Abstract
Objective: Distal femoral fractures are a common orthopedic problem. The most used treatment is the fixation by lateral locking plates. The long plates offer greater biomechanical advantages, but there are no studies that analyze the influence of the length of the plate in the consolidation of the fracture.
The aim of the study was to identify the ratio plate length/fracture height as a predictor of non-union risk in less invasive stabilization system (LISS). As secondary goals, we studied patient comorbidities, fracture pattern and construct characteristics, and its relationship with the need for reintervention, infection, and implant failure.
Material and methods: Single-center retrospective case-control study of 59 patients with 64 distal femur fractures treated with LISS plates between 2007-2017. Consolidation group n=49, non-consolidation group n=15. Patient demographics (age and gender), comorbidities (obesity, diabetes and smoke habit), injury (tipe and mechanism) and construct characteristics (plate length, proximal and distal screws, proximal and distal holes and working length) were obtained for all participants. We measured the ratio between plate length and fracture height in the same anteroposterior X-ray.
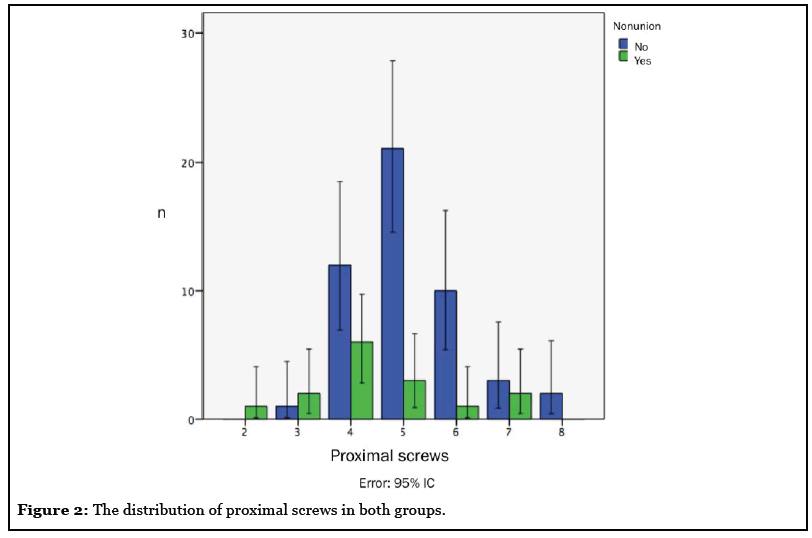
Results: No significant differences were found between the two groups in ratio plate length/fracture height. There were no statistically significant differences in demographic data, fracture pattern, plate length or working length. A relationship was found between no union and periprosthetic fractures (p=0.047) and number of proximal screws (p=0.045). Use of less than 5 or more than 6 proximal screws were found to be associated with proxima l plate failure and nonunion.
Conclusion: According to the results, the use of 5 or 6 proximal screws reduces the risk of no union. Use of less than 5 proximal screws may not provide the necessary fixation, while using more than 6 proximal screws may result in a too rigid construct.
On the other hand, periprosthetic fractures represent an independent risk factor for non-union.
Keywords
Distal femoral fractures, No consolidation, Non-union, Locking plate, LISS
Introduction
The distal femur constitutes the region between the metaphyseal-diaphyseal junction and the femoral condyles [1]. Fractures of this segment, which includes supracondylar and intercondylar fractures, represent between 4 and 7% of all the femur fractures, with an incidence of 37 cases per 100,000 habitants/year [2]. These fractures present a bimodal distribution depending on the injury mechanism. There is a peak incidence in young adults, with male predominance and associated with high-energy trauma, and a second peak in the elderly population with female predominance and associated with low energy trauma and osteoporosis [3]. There are several classifications which described these fractures, among them AO classification is most widely used (Arbeitsgemeinschaft für Müller osteosynthesefragen) for long bone fractures [4,5] due to its prognosis and therapeutic character [6] (Table 1).
| Segment 33: Distal Femur | |
|---|---|
| 33-A Extraarticular fracture | |
| 33-A1 simple | |
| 33-A2 metaphyseal wedge and/or fragmented wedge |
|
| 33-A3 metaphyseal complex | |
| 33-B Partial articular fracture | |
| 33-B1 lateral condyle, sagittal | |
| 33-B2 medial condyle, sagittal | |
| 33-B3 coronal | |
| 33-C Complete articular fracture | |
| 33-C1 articular simple, metaphyseal simple | |
| 33-C2 articular simple, metaphyseal multi- fragmentary | |
| 33-C3 articular multi-fragmentary | |
Table 1: Distal femur AO classification.
