Commentary
As aquatic therapy has become an important rehabilitative option, more exercise programs have emerged. Ai Chi, is one of the therapeutic aquatic exercise concepts with growing potential. In our previous study, both types of aquatic exercise, Ai Chi and conventional exercise, supported the restoration of postural control in people with chronic stroke, whereas Ai Chi seemed to have larger effects [1]. Along with the statistically significant amelioration of weight shifting ability, number of participants who reached clinical fall risk cutoff score was also higher in Ai Chi group than in control group. We have attributed the advantages of Ai Chi to the unique combination of movement characteristics, such as postural challenge, closed-chain movements, and multi-joint involvement.
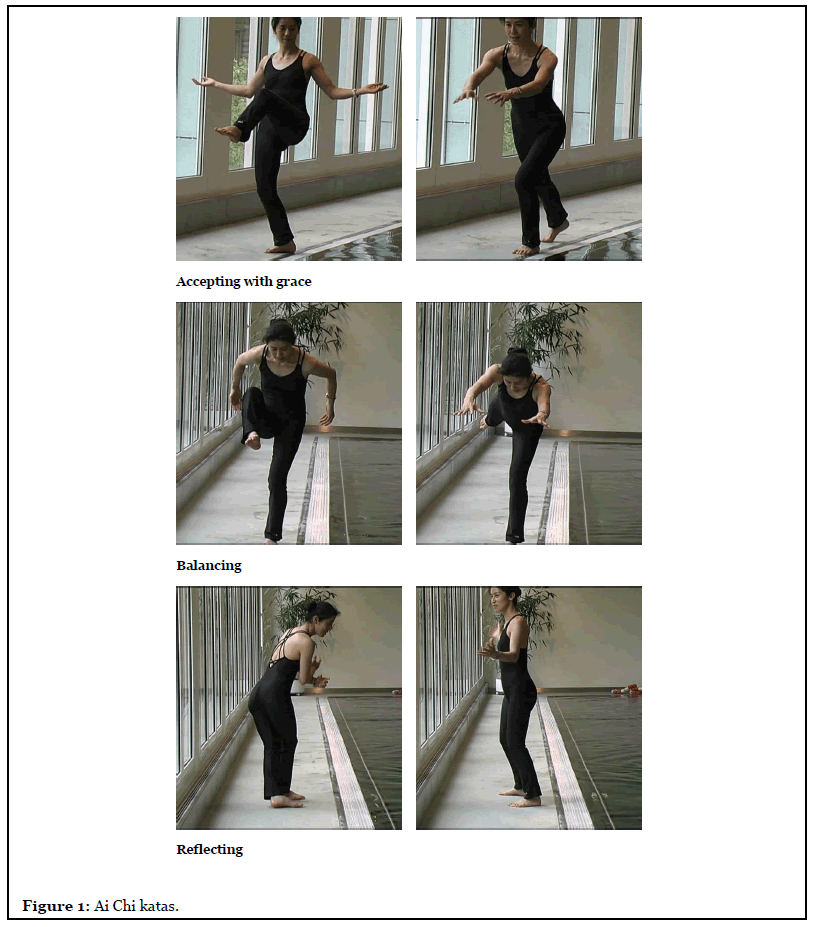
Over the decades, the number of studies using Ai Chi in stroke population is increasing. Ai Chi was mainly opted to target lower extremity movement and postural control [2]. The length of the intervention ranging from 4 weeks to 10 weeks and the session time varied from 30 to 60 minutes. The most common frequency was 2 to 3 times per week. Stroke frequently affects one side of the body, and therefore maintaining stability in water is expected to be challenging. In addition, potential muscle synergy, hyper- or hypotonicity, joint range limitation, and sometimes pain should always be closely observed. To provide a safe Ai Chi training, the therapist should understand the limitation in sensorimotor and cognitive functions. Incomplete movements due to restrictions in range of motion are adaptable in water. Buoyancy can well assist the movements especially for uplifting direction like abduction or flexion. It is possible for the therapist to stand aside or in front of the clients and to manually guide the movement of the hemiplegic side. In many cases, subjects tend to show increased muscles tone in the distal part (i.e. hands and feet). When the fingers and wrists are rigid and/or tight, it is recommended to start with the proximal parts (i.e. shoulder and trunk) and leave out the distal components in the beginning. However, if the subjects have difficulties keeping the feet on the floor when standing, the therapist can gently fix the feet with his/her own feet in the beginning. As long as the subjects start to develop control over lower extremity in Ai Chi katas, they should be encouraged to maintain balance without assistance. Katas involving single leg stance and weight shifting in anteroposterior axis, such as accepting with grace, rounding, and balancing, could be difficult for subjects with increased calf muscle tone and insufficient control of dorsiflexion and plantarflexion. Patients or clients usually need more time to acquire these katas with more assistance and cues from the therapist. However, these katas bear important components of selective movement control underweight support, and thus beneficial for breaking down the synergy patterns for individuals with hypertonicity. Other movements requiring trunk rotation over 90 degrees or crosswalk are particularly challenging due to lack of control in ankle movements, especially inversion and eversion. For example, patients/clients sometimes could only perform sidewalk instead of crosswalk in flowing and reflecting. The movement components are described in Table 1 and in the Supplementary Table in our previous study [1]. Examples of Ai Chi katas are demonstrated in Figure 1. The photos were reprinted with permission from International Aquatic Therapy Faculty (2005).
