Abstract
Purulent pericarditis was a prevalent complication of streptococcal pneumonia prior to the antibiotic era. In this article, we report a 68-year-old male presenting with dyspnea, chest pain, left knee pain, diagnosed with S. pneumoniae bacteremia and septic arthritis with isolation of same pathogen from synovial fluid.
ECG showed diffuse ST elevations, TTE showed small pericardial effusion along RV free wall. A subsequent TTE showed a pericardial effusion with signs of tamponade. Patient underwent a pericardiocentesis with drainage of purulent fluid. Repeat TTE showed a 2.7 mm vegetation on mitral valve. CT surgery recommended only antibiotics.
Purulent pericarditis is a life-threatening disease, so timely diagnosis and treatment are essential.
Keywords
Purulent pericarditis, Tamponade, Infective endocarditis, Pericardiocentesis
Introduction
Purulent pericarditis used to be a common complication of streptococcal pneumonia in the pre-antibiotic era, however its incidence has declined after the introduction of broad-spectrum antibiotics [1]. Purulent pericarditis is defined as the presence of gross pus or microscopic purulence in the pericardial space. There are several mechanisms of pathogenesis, including direct spread from an intrathoracic infection, such as from a bacterial pneumonia, pneumonia with empyema or esophageal rupture, hematogenous spread, due to bacteremia; extension from a myocardial focus, such as a valvular abscess or extension from a subdiaphragmatic focus, for example spread from a subphrenic abscess [2]. Staphylococcus aureus is the most common cause of purulent pericarditis overall, however Streptococcus pneumoniae is more common when there is direct spread from intrathoracic infection, such as pneumonia [3]. In the pre-antibiotic era underlying infectious processes were the predisposing factors in development of purulent pericarditis, however in the modern practice it is less common, with thoracic surgery, renal failure, malignancy, and pre-existing pericardial disease being the predisposing factors [3]. We present a case of a 68-year-old male with purulent pericarditis in the setting of streptococcal pneumonia.
Case Presentation
History of presentation
68-year-old male with past medical history of hypertension, diabetes, and hypothyroidism presented with dyspnea, chest pain as well as left knee pain and edema. The patient endorsed that few days prior to presentation, he experienced a sudden onset of shortness of breath, mainly with exertion, associated with cough productive of yellow sputum and orthopnea as well as sudden onset of left knee pain and swelling. He also complained of central, 7/10 non-radiating, dull chest pain mainly with exertion: lasting less than 5 minutes, relieved with sitting or rest and with no aggravating factors.
Further history included social history of prior tobacco use, no alcohol or illicit substance use. There was no pertinent family history. The patient has not been hospitalized recently and has not received any antibiotics.
Investigations
Chest X-ray showed a consolidating indication of pneumonia. Blood cultures were collected and grew S. pneumoniae and the same organism was isolated in the synovial fluid after arthrocentesis.