Supracondylar and intercondylar femur fractures (AO 33 A1–C3) suppose a surgical challenge for orthopedic surgeons. On the one hand, as articular fractures, they require anatomical articular surface reduction and absolute stability to allow early mobilization avoiding joint stiffness and loss of muscle mass. On the other hand, as a long bone fracture, the length, alignment and rotation of the limb must be restored [7-12]. At surgical treatment, there are various therapeutic options, and the choice of the type of implant depends on the surgical objective, influenced by the characteristics of the patient and fracture pattern [13].
Nowadays, the most commonly used technique consists in internal fixation using less invasive stabilization system (LISS, Synthes, West Chester, USA). This plate with locked screws was patented in 1990 and the first procedure was carried out in 1995. The LISS system has been approved by the AO Technical Commission as a surgical method that uses the angular stability between the plate and the screws improving considerably the stability of the fracture fixation. Other advantages of LISS plates are that it allows a good anatomical reduction, periosteal preservation, and an early mobilization; meeting the criteria of the AO. The biomechanical properties to withstand the fracture collapse, the relatively easy implantation and the opportunity to obtain multiple fixation areas in the distal fragment even in low bone stock cases, have supported the use of plates with locked screws as a gold standard for fixing this type of fractures [2]. Despite the initial good results, there are still nonunion and implant failure cases [14-17]. In recent years the increase in the incidence of this cases is an object of interest for orthopedic surgeons, and attributable, in part, to the popularization of these types of implants, to the application of this to a wider range of patients, and an increase in the frequency of its use in the treatment of high energy injuries. Implant length is a crucial point in plate osteosynthesis. In general, long plates offer greater biomechanical advantages, but there are no studies that analyze the influence of the length of this plate in the consolidation of distal femur fractures.
This study aims to analyze the possible risk factors for the absence of consolidation in the treatment of distal femur fracture with LISS plate. The main objective is to identify the ratio plate length/fracture height as a predictor of non-union risk in less invasive stabilization system (LISS). The secondary objectives are to analyze the patient comorbidities, the fracture pattern and the characteristics of osteosynthesis, and its relationship with the need for reintervention, infection, and implant failure. We hypothesize that there is a statistical relationship between a low ratio of plate length/fracture height and cases of non-union.
Methods and Materials
The study protocol was approved by the institutional review board. We developed a retrospective case-control study including all consecutive adult patients diagnosed of supracondylar femur fractures and supracondylar fractures with fracture line extending to distal third of femoral shaft (defined as segment 33 in the AO / OTA classification) [4,5], treated between 01/01/2007 and 12/31/2017.
Exclusion criteria were: (i) patients with conservative treatment, (ii) patients with distal femur fracture treated surgically with other implant than LISS plate, (iii) absence of pre and postoperative radiological study, (iv) follow-up less than 3 months after surgical treatment, and (v) patients with radiographic delay consolidation at 3 months and follow-up less than 6 months.
We identified 151 distal femur fractures treated during the study period. Of the 151 fractures, 87 (57.6%) had some exclusion criteria (12 for orthopedic treatment, 38 for surgical implant treatment different from LISS, 14 due to the absence of a complete radiological study and 23 due to lack of follow-up), obtaining a final cohort of 64 fractures in 59 patients, which was the population analyzed.
