Abstract
Introduction: Skull, rib, corner fractures, and fractures in children who have not started walking are highly associated with abuse. The majority of fractures stemming from abuse occur in children less than two years of age. The purpose of this study is to determine the etiology and relationship of displaced supracondylar elbow fractures with child abuse.
Materials and Methods: Seventy-five displaced supracondylar elbow fractures were reviewed to determine how the injury occurred. Medical records and radiographs were analyzed for demographics, cause of injury, age of injury, injury data, and for the presence of a child abuse investigation. Transphyseal fractures were excluded.
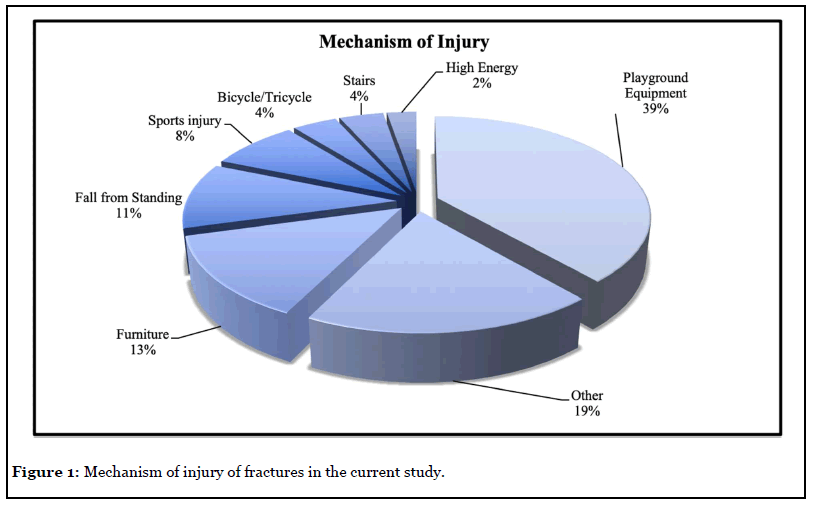
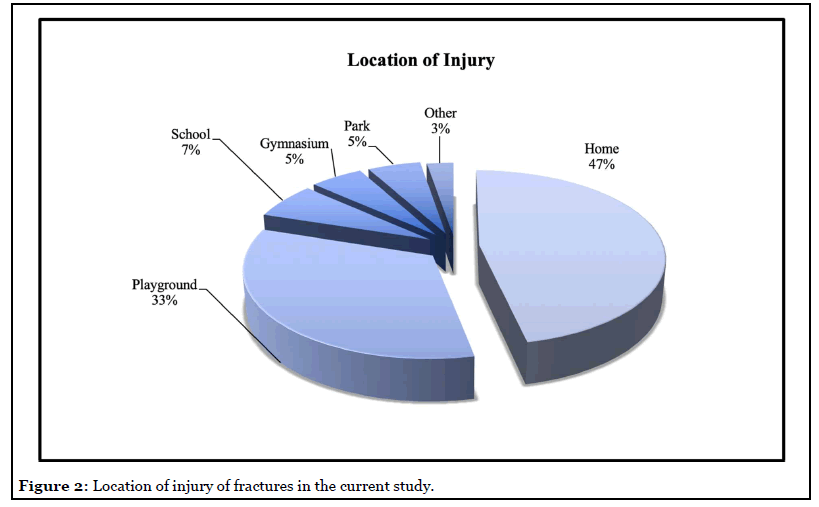
Results: Forty-two males (56%) and 33 females (44%) were studied. The average age was 6 years old (range: 1-year-5-months to 12-years-4-months). Two patients were 12 years of age, 3 were 23 years of age, and 70 were older than 3. All 75 were displaced supracondylar fractures. One fracture was open. All fractures stemmed from a reported accidental fall, including: falls from- -playground equipment 29 (39%), furniture 10 (13%), sports 6 (8%), stairs 3 (4%), bikes 3 (4%), and miscellaneous: running, falling, sledding, tree, wagon, fence, bounce-house, van, deck, power-wheels car, ATV, and go-cart. Outside physicians, orthopaedic surgeons, emergency department physicians, residents, nurses, and technicians evaluated each patient. All of them are able to submit for an evaluation if they suspect abuse. Only 1 patient aged 1-year-5-months, injured from a reported fall at home during a tantrum, was reported for possible abuse. The child abuse evaluation was negative.
