total, a response rate of 43%.
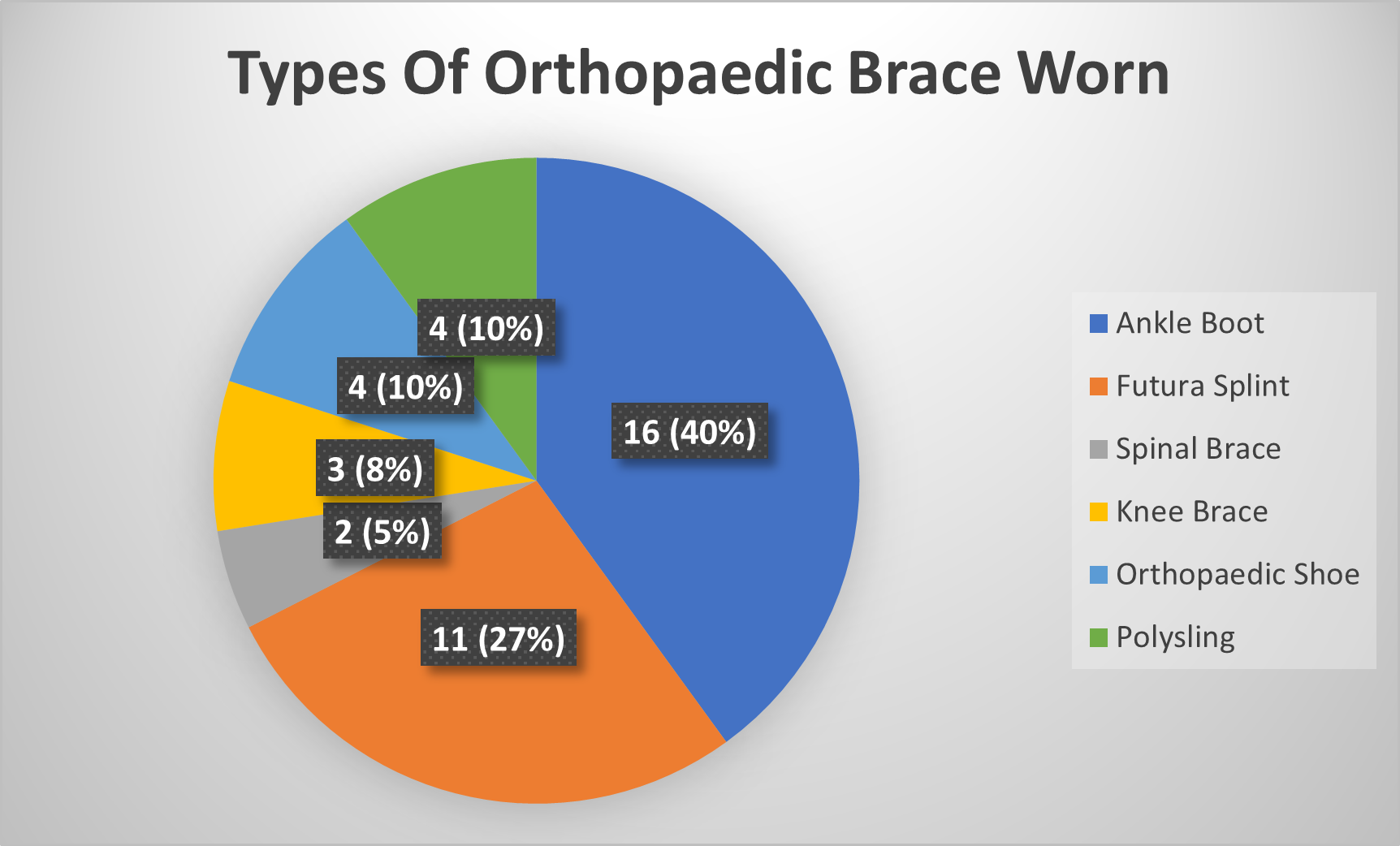
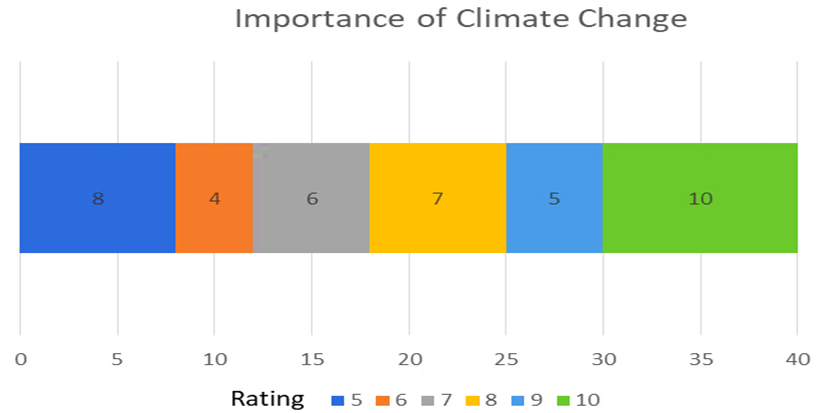
52% of patients were male with a mean age of 49 (16-82). The most common types of orthotics utilized are shown in Figure 1. The most common orthotic amongst responders was an ankle boot at 40%, followed by Futura (wrist) splints at 27%. The rest are shown in the chart making up a third of all orthoses worn. The next part of the questionnaire assessed the importance patients gave to key issues surrounding climate change and recycling. Firstly, we assessed how important climate change was to our patients (shown in Figure 2 below) Likert scale data showed that patients found climate change to be a relatively important issue, scores averaged 7.7 (range 5-10) with the majority of patients giving a score of 10.