| Number | Kata (Movement) | Movement Category | Position | Balance Components |
|---|---|---|---|---|
| 1 | Contemplating | Breathing control | Wide stance, weight evenly distributed | Static balance: the center of gravity remains unchanged over wide base of support, with symmetrical upper extremity movements. |
| 2 | Floating | |||
| 3 | Uplifting | |||
| 4 | Enclosing | Trunk stability | ||
| 5 | Folding | |||
| 6 | Soothing | |||
| 7 | Gathering | Basic coordination | Lounge position | Dynamic balance (double-leg standing): the center of gravity starts to shift over narrowing base of support, and the upper extremity movements become asymmetrical. |
| 8 | Freeing | Change between wide stance and lounge position | ||
| 9 | Shifting | Wide stance, weight reciprocally shifted to left and right | ||
| 10 | Accepting | Lounge position, weight constantly shifted forward and backward | ||
| 11 | Accepting with grace | One leg standing | Dynamic balance (single-leg standing): the base of support reduces largely from double-leg to single-leg standing. Though the upper extremity are symmetrical, the challenge for balance has been greatly increased. | |
| 12 | Rounding | |||
| 13 | Balancing | |||
| 14 | Flowing | Advanced coordination | Walking with cross steps | Dynamic balance with complex gait patterns: sideway and cross-walk patterns are incorporated with upper extremity movements may or may not be on the same rhythm (leg-open with hand-open, or leg-open with hand-closed) |
| 15 | Reflecting | Walking with cross steps and rotation | ||
| 16 | Suspending | Jumping |
Table 1: Description and training components of each Ai Chi kata.
Ai Chi can also be applied to other populations than stroke. The characteristics of Ai Chi can be easily related to the populations with balance deficits, such as elderly [3,4], Parkinson’s disease (PD) [5-7], and multiple sclerosis (MS) [8,9]. According to previous studies, Ai Chi seemed to improve balance and functional mobility more than land-based exercise. For those who intend to improve balance and functional mobility, the session usually takes at least 35 minutes to 60 minutes at maximum. The frequency varies from once a week to daily with total of 20 sessions approximately. In general, elderly with balance deficits usually needs less time for intervention whereas individuals with neurological disease (such as PD and MS) require longer time in one intervention and more sessions in total in order to obtain clinical improvements. The design of Ai Chi program is based on similar principles as other exercise programs. The session routinely starts with 10 minutes of preparation, followed by the practice of Ai Chi sequence, and ends with another 10 minutes of relaxation. The sequence progresses from easy to more challenging katas. With many notable elements for postural control, Ai Chi is beneficial for people who can walk independently but with relatively high risks of fall [10]. For instance, a slow increase of the amplitude of the centre of gravity in the course of weeks for elderly or the focus on medio-lateral stability with prevention of crossover strategies during katas with lateral displacement for Parkinson patients [11].
