Abstract
Daily activity restriction is an expected physical behavior aiming to prevent falls in the older population. However, it plays dual roles in preventing falls, both positive and harmful. Therefore, the degree of daily activity restriction is proposed as a critical factor influencing the weight ratio of the positive and negative roles and finally determining the efficacy of fall prevention. Thus, quantification of daily activity restriction is essential to learn its efficacy.
We proposed using activity frequency to quantify activity restriction and have testified its good sensitivity to discriminate the degree of activity restriction in older populations. We further attempted to link the degree of activity restriction with the degree of fear of falling to estimate the dual roles of activity restriction in preventing falls. Based on it, a new Composite Activity-specific Risk of Falls Scale tool has been developed. It is promising to use for guiding the modification of physical behavior to prevent falls in older populations. However, further studies are required to establish the evidence for its application.
Keywords
Activity restriction, Fear of falling, Falls, Risk, Physical disability, Elderly
Main Text
Activity restriction is the physical behavior of avoiding or reducing physical or daily activities, usually caused by fear of adverse events or physical disability. Here, activities are classified based on their objectives, such as physical activities to improve or maintain physical fitness and daily activities to meet daily living requirements. However, physical activities usually comprise daily activities that require energy expenditure by the skeletal muscles. The circumstances of activity restriction depend on the specific causes or aim in different populations. For instance, physical activity restriction is a common strategy for preventing heart attacks in patients with severe cardiomyopathy [1,2]. Daily activity restriction in the upright position is recommended to prevent preterm births in high-risk pregnancies [3]. Excessive fear of falling can induce general daily activity restriction and is therefore regarded as a strategy for preventing falls in the older population [4]. The efficacy of activity restriction in preventing adverse events is an important research topic that helps optimize behavior strategy.
Nevertheless, we realized through literature review that the measures of activity restriction still need to be standardized. In general, two methods have been used to assess activity restrictions in previous studies [1-4]: a qualitative approach based on self-perception and a quantification method based on the actual activity amount. The qualitative approach is used more commonly than the quantification method. However, self-perceived qualitative physical activity restriction has been reported not to match the actual physical activity amount and demonstrated a weaker correlation with physical fitness than the latter measure in previous studies in children and adolescents with congenital heart disease [1,2]. The findings hint that the quantified behavior of activity restriction is more proper than self-perceived qualitative behavior to consider when exploring the efficacy of activity restriction in preventing adverse events.
For daily activity restriction, we are the first to propose a quantification method based on activity frequency [5-7]. We designed a question, “How often have you performed the following activities in the previous 1-month period?” with a 5-point Likert scale for answers (0, no engagement; 1, occasional engagement [monthly]; 2, sometimes [weekly]; 3 often [daily]; and 4, very often [daily but with a higher frequency than usual]). The Activities-Specific Balance Confidence (ABC) scale was adopted as the daily activity item structure to evaluate activity-specific frequency. The quantification method sensitively identified the restriction of most daily activities in patients with stroke compared to the healthy older participants. Four restricted daily activities, including standing on a chair to reach, walking in crowds and being bumped, taking an escalator without holding onto a railing, and walking on icy sidewalks, demonstrated total restrictions in all participants with stroke. Avoidance of these four activities has been previously reported [8]. These activities cause patients to experience fall-induced environmental hazards and usually provoke an excessive fear of falling in older patients [8]. Fortunately, these activities involve alternative methods of daily living. For example, people can keep everything in easy reach, beat the rush when shopping, hold a handrail on an escalator, walk outside when sidewalks are not wet. Therefore, avoiding these activities is considered beneficial for fall prevention. This speculation is supported by the evidence that the activity frequency of walking in crowds and being bumped upon is an independent discriminator of fall history, with an odds ratio of 3.31 [5].
Nevertheless, restricting other activities, such as up and down stairs, picking up a slipper, and reaching eye level, may not be effective against falls. Because long-term restriction may result in the deconditioning of relevant physical function, and unfamiliarity with skills involved in activities such as movement sequence and timing. However, these basic daily activities cannot be avoided in daily living, and poor performance in occasional execution may lead to an immediate risk of falls. The dual roles of daily activity restriction in fall prevention have been previously proposed [9,10], positive mainly by decreasing exposure to fall-induced environmental hazards and negative primarily due to physical deconditioning resulted in. We further speculate that the degree of daily activity restriction could be a key factor influencing the weight ratio of the positive and negative roles and finally determining the efficacy of fall prevention.