Figure 1. Pie chart showing types of Orthopedic Brace Worn.
Figure 2. Cumulative bar chart showing patient perceived importance of climate change.
38 out of 40 (95%) patients were aware of climate change, with 37 understanding the issue of single use plastics (92.5%).
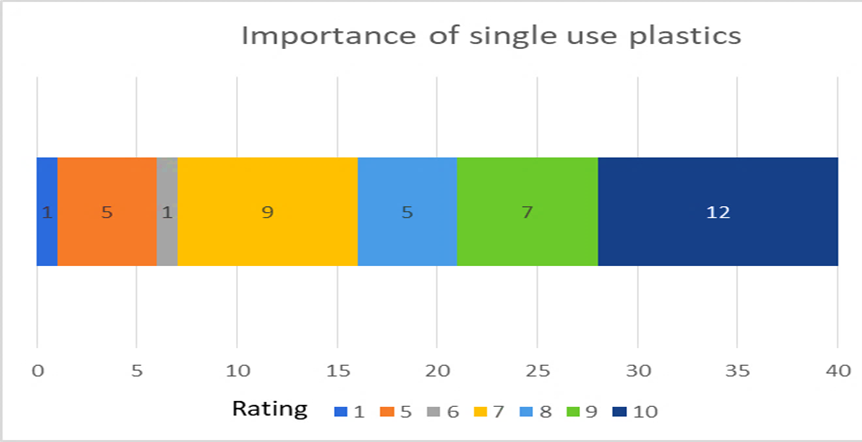
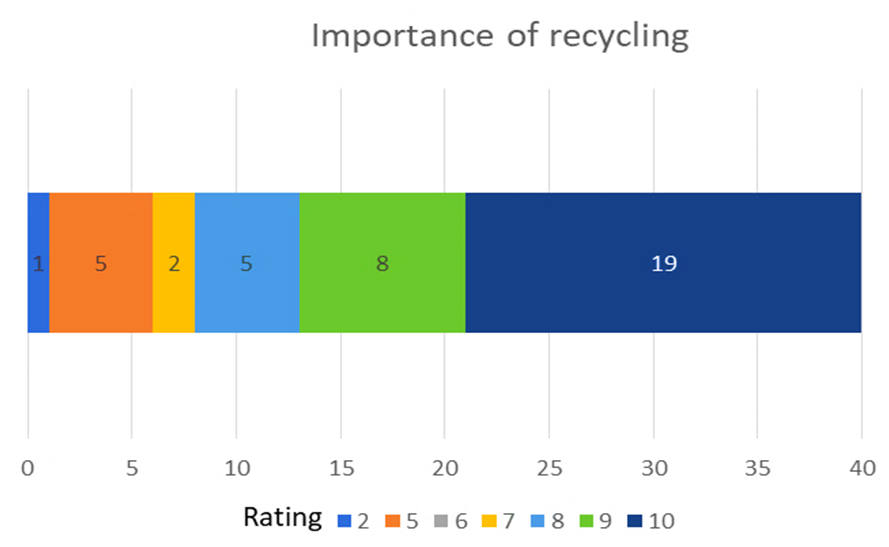
Further Likert scale data was obtained to assess patient assigned importance of single use plastics (Figure 3) and recycling (Figure 4).
Figure 3. Cumulative bar chart showing patient perceived importance of single use plastics.
Figure 4. Cumulative bar chart showing patient perceived importance of recycling.
Most patients attributed high importance to the issue of single use plastics. The mean rating was 8 (range 1 to 10) with the most common response being 10.
Similarly, most patients assigned a high importance to recycling. The most common response was 10 with a mean rating of 8.6 (range 2-10).