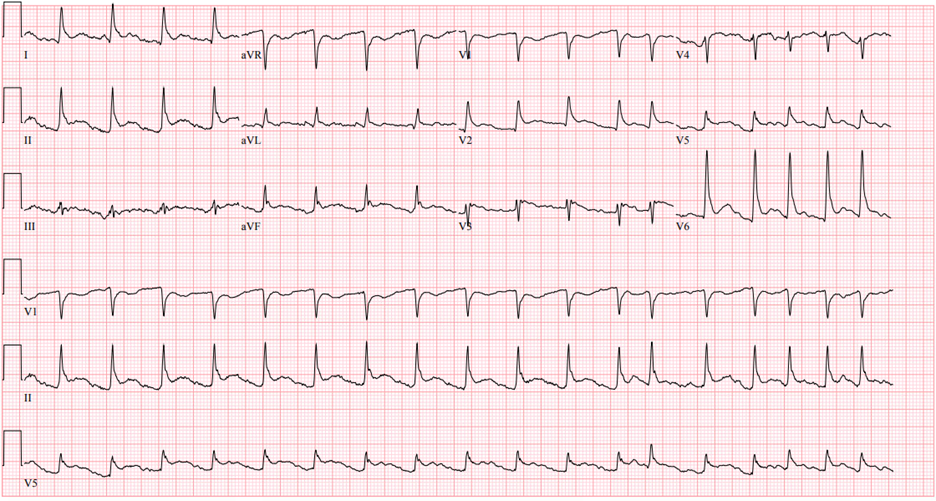
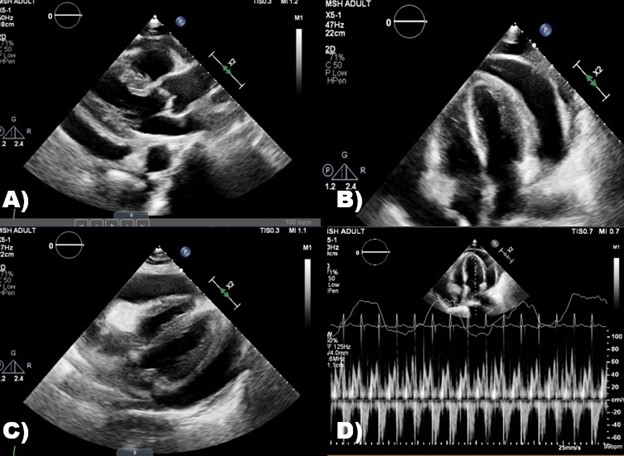
ECG (Figure 1) was performed and showed diffuse ST elevations therefore a transthoracic echocardiogram (TTE) (Figure 2) was obtained. It showed a small, free flowing pericardial effusion along the RV free wall with no evidence of hemodynamic compromise.
Figure 1. 12-lead ECG showing diffuse ST elevations.
Figure 2. A) Parasternal long axis view of large effusion. B) Apical 4-chamber view of large pericardial effusion. C) 4-chamber view of large circumferential pericardial effusion. D) Increased respiratory variation in transmitral flow.
Serial TTEs were done showing increasing size of pericardial effusion. On day 7 of hospitalization, patient had several episodes of atrial fibrillation with RVR complicated by hypotension. A subsequent TTE showed a large, free-flowing pericardial effusion with signs of early tamponade.
Management
Our patient underwent urgent pericardiocentesis with drainage of one liter of purulent fluid (Figure 3) and placement of pericardial drain.
Figure 3. Purulent pericardial fluid.
Fluid analysis confirmed purulent pericarditis; however, gram stain and cultures were negative. Repeat TTE showed a trivial pericardial effusion and a 2.7 mm mass suspicious for vegetation on the mitral valve with moderate MR, confirmed by TEE. CT surgery was consulted, and they recommended 6 weeks of antibiotics with no surgical intervention. The hospital course was complicated by multiple episodes of atrial fibrillation with rapid ventricular response, treated with beta blockers as well as amiodarone. Further hospital stay was complicated by left-sided empyema which was drained by pig-tail catheter placement by interventional radiology. Both the pericardial drain and pig-tail catheter were removed after several days, and the patient was continued on high-dose Ceftriaxone for a total of 6 weeks per infectious disease recommendations.
Outcome
The patient was successfully discharged to a skilled nursing facility for a prolonged IV antibiotic course with a follow up with cardiology. Several follow up TTEs have been done and showed only trivial pericardial effusion.
Discussion
Purulent pericarditis is a rare condition in the modern world, especially with the introduction of antibiotics. There are multiple mechanisms of pathogenesis of purulent pericarditis, including spread of intrathoracic infectious focus, hematogenous spread or extension from subdiaphragmatic infection [4]. In the case of our patient there are two possible mechanisms: spread from an intrathoracic focus, given he had diagnosed with pneumonia, or hematogenous spread, possibly from the septic arthritis, as the blood cultures collected on admission grew Streptococcus pneumoniae. It is difficult to precisely pinpoint which disease process was the enticing event that caused the complication of purulent pericarditis in this patient.
Staphylococcus aureus is known to be the most common cause of purulent pericarditis, however S. pneumoniae is the most prevalent organism causing purulent pericarditis when the causative mechanism is spread from an infectious intrathoracic focus [4], which was the case in our patient.