The study cohort was divided into two groups based on the presence or absence of fracture consolidation. Each group was analyzed separately to determine risk factors. It was defined as non-union for those cases with: (i) construct failure, (ii) need for secondary procedures to promote fracture consolidation or (iii) absence of radiological criteria for fracture consolidation (bone bridges and bone callus) on the anteroposterior and lateral radiographs of the femur at 6 months after intervention, valued independently by two observers (AMA, MDJ). In the discordant cases, the criteria of the most experienced surgeon (AMA) were followed. An informed written consent was obtained from each patient before data review.
Surgical treatment
All the patients received antibiotic and thromboembolic prophylaxis. All patients were treated by open reduction with a lateral approach of the distal femur and internal fixation with LISS® plate system. All implants were made of steel. The osteosynthesis construct characteristics (plate length, interfragmentary screws use, the number of proximal and distal screws and unicortical or bicortical screws use) were a decisión of the responsible surgeon in each case. All the patients were initially immobilized with an extended orthosis. Withdrawal of the orthosis for active mobilization, as well as the postoperative discharge time, was variable according to the responsible surgeon’s choice.
Patient characteristics
Patients’ medical records were reviewed and age, sex, obesity (defined as BMI> 30 Kg/m2), smoking habit, and diabetes were analyzed. The presentation of comorbidities that will affect the lower limbs (paraplegia, sclerosis multiple, and post-poliomyelitis paralysis) was also recorded.
Fracture characteristics
Fracture characteristics analyzed were: (i) fracture classification (AO classification system) [4,5], (ii) presence of knee arthroplasty (periprosthetic fracture), (iii) type of fracture (open or closed), (iv) laterality (left or right) and (v) injury mechanism (low or high energy). For open fractures, Gustilo and Anderson classification [18] was used, and for periprosthetic fractures, Lewis and Rorabeck classification [19] was used.
Osteosynthesis characteristics
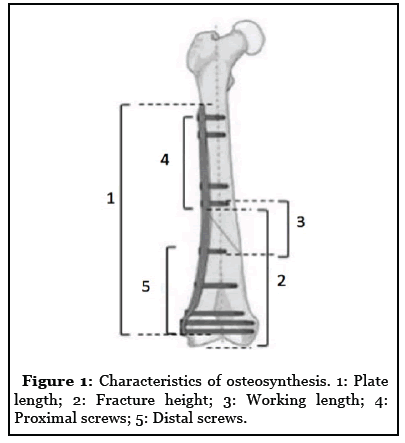
Postoperative radiographs were analyzed and the following osteosynthesis characteristics were recorded: (i) overall plate length (measured in diaphyseal holes), (ii) number of plate holes located in the proximal fragment, (iii) working length (number of holes spanning the fracture zone between the most distal screw in the proximal fragment and the most proximal screw in the distal fragment), (iv) number of screws proximal to the fracture focus, (v) number of screws distal to the fracture focus, (vi) number of proximal cortices and (vii) plate length/fracture height ratio (defined as the ratio between the length of the plate in mm and the distance from the articular surface of the medial condyle to the proximal end of the fracture focus in mm, measured on the same anteroposterior radiograph of the femur). Construct characteristics are illustrated in Figure 1.
The use of graft or bone substitute in the treatment was also analyzed.
Outcome measures
Malaignment was also analyzed, defined as angulation>7° in the sagittal plane or>10° in the coronal plane, shortening>1.5 cm, articular step>2mm or presence of distraction of the focus of fracture [20].
During the follow-up non-weight bearing, time to radiographic consolidation, the ability to final ambulation, final range of motion (ROM) and the presence of complications: infection, disassembly and need for reintervention was analyzed.
Statistic analysis
Statistical analysis was performed using the IBM SPSS Statistics® software version 21.0 (IBM, Armonk, USA) expressing the data in arithmetic mean (± standard deviation; rank). The hypothesis test was performed using the Chi-square test, Fisher’s exact test, the t-Student’s test, and the Wilcoxon signed ranges, depending on the use of dichotomous variables, quantitative or ordinal. Inter-observer reliability was analyzed by Cohen’s kappa coefficient. It was analyzed if there were statistical differences between both groups and each one of the characteristics studied, performing analysis by subgroups to avoid confounding factors. A p ≤ 0.05 was considered statistically significant.