Ai Chi can also be applied to other populations than stroke. The characteristics of Ai Chi can be easily related to the populations with balance deficits, such as elderly [3,4], Parkinson’s disease (PD) [5-7], and multiple sclerosis (MS) [8,9]. According to previous studies, Ai Chi seemed to improve balance and functional mobility more than land-based exercise. For those who intend to improve balance and functional mobility, the session usually takes at least 35 minutes to 60 minutes at maximum. The frequency varies from once a week to daily with total of 20 sessions approximately. In general, elderly with balance deficits usually needs less time for intervention whereas individuals with neurological disease (such as PD and MS) require longer time in one intervention and more sessions in total in order to obtain clinical improvements. The design of Ai Chi program is based on similar principles as other exercise programs. The session routinely starts with 10 minutes of preparation, followed by the practice of Ai Chi sequence, and ends with another 10 minutes of relaxation. The sequence progresses from easy to more challenging katas. With many notable elements for postural control, Ai Chi is beneficial for people who can walk independently but with relatively high risks of fall [10]. For instance, a slow increase of the amplitude of the centre of gravity in the course of weeks for elderly or the focus on medio-lateral stability with prevention of crossover strategies during katas with lateral displacement for Parkinson patients [11].
In addition to movement characteristics, Ai Chi, resembling Tai Chi, is also believed to involve cognitive functions [12]. Ai Chi requires the subjects to perform the movement while remembering the components and sequence of the movements simultaneously. It is a dualtask situation, causing motor-cognitive interference and providing cognitive challenges. Dual-task training can improve cognitive functions and particularly executive functions, which commonly declines in aging populations and people with neurological disorders [13,14]. Moreover, warm water immersion seems to induce cortical activation in sensorimotor areas, boosting the training effects [15]. Studies showed that simply standing in water would increase cerebral blood flow and improve the attenuation in sensorimotor areas [15-17]. The memory task performance of elderly was significantly better in the subjects standing in water than on land [18]. Assumingly, the effect of immersion, acting as priming effect, might be one of the factors to explain the prior training results of aquatic therapy. According to two studies of Nissim, Ai Chi is a feasible intervention for decreasing fall risks by improving balance and working memory [19,20]. These results showed that the beneficial effects of Ai Chi are not confined to motor perspectives.
People with orthopaedic problems could be a good example for Ai Chi application on populations other than neurological disorders. People with non-specific chronic/ recurrent low back pain tend to stiffen their low back and rely heavily on ankle strategy even when such strategy is not the most appropriate choice [21]. Instead, the hip strategy sometimes would be a functional choice for preventing fall. Therefore, the focus and practice on hip strategies is an emphasis during intervention [21]. Ai Chi including katas that fulfill the definition of the anterior-posterior hip control can be used to retrain the hip strategies, and such effects can also be enhanced by the properties of water on fascia extensibility.
Fascia is the dense irregular connective tissue sheets including aponeuroses, joint capsules, or endo-, peri- , and epi-mysium [22]. Covering large area of the musculoskeletal system, fascia plays an important role in providing stability [23], allowing mobility [24], and supporting force and transmission [24,25]. Ai Chi, with the abovementioned characteristics, might be able to address fascial issues. For instance, extensibility of the dorsal deep fascia measured with the finger-floor-test (FFT) [26] was improved after receiving regular care plus Ai Chi sessions, while the extensibility was not increased in those who only received regular care [9]. However, such increase of extensibility (3.8cm) was slightly less than the minimal detectable change (4.5cm) [27]. The small increase might be due to the inelastic properties of dense layers of collagenous fibers which are the major components of extra-muscular part of the dorsal deep fascia. However, slow movement with low force is suggested to augment intramuscular thixotropic changes [28]. Therefore, in addition to possible thixotropic changes, Ai Chi may also increase the expression of nitric oxide resulting in fascia relaxation by water immersion [22,29].