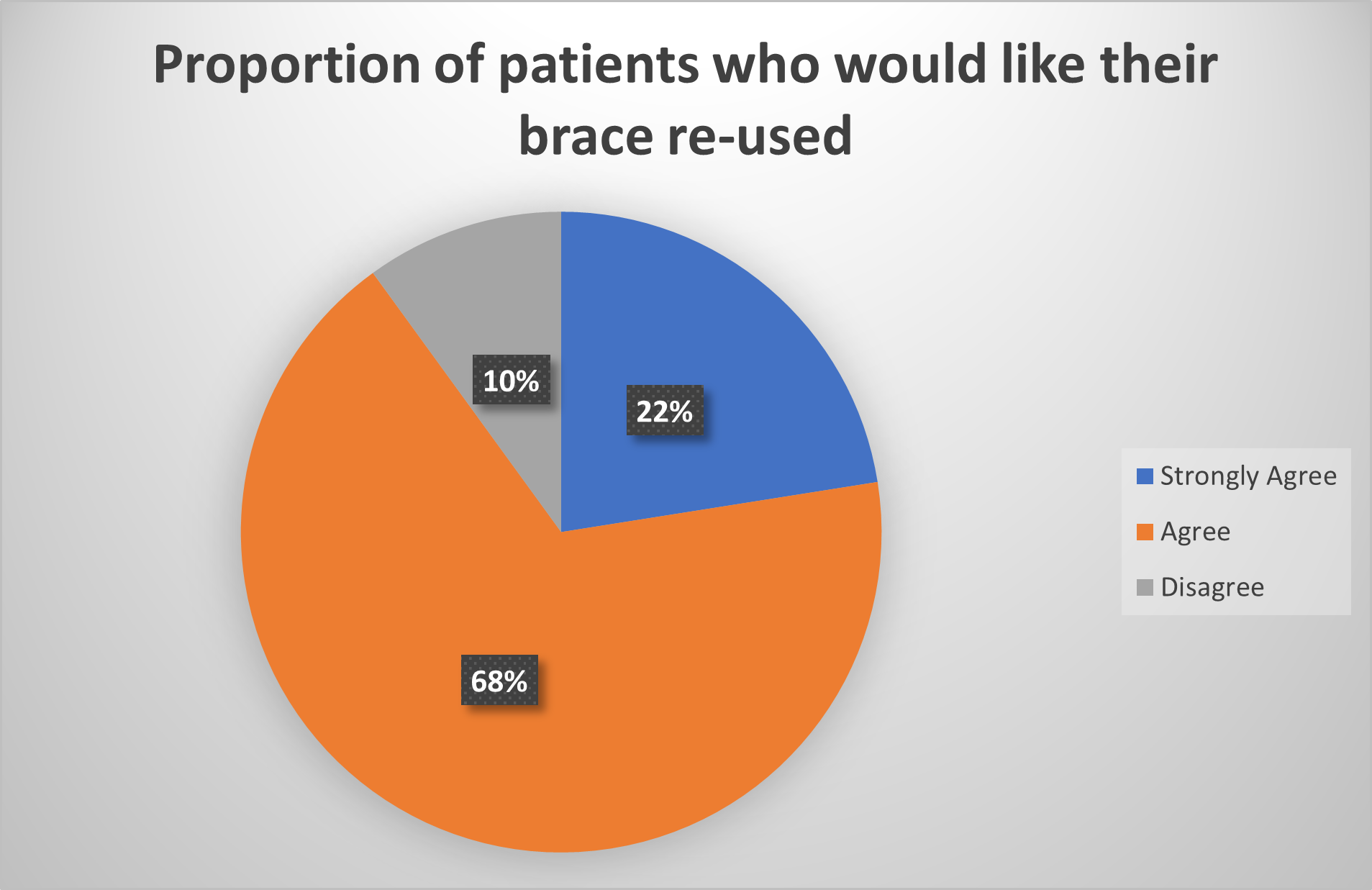
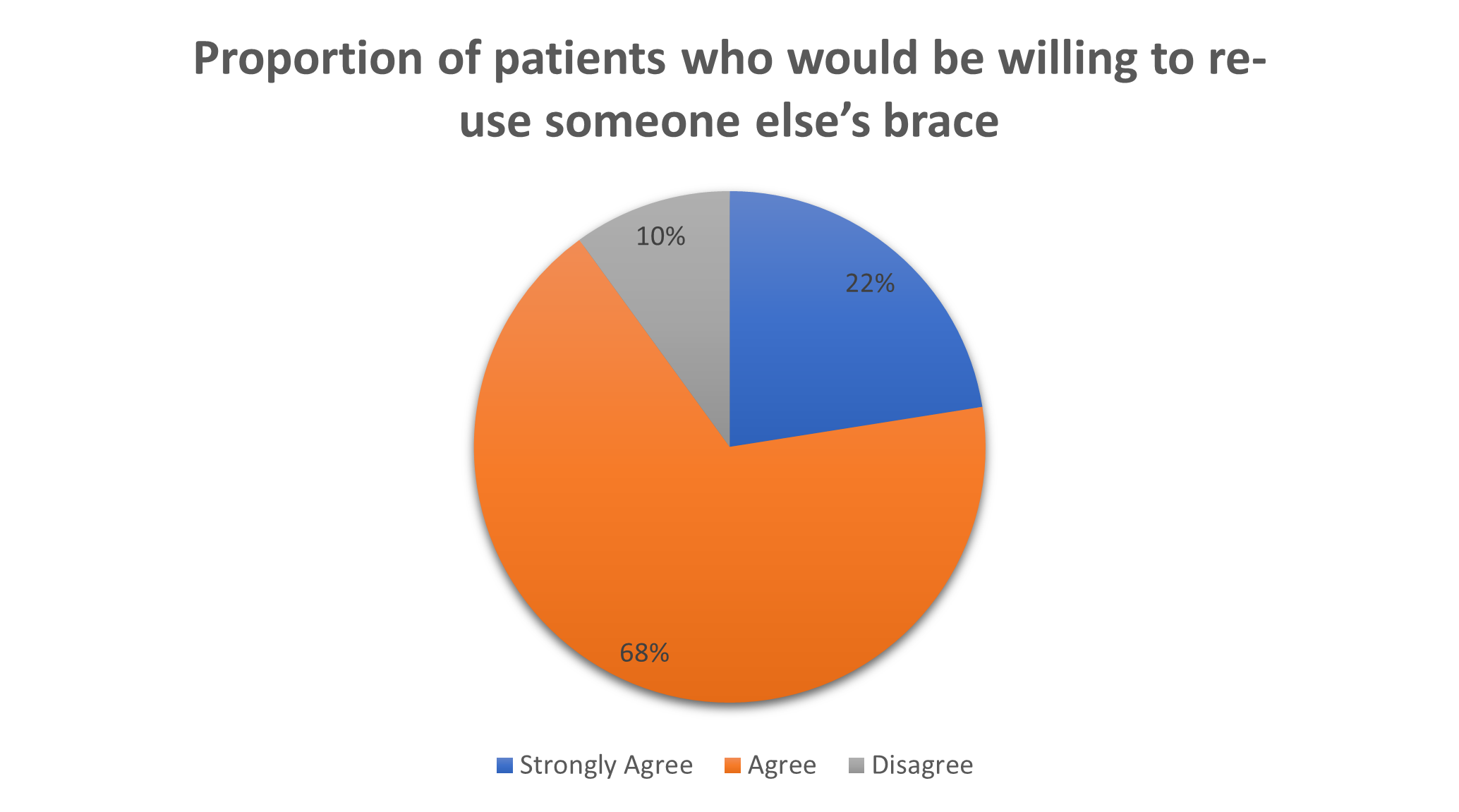
We then assessed patient attitudes towards re-use of orthotics. Firstly, we asked them to rate the statement: ‘I would like my brace to be re-used’ on a Likert scale. Results shown in the pie chart indicate 90% agreement to some degree (Figure 5). Similarly, we asked whether patients would be happy to re-use a previously used brace. 90% of patients reported that they were happy to use a recycled brace (Figure 6).
Figure 5. Pie chart showing patient attitudes towards re-use of their used brace.
Figure 6. Pie chart showing patient attitudes towards re-using a previously used brace.