Results
Patient characteristics
The average age of the patients was 64.9 years (± 16.5; 29-92), 14 men and 45 women. The average follow-up was 36.75 months (± 42.71; 4-218). Of the total 64 fractures, 15 fractures (23.43%) presented radiological criteria of absence of consolidation and required secondary intervention to promote union (cases). The other 49 fractures (76.56%) healed without unplanned surgeries and they were the control group. The average time to consolidation was 6.23 months (± 3.36; 3-17). The interobserver reliability beetwen the two observers was good (k=0.83; CI 95%: 0.78-0.88).
Five of the 59 patients presented bilateral femur fracture. A total of 7 patients presented comorbidities that affect the lower limbs: 2 patients (3.1%) with paraplegia (1 patient in the healed group and another in the non-union group), 2 cases (3.1%) with multiple sclerosis (1 patient in the healed group, and another in the non-union group), and 5 patients (7.8%) with postpolio residual paralysis in the operated limb (5 patients in the healed group, none in the non-union group). In the analysis of demographic and general data, we did not find statistically significant differences between both groups. Demographic characteristics are resumed in table 2.
| Patient characteristics | Entire Cohort (n=64) | Healed Fractures (n=49) | Non-Union (n=15) | p |
|---|---|---|---|---|
| Age (y) mean (SD; range) | 64.9 (± 16.5; 29-92) | 66.1 (29-92) | 62.26 (38-85) | 0.149 |
| Follow-up (m) mean (SD; range) |
36.75 (± 42.71; 4-218) | 28.08 (4-218) | 65.06 (14-218) | 0.064 |
| Gender (n) | 0.096 | |||
| Female | 76.27% (45) | 70.83% (34) | 93.33% (14) | |
| Male | 23.72% (14) | 29.16% (14) | 6.66% (1) | |
| Obesity (n) | 20.31% (13) | 14.28% (7) | 40% (6) | 0.061 |
| Diabetes (n) | 20.31% (13) | 18.75% (9) | 26.67% (4) | 0.444 |
| Smokers (n) | 25% (16) | 25% (12) | 26.67% (4) | <0.99 |
Table 2: Demographic characteristics.
In the analysis of fracture characteristics, a total of 15 fractures (23.43%) occurred as a result of high energy trauma and 7 fractures were open fractures (10.93%). There were 6 periprosthetic fractures (9.37%) and statistically significant differences were obtained between both groups (p=0.047), being these more frequent in the non-union group. The fracture characteristics are summarized in table 3.
| Fracture characteristics | Entire Cohort (n=64) | Healed Fractures (n=49) | Non-Union (n=15) | p |
|---|---|---|---|---|
| AO/OTA Classification (n) | 0.90 | |||
| A | 43.75% (28) | 42.85% (21) | 46.66% (7) | |
| B | 23.43% (15) | 30.61% (15) | 0 | |
| C | 32.81% (21) | 26.53% (13) | 53.33% (8) | |
| Periprosthetic fracture (n) | 9.37% (6) | 4.08% (2) | 26.67% (4) | 0.047 |
| Type of fracture (n) | <0.99 | |||
| Open | 10.93% (7) | 12.24% (6) | 6.66% (1) | |
| Closed | 89.06% (57) | 87.75% (43) | 93.33% (14) | |
| Side (n) | 0.39 | |||
| Left | 56.25% (36) | 53.06% (26) | 66.66% (10) | |
| Right | 43.75% (28) | 46.93% (23) | 33.33% (5) | |
| Mechanism of injury (n) | 0.737 | |||
| Low energy | 76.56% (49) | 77.55% (38) | 73.33% (11) | |
| High energy | 23.43% (15) | 22.44% (11) | 26.67% (4) |
Table 3: Fracture characteristics.