We are the first to evaluate the impact of activity restriction on the risk of falls by quantifying activity restriction, fear of falling, and their interaction [6,7]. Based on it, a tool to evaluate the risk of falls in older people and persons with physical disabilities has been developed: the Composite Activity-specific Risk of Falls Scale (CARFS). The CARFS comprises 14 items on daily activities, with one question on the performance frequency of each activity, as mentioned above, and the other on the degree of fear of falling. An expert panel from all balance-related activities of categories of the International Classification of Functioning, Disability, and Health of the World Health Organization determined the 14 activity items. The question on fear of falling is “How much fear of falling do you have when you perform the following activities,” with the answer scored by a 5-point Likert scale (fear of falling: 0, no worry; 1, slight worry; 2, moderate worry; 3, high worry; and 4, extreme worry). The composite risk of falls for each item (C) was estimated by the degree of fear of falling (A) and activity frequency (B) using the formula C = A+(4-B)+A´B/2, where 4-B indicates the degree of activity restriction [6, 7]. The notion underlying the formula is that daily activity restriction is beneficial when the fear of falling is high (possibly due to dangerous environmental hazards or poor physical ability) but unnecessary and even harmful when the fear is mild or nonexistent. The coefficient value of 1/2 was determined from four choices of 1/k (k = 1, 2, 3, 4) by the expert panel based on the rationality of the influence of the link between fear of falling and activity frequency on the risk of falls [6]. The relationships between the composite risk of falls, fear of falling, and activity frequency for each activity item are shown in Table 1. This formula, which considers the dual effects of activation restriction on the risk of falls, is valuable for determining the optimal behavior strategy based on the degree of fear of falling. However, a precondition must be met for clinical application: the fear of falling matches physical ability, especially balance, and mobility. In general, fear of falling is closely correlated with balance and mobility in older people, but with approximately 30% exception in community-dwelling older persons [11]. Psychological or cognitive interventions can be more appropriate for those with disparities between perceived fear and physical function before modifying their physical behavior [11].
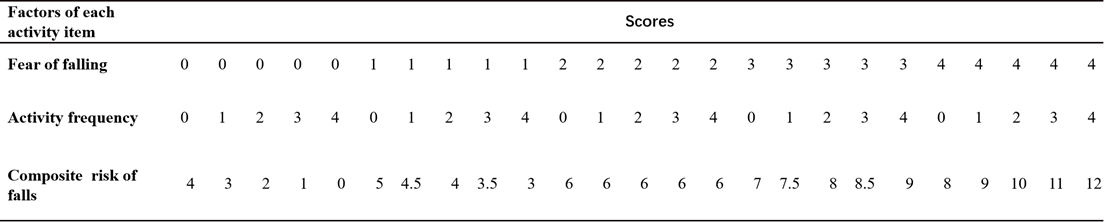
Table 1. Composite activities-specific risk of falls estimated by linking fear of falling with activity frequency.
The CARFS is promising for screening fall risk and modifying physical behavior to prevent falls. It is a reliable and valid tool for measuring the risk of falls, demonstrating excellent test-retest reliability, excellent internal consistency of the CARFS items, good-to-excellent convergent validity with the ABC scale and ambulation, and no ceiling or floor effects in older patients and patients with physical disabilities due to stroke or spinal cord injury [7]. However, evidence on the predictive validity of falls, sensitivity to change, and effectiveness of optimizing physical behavior for fall prevention have yet to be established in the target population.
Daily activation restriction is an expected physical behavior induced by an excessive fear of falling to prevent falls in older people. Using activity frequency, we recommend quantifying daily activity restriction that reflects actual physical behavior more directly than the self-perceived qualitative manner does. Quantified activity frequency helps estimate the dual roles of activity restriction in preventing falls by linking it with the degree of fear of falling. The CARFS is a reliable and valid scale that links activity-specific frequency and fear of falling to evaluate the risk of falls and guides the modification of physical behavior to prevent falls. Further studies are required to establish the evidence for its application.
Acknowledgment
We acknowledge the Shanghai Disabled Persons Federation for funding this work (Research Project: K2018029).
References
2. O'Byrne ML, McBride MG, Paridon S, Goldmuntz E. Association of Habitual Activity and Body Mass Index in Survivors of Congenital Heart Surgery: A Study of Children and Adolescents With Tetralogy of Fallot, Transposition of the Great Arteries, and Fontan Palliation. World J Pediatr Congenit Heart Surg. 2018;9(2):177-84.
3. Palacio M, Mottola MF. Activity Restriction and Hospitalization in Pregnancy: Can Bed-Rest Exercise Prevent Deconditioning? A Narrative Review. Int J Environ Res Public Health. 2023;20(2).
4. Denkinger MD, Lukas A, Nikolaus T, Hauer K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 2015;23(1):72-86.
5. Chen LY, Wang JX, Chen YY, Yang YJ, Yao JJ, Shen X. Activities-specific performance frequency can accurately detect fallers in elderly populations: an alternative method for quantifying activity restrictions. BMC Geriatr. 2022;22(1):205.
6. Wang JX, Chen LY, Jiang YN, Ni L, Sheng JM, Shen X. Establishing content validity for a composite activities-specific risk of falls scale:linkage between fear of falling and physical activity. BMC Geriatr. 2021;21(1):275.
7. Jiang YN, Wang JX, Chen LY, Yao JJ, Ni L, Sheng JM, et al. Reliability and Validity of the Composite Activity-Related Fall Risk Scale. Front Neurol. 2022;13:832691.
8. Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). J Gerontol B Psychol Sci Soc Sci. 1998;53(1):P43-50.
9. Moreira NB, Rodacki ALF, Pereira G, Bento PCB. Does functional capacity, fall risk awareness and physical activity level predict falls in older adults in different age groups? Arch Gerontol Geriatr. 2018;77:57-63.
10. Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33(4):368-73.
11. Delbaere K, Close JC, Brodaty H, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. Bmj. 2010;341:c4165.