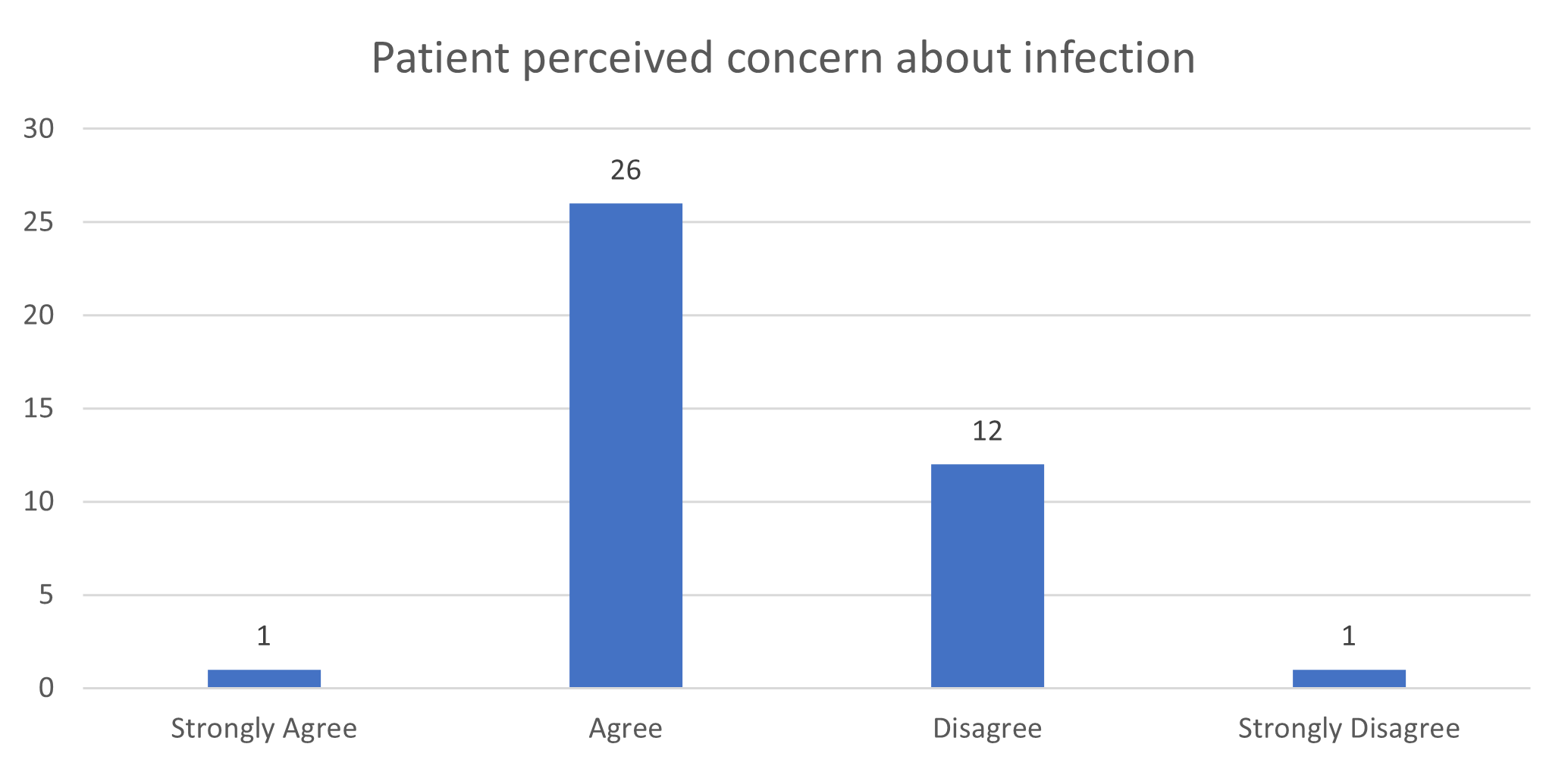
We then assessed patient perceived barriers to brace re-use on a similar scale, shown in bar charts below (Figures 7 and 8). 67.5% of patients agreed to some degree that infection would be a concern with brace re-use.
Figure 7. Bar chart showing whether patients perceive infection as a barrier to brace re-use.
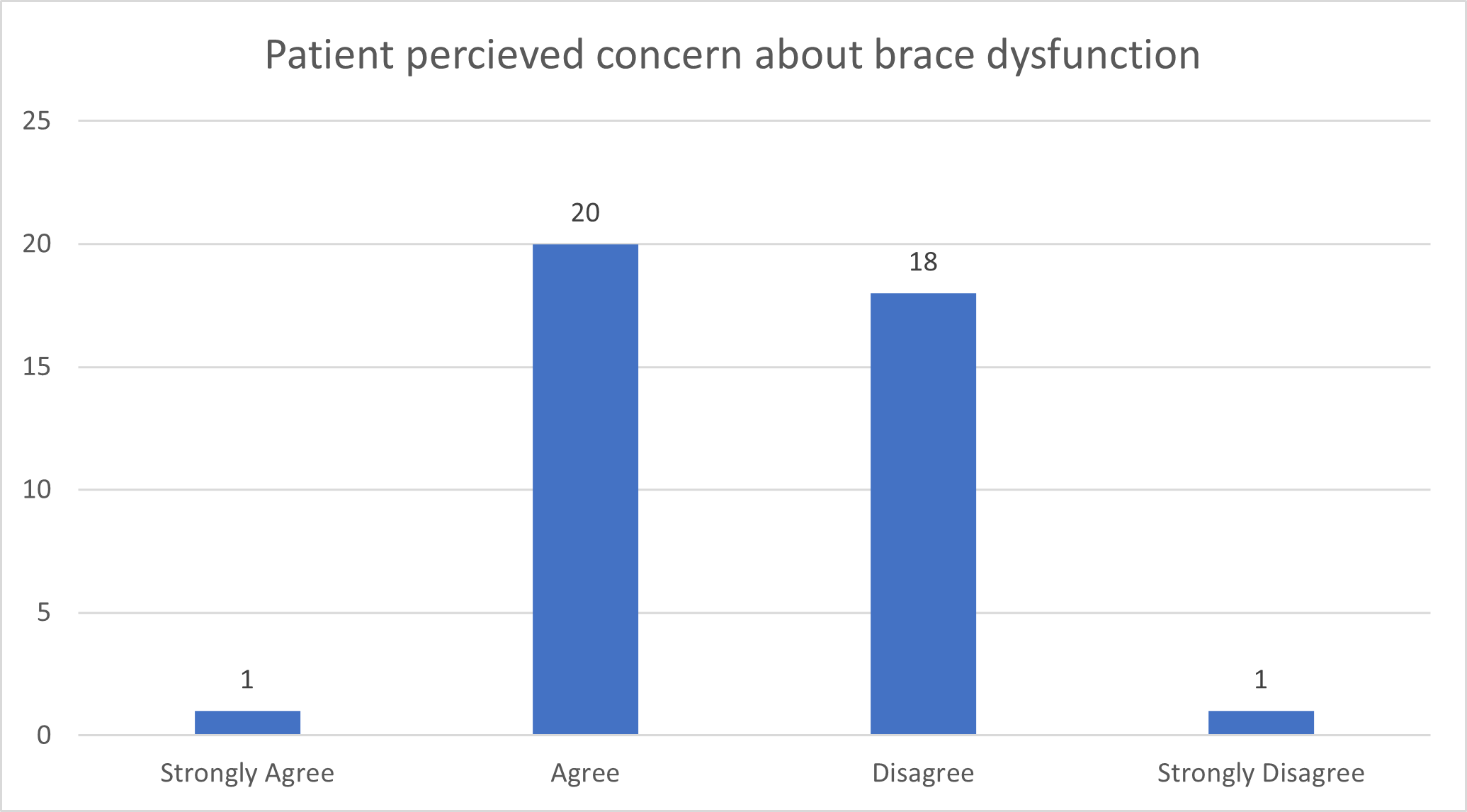
Figure 8. Bar chart showing whether patients perceive dysfunction as a barrier to brace re-use.
The next question pertained to brace integrity, around 52.5% of patients felt that brace dysfunction would be a concern with brace re-use.
Finally, we examined the free space responses using an inductive approach. The recurring theme for those who commented were that they would re-use an orthotic if they could be satisfied that it could be cleaned appropriately. One response indicated that they would want the integrity of the orthotic to be monitored for subsequent uses.
Discussion
Our study demonstrates strong patient support for a strategy of re-use or recycling of orthotics.
Despite the overall positive response, some concerns remained. The main apprehensions regarding a re-use strategy were infection and orthotic dysfunction with 68% being concerned about the possibility of cross infection. This mirrors work by the Association of Surgeons of Great Britain and Ireland, which suggested that 60% of patients fear the possibility of cross infection from a reusable product [12]. There is paucity of evidence in the literature that proves infection is transmitted between braces. Leichsenring et al. [13] demonstrated absent organic material present on cardiac catheters after application of a sterilization protocol, suggesting the catheters are safe for re-use with regards to infection. Similar protocols may be applicable to orthotics.
If orthoses are to be re-used, then appropriate sterilization processes will be required. The Spaulding classification [14], qualifies the level of decontamination required for different medical devices. Most orthopedic braces would be classified as low or intermediate risk. The WHO has published generalized guidelines on sterilization and re-use of medical devices [15], however more specific guidelines based on manufacturer recommendations would be required for each trust.
There are recent examples of positive advances regarding sustainability in orthotics. The Orthotics department at Oxford University Hospitals have demonstrated successful re-use of steel from braces leading to an 80% reduction in steel as well as well as 78% reduction in spend, whilst also recycling more than 3.5 tons of thermoplastic since 2018 [16]. Elsewhere, Shiyo et al. [17] described a process of re-use of Plaster of Paris (POP), concluding that POP could be recycled continuously. Such a process would have obvious benefits in fracture clinics. Economic factors such as cost saving and waste reduction need to be demonstrated with a re-use strategy to make them attractive to patients and healthcare providers.
The principles of sustainability in healthcare are gradually gaining traction [18]. The UK legislature via the Health and Care Act 2022 has committed the National Health Service (NHS) to delivering a ‘net zero NHS’. The aim is to cut carbon emissions to a level matching output of emissions by 2045, with the preliminary target of 80% reduction by 2032 [19].