No significant differences were found in the number of distal screws, the number of proximal cortices, working length, graft use or the plate length/fracture height ratio. There was a significant difference between both groups in the number of proximal holes (p=0.032) and the number of proximal screws (p=0.045) (Figure 2). The difference is especially significant taking as a cut-off point the use of 5 proximal screws or more (p=0.012). The osteosynthesis construct and treatment characteristics are summarized in table 4.
| Osteosynthesis characteristics mean (range) | Entire Cohort (n=64) | Healed Fractures (n=49) | Non-Union (n=15) | p |
|---|---|---|---|---|
| Plate length (holes) | 7.98 | 8.02 (5-12) | 7.86 (5-11) | 0.79 |
| Proximal holes | 6.92 | 6.10 (3-10) | 5.06 (2-9) | 0.032 |
| Working length (holes) | 1.53 | 1.59 (0-7) | 1.33 (0-5) | 0.612 |
| Proximal screws | 5 | 5.16 (2-8) | 4.46 (2-7) | 0.045 |
| Distal screws | 5.57 | 5.53 (3-8) | 5.73 (0-7) | 0.555 |
| Proximal cortices | 6.74 | 6.85 (3-14) | 6.4 (3-12) | 0.525 |
| Plate length/fracture height ratio | 2.31 | 2.38 (1.31-4.81) | 2.1 (1.33-4.23) | 0.226 |
| Bone graft | 15.62% (10) | 12.5% (6) | 26.66% (4) | 0.21 |
Table 4:Osteosynthesis construct characteristics.
Outcome measures
A total of 12 fractures (18.75%) met radiological criteria of malalignmnet (3 in the non-union group, and 9 in the healed group), without statistically significant differences between groups.
Of the total 64 fractures, 21 (32%) needed secondary surgical intervention: 8 in the healed group (5 hardware removal and 3 arthrolysis) and 13 in the non-union group (all due to lack of consolidation). In the group of lack of consolidation, the average time to reintervention was 10.9 months (± 5.43; 3-20). In 6 of the 13 (46.1%) patients, new osteosynthesis with LISS plate was performed, all of them evolving to consolidation in an average time of 7 months (± 6.87; 3-22) since the reintervention. Of the other 7 (53.9%) remaining patients, 5 were treated by nail osteosynthesis, one by arthrodesis and another one by arthroplasty. Two patients with no consolidation were treated by conservative treatment. There was a significant difference in the number of reintervention (p=0.036).
There were 5 cases of complications: 2 cases (3.1%) of neuropraxia of the common peroneal nerve, who recovered completely, and 3 cases (4.6%) of infection: two cases of superficial infections treated with antibiotic therapy, and one septic absence of consolidation that required debridement, hardware removal at 12 months after surgery and a new nail osteosynthesis. No statistically significant differences were found in the number of complications between both groups. Outcome measures are presented in table 5.
| Entire Cohort (n=64) | Healed Fractures (n=49) | Non-Union (n=15) | p | |
|---|---|---|---|---|
| Malalignment (n) | 18.75% (12) | 18.36% (9) | 20% (3) | <0.99 |
| Infection (n) | 6.25% (4) | 6.12% (3) | 6.66% (1) | <0.99 |
| Reintervention (n) | 32.81% (21) | 16.32% (8) | 86.66% (13) | 0.036 |
Table 5: Outcome measures.
The average time to load was 3.69 months (± 2.62; 1-17). ROM at the end of the mean follow-up was 93° (± 16.9; 40-130). At the end of the follow-up, 6 patients (10.1%) were non-ambulatory, 3 of them did not ambulate before the fracture (2 cases of paraplegia, a case of advanced multiple sclerosis) and the other 3 cases performed bedchair life before the fracture.
Discussion
The treatment of distal femur fractures represents a surgical challenge. Various factors can influence the prognosis, affecting the fracture consolidation and the risk of development absence of consolidation. Some of these factors may be related to the patient comorbidities, others are related to the fracture characteristics, and finally, a large number of factors are controlled by the surgeon, of which the most important are concerning the osteosynthesis characteristics [2,12,21,22].
Locked plates, like LISS, provide stability acting as internal fixator and they have been widely used for the treatment of distal femur fractures [9,10,13,19]. While preliminary studies demostrated very good results [10,23], posterior studies showed a negligible percentage of non-union and implant failure [14,16]. Thus, determining which factors are involved and which of them can be modified by the surgeon could develop protocols that help when designing the optimal treatment for each patient.