Purulent pericarditis is typically acute in onset with high fever, tachycardia, chest pain and cough [5]. Our patient has had a sudden onset of chest pain along with cough and dyspnea and he was tachycardic on admission and even developed atrial fibrillation with rapid ventricular response during his hospitalization.
Diagnosis of purulent pericarditis is made by draining the pericardial fluid and sending it for analysis. Fluid analysis usually shows high protein concentration with low glucose and markedly elevated leukocytes. In our patient pericardial fluid glucose was less than 10 mg/dl, total protein 3.7 g/dl, with leukocytes over 46 thousand with neutrophilic predominance, which is consistent with a bacterial infection. Gram stain and culture of the fluid should also be performed, however they may be non-diagnostic if the patient was already started on antibiotics, as in our case.
The mainstem of treatment is pericardial drainage and use of antimicrobials [6]. One of the most used techniques is pericardiocentesis, but it might be difficult to perform if the pericardial fluid is thick or loculated. Other, more invasive techniques, include subxiphoid pericardiotomy, which allows for a more permanent drainage of pericardial fluid as well as manual lysis of any adhesions or loculations, however it is a more invasive procedure. Pericardiotomy carries more risks and has higher morbidity and mortality, it may be required in patients with recurrent tamponade and very dense adhesions. Video-assisted thoracic surgery (VATS) is an option for draining pericardial fluid, however it requires intubation and deflation the left lung and a chest incision, therefore has more risk and adds little benefit over subxiphoid pericardiotomy [6].
Our patient underwent pericardiocentesis with drainage of one liter of purulent fluids and with subsequent pericardial drain placement, which was removed successfully after several days. Antimicrobial therapy should cover for both gram-positive and gram-negative bacteria, with several possible combinations of antibiotics, for example Vancomycin and Ceftriaxone or a carbapenem or piperacillin-tazobactam, ampicillin-sulbactam or Cefepime. For severely immunocompromised patients, additional therapy with fluconazole is recommended in addition to antibiotics. Once a pathogen is identified the antimicrobial therapy should be narrowed to cover the specific pathogen. Duration of therapy is individualized but can range from two to six weeks. Our patient was initially started on broad spectrum antibiotics with Vancomycin and Cefepime, later switched to Ceftriaxone on which he was discharged for six weeks duration.
Purulent pericarditis is a disease with high mortality, up to 30% [7] if not treated promptly.
Conclusion
This case demonstrates purulent pericarditis in the setting of streptococcal pneumonia complicated by bacteremia, infective endocarditis, empyema, and septic arthritis. Purulent pericarditis is a rare entity in the modern era, however, can progress rapidly and be lethal, therefore requires rapid diagnosis and treatment.
Disclosures
The authors have nothing to disclose.
Funding
The authors did not receive any funding.
Informed Consent
Informed consent was obtained from the patient prior to writing the case report.
References
2. Kauffman CA, Watanakunakorn C, Phair JP. Purulent pneumococcal pericarditis. A continuing problem in the antibiotic era. Am J Med. 1973 Jun;54(6):743-50.
3. Klacsmann PG, Bulkley BH, Hutchins GM. The changed spectrum of purulent pericarditis: An 86 year autopsy experience in 200 patients. Am J Med. 1977;63:666-73.
4. Rubin R, Moellering Jr. R. Clinical, microbiologic and therapeutic aspects of purulent pericarditis. Am J Med. 1975 Jul;59(1):68-78.
5. Sagristà-Sauleda J, Barrabés JA, Permanyer-Miralda G, Soler-Soler J. Purulent pericarditis: Review of a 20-year experience in a general hospital. J Am Coll Cardiol. 1993;22:1661-5.
6. Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, Bogaert J, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015;36:2921-64.
7. Augustin P, Desmard M, Mordant P, Lasocki S, Maury J-M, Heming N, et al. Clinical review: Intrapericardial fibrinolysis in management of purulent pericarditis. Crit Care. 2011;15:220.