Surgical bodies have also responded to climate change with the Royal College of Surgeons (RCS) of England devising a ‘Sustainability in Surgery’ strategy [20]. The strategy promotes the benefit of re-usable rather than single use items thereby reducing environmental impact. The published document highlights the importance of repair, the reduction of plastic packaging waste and re-use of instruments whilst censuring single use items. This has been reiterated by the Association of Surgeons of Great Britain and RCS Ireland emphasizing the importance of reduction, re-use, and recycling in theatre amongst other steps [12].
Internationally, Healthcare Without Harm Europe (HWHE), a multinational organization, with 137 members in over 22 European countries work on initiatives encouraging more sustainable procurement practices, greener medicine production as well as accurate carbon emission measurements amongst others. The HWHE report “Measuring and Reducing Plastic in the Healthcare Sector” identified prevention of waste generation as key to reducing waste generation. The steps included reduction, re-use, reprocessing and repair of materials as key. Although the report does not highlight any examples from orthopedics, it gives the example of the re-use of linear suture machines and harmonic shears in Portugal, leading to a cost saving of 90,000 Euros, with the machines achieving the same clinical results [21].
The literature which concerns orthopedics and sustainability, mainly examines the production of peri-operative waste, De Sa investigated 5 hip arthroscopies for femora-acetabular impingement, discovered an average of 9.4 kg waste per case [22] whilst a similar study of 5 primary total knee arthroplasties noted an average of 13.3 kg [4]. Kooner evaluated 55 procedures in orthopedics, concluding that up to three quarters of plastic waste from orthopedic theatres could be recycled and waste reduction strategies should be employed to encourage this [23]. Other strategies to encourage sustainability in orthopedics have included the WALANT (wide awake, local anesthetic, no tourniquet) technique in hand surgery which utilizes field sterility rather than theatre sterility in turn reducing theatre waste whilst the absence of anesthetic personnel involvement, reduces the carbon footprint [24].
Literature does not always support the use of reusable materials. The emissions generated in the sterilization process may in some circumstances exceed those of single use products [25,26]. Leiden et al. evaluated the environmental impact of reusable and single use instrumented lumbar fusion instrumentation. The initial detrimental environmental effect of the single use instrumentation was supplanted by the energy expended on steam sterilization [27].
Ethical considerations regarding re-use of medical devices have been discussed by both Collier [28] and Das [29]. Both authors examine the detriment to patient autonomy if patients are not aware of the use of reprocessed items. When giving patients options of treatment, all reasonable alternatives should be discussed to encourage patient centered decision making. This included the option to re-use braces. Thus, gauging patients’ understanding, and opinion is a vital first part of this process, which our study seeks to do.
The limitations of the study include a low response rate as well as a lack of inclusion of patients in elective orthopedic clinics or those not wearing an orthoses. There is also a relatively high likelihood of selection bias, those who are willing to complete a survey about the environment are also those most likely to be well informed about such matters.
Conclusion
This is the first study to have examined patient attitudes towards climate change and single use braces. Re-use strategies have been identified as crucial to address climate change by multiple bodies including the NHS, the RCS, and the BOA. Much literature already exists highlighting the role of surgeons in fighting climate change, however patient thoughts on sustainability in Orthopedics have been unknown, particularly in the outpatient setting.
Our results show most of our patients are aware of climate change, single use plastics and the importance of recycling. There is overwhelming support for the re-use of orthoses in the outpatient setting. Further work should aim to identify strategies that can be employed locally for recycling and re-use but there may also a role for industry using materials which can be more easily reprocessed and working to produce more environmentally sustainable products.
References
2. Beloeil H, Albaladejo P. Initiatives to broaden safety concerns in anaesthetic practice: The green operating room. Best Practice & Research Clinical Anaesthesiology. 2021;35(1):83-91.
3. https://nhsproviders.org/news-blogs/blogs/not-so-fantastic-plastic
4. Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta M. The Carbon Footprint of Surgical Operations. Annals of Surgery. 2020;272(6):986-95.
5. Stall N, Kagoma Y, Bondy J, Naudie D. Surgical waste audit of 5 total knee arthroplasties. Canadian Journal of Surgery. 2013;56(2):97-102.
6. Hennessy O, Devitt A. AB158. An analysis of implant related waste in the Trauma and Orthopaedics Department of Galway University Hospital. Mesentery and Peritoneum. 2020;4:AB158-AB158. Accessed 17/11/2023 at: https://map.amegroups.org/article/view/5463/html
7. Doyle F, Mulrain J, Rowan F. AB124. 77. The current state of plastic waste in the orthopaedic operating theatre. Mesentery and Peritoneum. 2019;3:AB124-AB124. Accessed 17/11/2023 at: https://map.amegroups.org/article/view/4810/html
8. Phoon KM, Afzal I, Sochart DH, Asopa V, Gikas P, Kader D. Environmental sustainability in orthopaedic surgery. Bone Jt Open. 2022 Aug 1;3(8):628-40.