These immersion and movement effects on fascia also could affect interstitial fluid flow as seen in lymphedema after breast cancer surgery. Complete decongestive therapy (CDT) is the gold standard of lymphedema management [30]. Elements are strength training and elongation exercises during first 3 months post-surgery, staring with a low training intensity: slow, smooth, controlled and repetitive. Ai Chi would satisfy this description. Originally, Ai Chi is about stretching meridians, which coincides with the increase of tensile forces on fascia [31]. Every of the 20 kata’s in Ai Chi includes arm movements under the water surface, but adaptations will need to elevate the arm above water, leading to an alternation of hydrostatic pressure and gravity forces, both affecting interstitial hypervolume/lymphedema. Hydrostatic pressure effects on lymphedema have been described by Ambroza & Geigle [32] and Tidhar & Katz-Leurer [33]. Recently, Deacon et al. [34] compared slow paced Ai Chi movements (30-45°/ sec) with conventional aquatic therapy which contained movements twice as fast in women with breast cancer related lymphedema (BCRL). The results showed that Ai Chi is a viable and more effective form of therapy for arm volume reduction in women with BCRL. Other Ai Chi adaptations in CDT like starting the movement sequence of the arms with proximal joints instead of the distal ones as described in the classical way, the inclusion of explicit deep abdominal breathing or the focus on thoracic movements in order to influence the sympathetic innervation of vasculature in the upper part of the body need to be established. The possible indications for Ai Chi are listed in Table 2.
| Impairments | Functional limitations |
|---|---|
| Decreased joint mobility Decreased joint stability | Decreased static standing balance |
| Decreased muscle strength | Decreased dynamic standing balance |
| Decreased muscle flexibility |
Decreased postural control |
| Decreased muscle endurance | Decreased transferring ability |
| Abnormal muscle tonicity | Decreased walking ability |
| Synergistic patterns | Decreased dual task performance |
| Insufficient movement control |
|
| Insufficient movement coordination |
|
| Increased pain | |
| Lack of isolated movements (e.g. due to pain) | |
| Decreased fascia extensibility | |
| Decreased facia mobility | |
| Adhesive tissues | |
| Decreased executive functions | |
| Lymphoedema |
Table 2: Indications of Ai Chi.
Overall, the benefits of Ai Chi could be attributed to two major reasons: the effects of water immersion, and the characteristics of the movement patterns. Many positive effects of accumulative Ai Chi training were found in literature. First, Ai Chi contains various standing positions and requires constant control or shift of center of gravity, which makes Ai Chi an ideal training for people with balance deficits. It has been applied in elderly, and people with certain neurological or orthopedic disorders. Second, the stretch and slowness in the movement might exert benefits on increasing extensibility of fascia, and decreasing lymphoedema of people with breast cancer. Third, the influence of immersion should not be overlooked. Brain activation may alter due to hydrostatic pressure, leading to possible effects on cognitive function. Water immersion might be able to boost the effect of Ai Chi, or any aquatic therapy. Further physiological regulations and mechanisms of Ai Chi are yet to be explored.
Acknowledgement
This work was supported by grants from the National Health Research Institutes (NHRI-EX109-10913PI) and the Ministry of Science and Technology (MOST 106-2314-B-010-040-MY3).
References
2. Morris DM. Aquatic therapy to improve balance dysfunction in older adults. Topics in Geriatric Rehabilitation. 2010 Apr 1;26(2):104-19.