Discussion and Conclusion: Pediatric supracondylar fractures occur from accidental falls while children are at play. Most supracondylar fractures occur in children over the age of two. In the current series, 73 out of the 75 cases involved individuals that were two years of age or older. Child abuse is rarely associated with displaced supracondylar fractures in children.
Keywords
Pediatric Orthopaedics, Supracondylar, Abuse, Upper Extremity Trauma
Introduction
Supracondylar fractures of the humerus are the most common elbow fracture in the pediatric population and comprise nearly 60% of all elbow fractures [1-5]. Supracondylar fractures most commonly occur in children aged five to seven [1-7]. Historically, males had a higher incidence of supracondylar humeral fractures [7,8]. More recent studies support a more equal distribution amongst males and females. Three articles suggest supracondylar fractures are more common in females [6,8,9]. The most common mechanism of injury for this fracture is a fall on an outstretched hand [1,3,6,8]. The epidemiology of supracondylar fractures has evolved in recent years due to an increased incidence of childhood involvement in athletics and modern changes in playground equipment [10,11]. Between 1990 and 1994, playground equipment alone resulted in more than 200,000 injuries and 88% were attributable to falling from monkey-bars, jungle gyms, swings, and slides [12]. The primary aim of this study was to investigate if child abuse is a common mechanism leading to displaced supracondylar fractures.
Methods
The College of Medicine Institutional Review Board (IRB) approved this study. The electronic medical records (EMR) and radiographs for all patients who underwent operative fixation of supracondylar humeral fractures from 2010-2014 were analyzed by the senior author. Seventy-five consecutive displaced supracondylar elbow fractures were reviewed to determine specific information about the manner in which the injury occurred. Data elements recorded from the EMR included patient date of birth, gender, height, weight, handedness, date, time, location, mechanism, and physical exam findings including associated fractures, concurrent injuries, and neurovascular status (Tables 1 and 2). Other parameters collected included date, time, length of surgery, range of motion, including hyper-extensibility, and carrying angle of the contralateral upper extremity. Finally, the medical record was analyzed for evidence of a report of child abuse by any member of the child’s medical care team. The inclusion criteria for this study included patients less than 13 years of age at the time of sustaining a supracondylar fracture. Exclusion criteria included patients greater than or equal to 13 years of age at the time of surgery, nondisplaced fractures that were treated with a cast or splint, and transphyseal fractures.
| Patient Characteristics | |
|---|---|
| Male | 42 (56.0%) |
| Female | 33 (44.0%) |
| Avg. Age at Time of Fracture | 6y, 2mo (ly, Smo — 12y, 4mo) |
| Right-Hand Dominant | 65 (86.7%) |
| Left-Hand Dominant | 7 (9.3%) |
| Handedness Not Documented | 3 (4.0%) |
| Avg. Height (cm) | 115.5 |
| Avg. Weight (kg) | 22.7 |
Table 1: General patient characteristics for children with supracondylar fractures.
| Presenting Complications | |
|---|---|
| Pucker Sign | 9 (12%) |
| Compartment Syndrome | 0 (0%) |
| Nerve Injury | 7 (9%) |
| Vascular Injury | 4 (5.3%) |
| Additional Fractures | 7 (9%) |
Table 2:Supracondylar associated findings.
Results
Seventy-five patients met inclusion criteria. Forty-two males (56%) and thirty-three females (44%) were studied. The average age was six years and two months with a range of 1-year-5-months to 12-years-4-months (Table 1). All patients in this study were independent ambulators at the time of fracture. Two patients were between the ages of one and two years, three were between ages two and three years, and seventy were older than three. The average height and weight were 115.5 cm and 22.7 kg, respectively. Fifty-nine (79%) patients were Caucasian, three (4%) were African American, four (5%) were mixed races, and nine (12%) were of unknown race. Sixty-five (87%) patients were right-hand dominant, seven (9%) were left hand dominant, and three (4%) were too young for handedness to be determined.