The percentage of non-union obtained in the study (23%) agrees with those described in other studies, between 0 and 32% [24]. Several authors have previously suggested some factors associated with non-union, such as the presence of obesity, open fracture, infection, graft use or the injury mechanism [2,12]. In this study, statistically significant differences were not found in the presence or absence of these factors, which could be explained due to the small sample size. Only obesity had a result close to the significance. Rodriguez et al. [2] found no significant differences in terms of age, sex, diabetes, smoking, fracture classification, periprosthetic fracture, length of the plate and total screw density. Except for the presence of periprosthetic fracture, which is significant for a lack of consolidation, the other factors agree with the aforementioned study. Differences between studies may be due to heterogeneity of populations and the lack of standardized protocols for postoperative care.
Regarding the characteristics of the plate, Wong et al. [21] found a high incidence of proximal screw failure in their database and suggested that plate length may be the cause of proximal screw failure. On the contrary, Button et al. [25] found that with the use of 13-hole plates, disassembly was not avoided. In the present study, only one disassembly was recorded by the failure of the proximal screws, which could be due to a lower presence of osteoporotic patients in our sample.
The purpose of this study was to identify the plate length/fracture height ratio as a predictor of nonunion risk. Although the most common method used by surgeons to identify plate length is the number of holes, locked plates are pre-contoured plates that must always be placed in the same position and we can not move the plate to leave the fracture in the middle third of the plate. So, the plate length/fracture height ratio could be a more useful and objective measure than plate length analysis in isolation. According to the results observed in other types of plates, the hypothesis was that a high ratio would be biomechanically better, but the results obtained do not support this hypothesis. Equally, there were no significant results regarding the number of proximal cortices, although the use of unicortical screws compared to bicortical has been also recognized as a potential cause of plate disassembly, particularly of osteoporotic bones. Fulkerson et al. [22] suggested that their cases of absence of consolidation was related to the use of unicortical screws and several authors [21,26] recommend the use of locked bicortical screws to provide a more stable construct in patients with severe osteopenia and great fracture comminution. In the present study, there was statistically significant differences in the number of proximal screws, especially from 5 screws, which would suggest that the number of proximal screws is more important than the number of proximal cortices.
The results of this study should be taken with caution due to the methodological limitations, which include a relatively small sample of patients, and the fact of being a retrospective study, with the limitations inherent in this type of study. A power analysis was not performed, and it is possible that the study was underpowered to evaluate all the potential risk factors. Another limiting factor was the interobserver differences in radiographs interpretation. The overall working lenght in our sample is too small and the role that the interfragmentary screws can play providing stability and promoting consolidation has not been analyzed. All the plates in our sample are made of stainless steel, so it was not possible to determine if the use of plates of steel or titanium was related to implant failure, a factor which has been shown to play a role in other studies [2].
Conclusion
Although the association of absence of consolidation could not be demonstrated with certain risk factors already known for other fractures and demonstrated in other studies, the present study highlights the need to fix with at least 5 proximal screws in LISS plate, regardless of the fracture height. Osteosynthesis with less proximal screws may be associated with a greater likelihood of non-union and excessively long plates can pose greater technical difficulty and risk surgical without obtaining an associated benefit. In the present study, only one specific type of fixing system is analyzed, it would be interesting to study the behavior of other systems.
Based on the results of this work, it can be concluded that osteosynthesis with at least 5 proximal screws reduces the risk of non-union. Also, the periprosthetic fractures supose a greater risk of lack of consolidation. At the time of reducing the risk of absence of consolidation is important for the choice of osteosynthesis construct by the surgeon.
Disclosure Statement
No potential conflict of interest was reported by the authors.
References
2. Rodriguez EK, Boulton C, Weaver MJ, Herder LM, Morgan JH, Chacko AT, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures. Injury. 2014 Mar 1;45(3):554-9.