9. Farrell E, Smyth D. The environmental impact of personal protective equipment in a pre and post COVID era in the ENT clinic. European Archives of Oto-Rhino-Laryngology. 2021;278(12):5051-58.
10. Park E, LaMattina K. Economic and Environmental Impact of Single-use Plastics at a Large Ophthalmology Outpatient Service. Journal of Glaucoma. 2020;29(12):1179-83.
11. Berry D. Composite Materials for Orthotics and Prosthetics. Orthotics and Prosthetics. 1987;40(4):35-43.
12. Statement on Sustainability in Surgery [Internet]. Asgbi.org.uk. 2012 [cited 9 August 2022]. Available from: https://www.asgbi.org.uk/userfiles/file/consensus/asgbi_consensus_statement_on_cost-effective_surgery.pdf
13. Leichsenring ML, Psaltikidis EM, de Oliveira Figueiredo MJ, Moretti ML, Trabasso P. Conception and validation of a protocol for reuse of non-irrigated electrophysiology catheters in a Brazilian teaching hospital. Journal of Interventional Cardiac Electrophysiology. 2017;51(1):45-50.
14. Rowan NJ, Kremer T, McDonnell G. A review of Spaulding's classification system for effective cleaning, disinfection and sterilization of reusable medical devices: Viewed through a modern-day lens that will inform and enable future sustainability. Science of The Total Environment. 2023;878:162976.
15. Decontamination and reprocessing of medical devices for health care facilities: aide-memoire [Internet]. www.who.int. Available from: https://www.who.int/publications/i/item/WHO-UHL-IHS-IPC-2022.4
16. Trust C. Reduce, Reuse, Recycle: Orthotics team helping create a greener OUH - Oxford University Hospitals [Internet]. Ouh.nhs.uk. 2022 [cited 12 September 2022]. Available from: https://www.ouh.nhs.uk/news/article.aspx?id=1660&returnurl=/default.aspx&pi=0
17. Shiyo S, Nagels J, Shangali H. Recycling of plaster of Paris. African Journal of Disability. 2020;9.
18. Press Release: A Zero Waste hierarchy for Europe - Zero Waste Europe [Internet]. Zero Waste Europe. 2022 [cited 12 September 2022]. Available from: https://zerowasteeurope.eu/press-release/press-release-a-zero-waste-hierarchy-for-europe
19. NHS G. Greener NHS » Delivering a net zero NHS [Internet]. England.nhs.uk. 2022 [cited 15 August 2022]. Available from: https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/
20. Sustainability in Surgery — Royal College of Surgeons [Internet]. Royal College of Surgeons. 2021 [cited 9 August 2022].: https://www.rcseng.ac.uk/about-the-rcs/about-our-mission/sustainability-in-surgery/
21. Pages 51-58 [Internet]. Noharm-europe.org. 2022 [cited 9 August 2022]. Available from: https://noharm-europe.org/sites/default/files/documents-files/6886/2021-09-23-measuring-and-reducing-plastics-in-the-healthcare-sector.pdf
22. De Sa D, Stephens K, Kuang M, Simunovic N, Karlsson J, Ayeni OR: The direct environmental impact of hip arthroscopy for femoroacetabular impingement: A surgical waste audit of five cases. J Hip Preserv Surg 2016;3:132-7.
23. Kooner S, Hewison C, Sridharan S, Lui J, Matthewson G, Johal H, et al. Waste and recycling among orthopedic subspecialties. Canadian Journal of Surgery. 2020;63(3):E278-83.
24. Shahid S, Saghir N, Saghir R, Young-Sing Q, Miranda BH. WALANT: A Discussion of Indications, Impact, and Educational Requirements. Archives of Plastic Surgery. 2022;49(4):531.
25. Davis NF, McGrath S, Quinlan M, Jack G, Lawrentschuk N, Bolton DM. Carbon Footprint in Flexible Ureteroscopy: A Comparative Study on the Environmental Impact of Reusable and Single-Use Ureteroscopes. Journal of Endourology. 2018 Mar;32(3):214-7.
26. McGain F, McAlister S, McGavin A, Story D. A Life Cycle Assessment of Reusable and Single-Use Central Venous Catheter Insertion Kits. Anesthesia & Analgesia. 2012 May;114(5):1073-80.
27. Leiden A, Cerdas F, Noriega D, Beyerlein J, Herrmann C: Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries. Resourc Conserv Recycl 2020;156:104704.
28. Collier R. The ethics of reusing single-use devices. Canadian Medical Association Journal. 2011 Jul 11;183(11):1245-5.
29. Das AK, Okita T, Enzo A, Asai A. The Ethics of the Reuse of Disposable Medical Supplies. Asian Bioethics Review. 2020 Apr 12;12(2):103-16.