3. Covill LG, Utley C, Hochstein C. Comparison of ai chi and impairment-based aquatic therapy for older adults with balance problems: a clinical study. Journal of Geriatric Physical Therapy. 2017 Oct 1;40(4):204-13.
4. Olabe Sánchez PJ. Repercusión del Ai Chi en el equilibrio de las personas mayores. European Journal of Investigation in Health, Psychology and Education. 2014; 4(3):247-256.
5. Kurt EE, Büyükturan B, Büyükturan Ö, Erdem HR, Tuncay F. Effects of Ai Chi on balance, quality of life, functional mobility, and motor impairment in patients with Parkinson’s disease. Disability and Rehabilitation. 2018 Mar 27; 40(7):791-7.
6. Pérez-de la Cruz S. A bicentric controlled study on the effects of aquatic Ai Chi in Parkinson disease. Complementary Therapies in Medicine. 2018 Feb 1; 36:147-53.
7. Pérez-de la Cruz S, Luengo AG, Lambeck J. Effects of an Ai Chi fall prevention programme for patients with Parkinson’s disease. Neurología (English Edition). 2016 Apr 1;31(3):176-82.
8. Bayraktar D, Guclu-Gunduz A, Yazici G, Lambeck J, Batur-Caglayan HZ, Irkec C, et al. Effects of Ai-Chi on balance, functional mobility, strength and fatigue in patients with multiple sclerosis: a pilot study. NeuroRehabilitation. 2013 Jan 1;33(3):431-7.
9. Castro-Sánchez AM, Matarán-Peñarrocha GA, Lara- Palomo I, Saavedra-Hernández M, Arroyo-Morales M, Moreno-Lorenzo C. Hydrotherapy for the treatment of pain in people with multiple sclerosis: a randomized controlled trial. Evidence-Based Complementary and Alternative Medicine. 2012 Oct;2012.
10. Skinner EH, Dinh T, Hewitt M, Piper R, Thwaites C. An Ai Chi-based aquatic group improves balance and reduces falls in community-dwelling adults: a pilot observational cohort study. Physiotherapy Theory and Practice. 2016 Nov 16;32(8):581-90.
11. King LA, Horak FB. Lateral stepping for postural correction in Parkinson’s disease. Archives of Physical Medicine and Rehabilitation. 2008 Mar 1;89(3):492-9.
12. Miller SM, Taylor-Piliae RE. Effects of Tai Chi on cognitive function in community-dwelling older adults: a review. Geriatric Nursing. 2014 Jan 1;35(1):9-19.
13. Al-Yahya E, Dawes H, Smith L, Dennis A, Howells K, Cockburn J. Cognitive motor interference while walking: a systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews. 2011 Jan 1;35(3):715-28.
14. Fritz NE, Cheek FM, Nichols-Larsen DS. Motorcognitive dual-task training in neurologic disorders: a systematic review. Journal of Neurologic Physical Therapy: JNPT. 2015 Jul;39(3):142.
15. Sato D, Onishi H, Yamashiro K, Iwabe T, Shimoyama Y, Maruyama A. Water immersion to the femur level affects cerebral cortical activity in humans: functional near-infrared spectroscopy study. Brain Topography. 2012 Apr 1;25(2):220-7.
16. Sato D, Yamashiro K, Onishi H, Shimoyama Y, Yoshida T, Maruyama A. The effect of water immersion on short-latency somatosensory evoked potentials in human. BMC Neuroscience. 2012 Dec 1;13(1):13.
17. Pugh CJ, Sprung V, Ono K, Spence A, Thijssen D, Carter H, et al. The effect of water immersion during exercise on cerebral blood flow. Medicine and Science in Sports and Exercise. 2015; 47(2): 299-306.
18. Bressel E, Louder TJ, Raikes AC, Alphonsa S, Kyvelidou A. Water immersion affects episodic memory and postural control in healthy older adults. Journal of Geriatric Physical Therapy. 2019 Oct 1;42(4):E1-6.