There were seventy-five displaced supracondylar fractures and eighty-seven total fractures in the cohort. Seven patients (9%) sustained twelve additional fractures. All seven patients suffered ipsilateral distal radial and/ or ulnar fractures, with complete displacement occurring in two patients all of which were ipsilateral distal radius fractures (Table 2). No patient suffered bilateral supracondylar elbow fractures. No patient sustained another fracture of another limb. One supracondylar elbow fracture was open. Nine (12%) patients had a pucker sign at the time of presentation. The pucker sign is a black and blue skin change directly over the supracondylar fracture. No patient had any additional skin bruises or traumatic lesions. Seven (9%) patients presented with an anterior interosseous nerve palsy and one presented with an additional ulnar nerve palsy. Four (5%) patients presented without a palpable radial pulse; all pulses were subsequently identified via Doppler ultrasound. No patient presented with, or developed, a compartment syndrome. The average contralateral elbow extension was -5°, average flexion was 135°, and the average contralateral carrying angle was 8°.
All seventy-five patients sustained a supracondylar elbow fracture stemming from a reported fall, including twentynine (39%) from playground equipment, ten (13%) from furniture, six (8%) while playing sports, three (4%) from falling down the stairs, and three (4%) from riding bicycles. The remaining twenty-four (32%) patients fell performing miscellaneous activities, including: running and tripping, falls from a toy ball, sled, tree, wagon, fence, bounce house, mini-van, deck, battery-powered ride-in car, all-terrain vehicle, and go-cart. The site of the fall was varied. Thirtyfive fractures (47%) occurred at the child’s home, thirty (40%) on school grounds, four (5%) in a gymnasium, four (5%) in a park, one at a farm show, and one in a parking lot (Figures 1 and 2).
Only 1 patient, the youngest patient in the cohort at 1-year-5-months, injured from a reported fall at home during a temper tantrum, was reported for possible abuse by the referring ED doctor. The SCAN (Suspected Child Abuse and Neglect) evaluation was negative. The remaining 74 patients were deemed accidental falls after evaluation by multiple medical professionals including nurses, residents, emergency department (ED) physicians, and orthopaedic surgeons.
Discussion
The average age of supracondylar fractures is six years [3,6,7,13,16]. Supracondylar fractures begin to occur in children after the age of one, and peak at the age of six. According to a report from the American Academy of Pediatrics, supracondylar fractures in ambulatory children are usually the result of a short fall [13]. To our knowledge, the relationship between displaced supracondylar fractures and child abuse has not been specifically studied. In our cohort, 73 of the 75 children with supracondylar fractures were older than two. Unless other evidence of abuse is present – such as multiple fractures, bruises, or an inconsistent history, a single fracture is unlikely the result of abuse in an ambulatory-age child [13-16]. In a non-ambulatory child less than two years of age with a supracondylar fracture, child abuse should be considered. In the current study, one out of two children less than the age of two sustained a supracondylar fracture that raised a concern for possible child abuse. In this case, the child abuse work-up and evaluation was negative.
Although a few studies have suggested that males no longer have a higher incidence of supracondylar fractures than females [6,8,9] our population demonstrated a slight male preponderance (56 vs 44%). Nearly 60% fractured their non-dominant arm; this is consistent with Farnsworth’s findings [6]. Neurovascular injury due to stretch neurapraxia has been shown to be more likely with greater fracture displacement [17,18]. In the current study, seven children sustained a neurological injury, and four sustained a vascular injury which is presented as a loss of radial pulse (Table 2). All seven of the neurological injuries recovered with 4 months of observation, and all of the vascular injuries resolved with reduction of the fracture. In the current study, nine children presented with a pucker sign. The pucker sign is a black and blue skin bruising in the ante-cubital fossa that results from bleeding about the fracture. The pucker sign is not an indicator of child abuse [19]. No additional skin bruising, or skin lesions were noted on any patient.