3. Gwathmey WF, Jones-Quaidoo SM, Kahler D, Hurwitz S, Cui Q. Distal femoral fractures: current concepts. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2010 Oct 1;18(10):597-607.
4. Müller ME, Perren SM, Allgöwer M, Müller ME, Schneider R, Willenegger H. Manual of internal fixation: techniques recommended by the AO-ASIF group. Springer Science & Business Media; 1991.
5. Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Springer Science & Business Media; 2012 Dec 6.
6. Weight M, Collinge C. Early results of the less invasive stabilization system for mechanically unstable fractures of the distal femur (AO/OTA types A2, A3, C2, and C3). Journal of Orthopaedic Trauma. 2004 Sep 1;18(8):503-8.
7. Valles JF, Rodríguez FR, Gómez JM. Distal femur fractures. Comparative analysis of two different surgical treatments. Mexican Orthopedic Act. 2010; 24 (5): 324-30.
8. Heiney JP, Barnett MD, Vrabec GA, Schoenfeld AJ, Baji A, et al. Distal femoral fixation: a biomechanical comparison of trigen retrograde intramedullary (im) nail, dynamic condylar screw (DCS), and locking compression plate (LCP) condylar plate. Journal of Trauma and Acute Care Surgery. 2009 Feb 1;66(2):443-9.
9. Albert MJ. Supracondylar fractures of the femur. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 1997 May 1;5(3):163-71.
10. Hontzsch D. Distal femoral fracture-technical possibilities. Kongressbd Dtsch Ges Chir Kongr. 2001;118:371-4.
11. Kanabar P, Kumar V, Owen PJ, Rushton N. Less invasive stabilisation system plating for distal femoral fractures. Journal of Orthopaedic Surgery. 2007 Dec;15(3):299-302.
12. Ricci WM, Streubel PN, Morshed S, Collinge CA, Nork SE, Gardner MJ. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. Journal of Orthopaedic Trauma. 2014 Feb 1;28(2):83-9.
13. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006 Aug 1;37(8):691-7.
14. Chen F, Mont MA, Bachner RS. Management of ipsilateral supracondylar femur fractures following total knee arthroplasty. The Journal of Arthroplasty. 1994 Oct 1;9(5):521-6.
15. Figgie MP, Goldberg VM, Figgie III HE, Sobel M. The results of treatment of supracondylar fracture above total knee arthroplasty. The Journal of Arthroplasty. 1990 Sep 1;5(3):267-76.
16. Kobbe P, Klemm R, Reilmann H, Hockertz TJ. Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury. 2008 Apr 1;39(4):472-9.
17. Mize RD, Bucholz RW, Grogan DP. Surgical treatment of displaced, comminuted fractures of the distal end of the femur. The Journal of Bone and Joint Surgery. American Volume. 1982 Jul;64(6):871-9.
18. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. The Journal of Bone and Joint Surgery. 2002 Apr 1;84(4):682.
19. Lewis PL, Rorabeck CH, Anglish RD. Fractures of femur, tibia and patella following total knee arthroplasty: decision, making and principles of management. Instr Course Lecture 1998,47:449-60.
20. Giles JB, DeLee JC, Heckman JD, Keever JE. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. The Journal of Bone and Joint surgery. American Volume. 1982 Jul 1;64(6):864-70.
21. Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. International Orthopaedics. 2005 Apr 1;29(2):117-20.
22. Fulkerson E, Tejwani N, Stuchin S, Egol K. Management of periprosthetic femur fractures with a firstgeneration locking plate. Injury. 2007 Aug 1;38(8):965-72.
23. Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury. 2000 Sep 1; 31: 62-94.
24. Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femur fractures: is there a problem with fracture healing? Journal of Orthopaedic Trauma. 2011 Feb 1;25:S8-14.
25. Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur: a report of four cases. Journal of Orthopaedic Trauma. 2004 Sep 1;18(8):565-70.
26. Kanabar P, Kumar V, Owen PJ, Rushton N. Less invasive stabilisation system plating for distal femoral fractures. Journal of Orthopaedic Surgery. 2007 Dec;15(3):299-302.