19. Nissim M, Livny A, Barmatz C, Tsarfaty G, Berner Y, Sacher Y, et al. Effects of aquatic physical intervention on fall risk, working memory and hazard-perception as pedestrians in older people: a pilot trial. BMC Geriatrics. 2020 Dec;20(1):1-2.
20. Nissim M, Hutzler Y, Goldstein A. A walk on water: comparing the influence of Ai Chi and Tai Chi on fall risk and verbal working memory in ageing people with intellectual disabilities–a randomised controlled trial. Journal of Intellectual Disability Research. 2019 Jun;63(6):603-13.
21. Brumagne S, Janssens L, Knapen S, Claeys K, Suuden- Johanson E. Persons with recurrent low back pain exhibit a rigid postural control strategy. European Spine Journal. 2008 Sep 1;17(9):1177-84.
22. Schleip R, Klingler W, Lehmann-Horn F. Active fascial contractility: fascia may be able to contract in a smooth muscle-like manner and thereby influence musculoskeletal dynamics. Medical Hypotheses. 2005 Jan 1;65(2):273-7.
23. Cheung JT, Zhang M, An KN. Effects of plantar fascia stiffness on the biomechanical responses of the ankle–foot complex. Clinical Biomechanics. 2004 Oct 1;19(8):839-46.
24. Barker PJ, Briggs CA, Bogeski G. Tensile transmission across the lumbar fasciae in unembalmed cadavers: effects of tension to various muscular attachments. Spine. 2004 Jan 15;29(2):129-38.
25. Huijing PA. Muscle as a collagen fiber reinforced composite: a review of force transmission in muscle and whole limb. Journal of Biomechanics. 1999 Apr 1;32(4):329-45.
26. Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou MA, Revel M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Archives of Physical Medicine and Rehabilitation. 2001 Nov 1;82(11):1566-70.
27. Ekedahl H, Jönsson BO, Frobell RB. Fingertip-to-floor test and straight leg raising test: validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Archives of Physical Medicine and Rehabilitation. 2012 Dec 1;93(12):2210-5.
28. Nuyens GE, De Weerdt WJ, Spaepen Jr AJ, Kiekens C, Feys HM. Reduction of spastic hypertonia during repeated passive knee movements in stroke patients. Archives of Physical Medicine and Rehabilitation. 2002 Jul 1;83(7):930-5.
29. Karaarslan F, Ozkuk K, Karabulut SS, Bekpinar S, Karagulle MZ, Erdogan N. How does spa treatment affect cardiovascular function and vascular endothelium in patients with generalized osteoarthritis? A pilot study through plasma asymmetric di-methyl arginine (ADMA) and L-arginine/ADMA ratio. International Journal of Biometeorology. 2018 May 1;62(5):833-42.
30. Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, et al. Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Medicine & Science in Sports & Exercise. 2019 Nov 1;51(11):2375-90.
31. Bai Y, Yuan L, Soh KS, Lee BC, Huang Y, Wang CL, et al. Possible applications for fascial anatomy and fasciaology in traditional Chinese medicine. Journal of Acupuncture and Meridian Studies. 2010 Jun 1;3(2):125-32.
32. Ambroza C, Geigle PR. Aquatic Exercise as a Management Tool for Breast Cancer–Related Lymphedema. Topics in Geriatric Rehabilitation. 2010 Apr 1;26(2):120-7
33. Tidhar D, Katz-Leurer M. Aqua lymphatic therapy in women who suffer from breast cancer treatment-related lymphedema: a randomized controlled study. Supportive Care in Cancer. 2010 Mar 1;18(3):383-92.
34. Deacon R, de Noronha M, Shanley L, Young K. Does the speed of aquatic therapy exercise alter arm volume in women with breast cancer related lymphoedema? A crossover randomized controlled trial. Brazilian Journal of Physical Therapy. 2019 Mar 1;23(2):140-7.