All patients in the current study demonstrated elbow hyperextension of the contralateral elbow averaging -5° supporting the relationship between ligamentous laxity and supracondylar elbow fractures [20,21]. Supracondylar elbow fractures occur largely from falls stemming from play equipment. Farnsworth reported that 29% of fractures stemmed from a fall from playground equipment, of which 61% were due to monkey bars [6]. The current study confirms Farnsworth’s findings: 38% of fractures occurred from a fall at the playground, of which 62% stemmed from a fall from the monkey bars. Falls from trampolines are also a common cause of supracondylar fractures [13]. In the current study, 10% of fractures resulted from a trampoline fall. Barr et al. reported that falls from furniture at home are the most common cause of supracondylar fractures in young children with an average age 4 years old [22]. The current study confirms these reports.
Although the presence of multiple fractures in different limbs is a red flag for child abuse, the combination of a supracondylar fracture with an ipsilateral distal radius fracture is not a red flag for child abuse. The findings of the current study and a review of literature demonstrate that supracondylar fractures following a fall can present with a second fracture in the same arm in approximately 10% of cases. About 50% of the additional fractures are distal radius fractures of the ipsilateral arm [6,7].
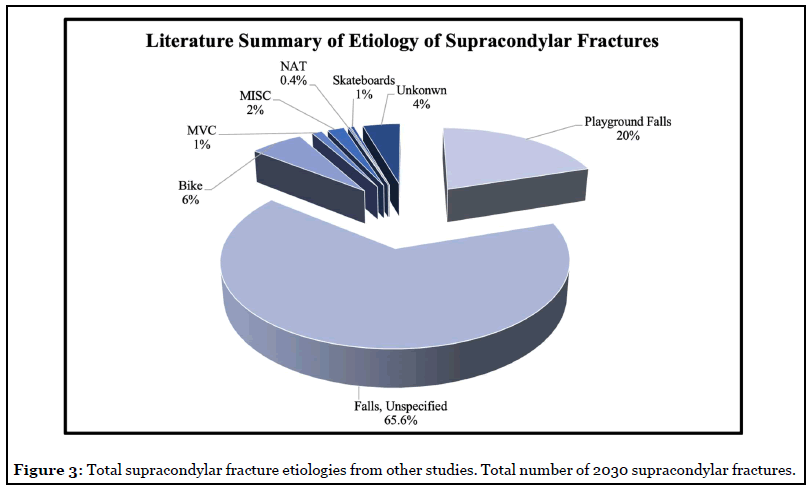
Supracondylar fractures following an act of child abuse are rare. We reviewed nine studies from six countries pertaining to supracondylar fractures. The studies included displaced supracondylar fractures from the US, UK, Mexico, Denmark, India, and China. Some 2,030 supracondylar fractures were reviewed. All the studies demonstrated a significant number of fractures resulting from playground falls [1,2,6-9,22-24]. Falls from low heights contributed the largest percentage of supracondylar fractures (Figure 3). Only eight cases (0.4%) out of 2,030 displaced supracondylar fractures were confirmed to be abuse [6,9,24].
The results of the current study and literature review demonstrate that a supracondylar fracture by itself should not be a red flag for abuse. Some factors helpful for identifying pediatric abuse include a non-ambulatory infant, multiple fractures, corner fractures, additional skin bruising, an inconsistent history, and a delayed presentation [13-16]. The limitations of this study included use of a single surgeon’s sample, the retrospective design, inclusion of only displaced fractures undergoing surgery, and small sample size.
Conclusion
Pediatric elbow supracondylar fractures occur from accidental falls while children are at play. The mechanism typically involves a fall on the outstretched hand and hyperextension of the elbow resulting in a fracture of the thin humeral cortex at the supracondylar location.
Conflict of Interest Statement
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Ethical Review Committee Statement
This study was an IRB approved study conducted at the Milton S. Hershey Penn State Medical Center. The approval document has been provided.
This study was conducted solely out of The Penn State College of Medicine at Milton S. Hershey Medical Center.
References
2. Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. Journal of Orthopaedic Science. 2001 Jul 1;6(4):312-5.
3. Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. Journal of Pediatric Orthopaedics. 1999 May 1;19(3):344-50.
4. Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. JBJS. 2008 May 1;90(5):1121-32.
5. Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 1997 Jan 1;5(1):19-26.
6. Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. Journal of Pediatric Orthopaedics. 1998 Jan 1;18(1):38-42.
7. Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. Journal of Pediatric Orthopaedics B. 2001 Jan 1;10(1):63-7.
8. Mitchelson AJ, Illingworth KD, Robinson BS, Elnimeiry KA, Wilson CJ, Markwell SJ, Gabriel KR, McGinty J, Saleh KJ. Patient demographics and risk factors in pediatric distal humeral supracondylar fractures. Orthopedics. 2013 Jun 1;36(6):e700-6.
9. Mehlman CT, Denning JR, McCarthy JJ, Fisher ML. Infantile Supracondylar Humeral Fractures (Patients Less Than Two Years of Age): Twice as Common in Females and a High Rate of Malunion with Lateral Column-Only Fixation. JBJS. 2019 Jan 2;101(1):25-34.
10. Miller MD, Thompson SR. DeLee & Drez’s Orthopaedic Sports Medicine E-Book. Elsevier Health Sciences; 2014 Apr 4.
11. Reynolds R, McKenzie S, Allender S, Brown K, Foulkes C. Systematic review of incidental physical activity community interventions. Preventive medicine. 2014 Oct 1;67:46-64.
12. Waltzman ML, Shannon M, Bowen AP, Bailey MC. Monkeybar injuries: complications of play. Pediatrics. 1999 May 1;103(5):e58.
13. Flaherty EG, Perez-Rossello JM, Levine MA, Hennrikus WL, American Academy of Pediatrics Committee on Child Abuse and Neglect. Evaluating children with fractures for child physical abuse. Pediatrics. 2014 Feb 1;133(2):e477- 89.
14. Schwend RM, Werth C, Johnston A. Femur shaft fractures in toddlers and young children: rarely from child abuse. Journal of Pediatric Orthopaedics. 2000 Jul 1;20(4):475-81.
15. Leaman LA, Hennrikus WL, Bresnahan JJ. Identifying non-accidental fractures in children aged< 2 years. Journal of Children’s Orthopaedics. 2016 Aug 1;10(4):335-41.
16. Rosado N, Ryznar E, Flaherty EG. Understanding humerus fractures in young children: Abuse or not abuse?. Child Abuse & Neglect. 2017 Nov 1;73:1-7.
17. Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: a meta-analysis. Journal of Pediatric Orthopaedics. 2010 Apr 1;30(3):253-63.
18. Campbell CC, Waters PM, Emans JB, Kasser JR, Millis MB. Neurovascular injury and displacement in type III supracondylar humerus fractures. Journal of Pediatric Orthopaedics. 1995 Jan 1;15(1):47-52.
19. Smuin DM, Hennrikus WL. The effect of the pucker sign on outcomes of type III extension supracondylar fractures in children. Journal of Pediatric Orthopaedics. 2017 Jun 1;37(4):e229-32.
20. Nork SE, Hennrikus WL, Loncarich DP, Gillingham BL, Lapinsky AS. Relationship between ligamentous laxity and the site of upper extremity fractures in children: extension supracondylar fracture versus distal forearm fracture. Journal of pediatric orthopedics. Part B. 1999 Apr;8(2):90-2.
21. Spencer HT, Wong M, Fong YJ, Penman A, Silva M. Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. JBJS. 2010 Apr 1;92(4):904-10.
22. Barr LV. Paediatric supracondylar humeral fractures: epidemiology, mechanisms and incidence during school holidays. Journal of children’s orthopaedics. 2014 Mar 1;8(2):167-70.
23. Barrón-Torres EA, Sánchez-Cruz JF, Cruz-Meléndez JR. Perfil clínico-epidemiológico de las fracturas supracondíleas de húmero en pacientes pediátricos en un hospital general regional. Cirugía y Cirujanos. 2015 Jan 1;83(1):29-34.
24. Pandya NK, Baldwin KD, Wolfgruber H, Drummond DS, Hosalkar HS. Humerus fractures in the pediatric population: an algorithm to identify abuse. Journal of Pediatric Orthopaedics B. 2010 Nov 1s;19(6):535-41.
