Abstract
Dyspnea and reduced exercise capacity negatively affect the quality of life in many Chronic Obstructive Pulmonary Disease (COPD) patients with emphysema phenotype. Surgical procedures may be preferred in cases where improvement in respiratory functions cannot be achieved despite pharmacological treatments. These surgical operations are bullectomy, lung transplantation, lung volume reduction surgery (LVRS) or bronchoscopic lung volume reduction (BLVR). Pulmonary rehabilitation (PR) is a well-established and widely accepted standard therapy in order to alleviate symptoms and optimize pulmonary functions. It is stated in the guidelines and reports that receiving of PR before the bronchoscopic interventions is a necessity. Moreover, there are very few studies on this subject. In this review, PR will be discussed in relation to BLVR.
Keywords
Coil, Dyspnea, Exercise, Physiotherapy, Valve
Emphysema and Hyperinflation
The main symptom in Chronic Obstructive Pulmonary Disease (COPD) is shortness of breath. Shortness of breath occurs especially with exercise and progresses over the years despite all medical treatments. One of the main mechanisms by which this symptom occurs is hyperinflation in the lungs [1].
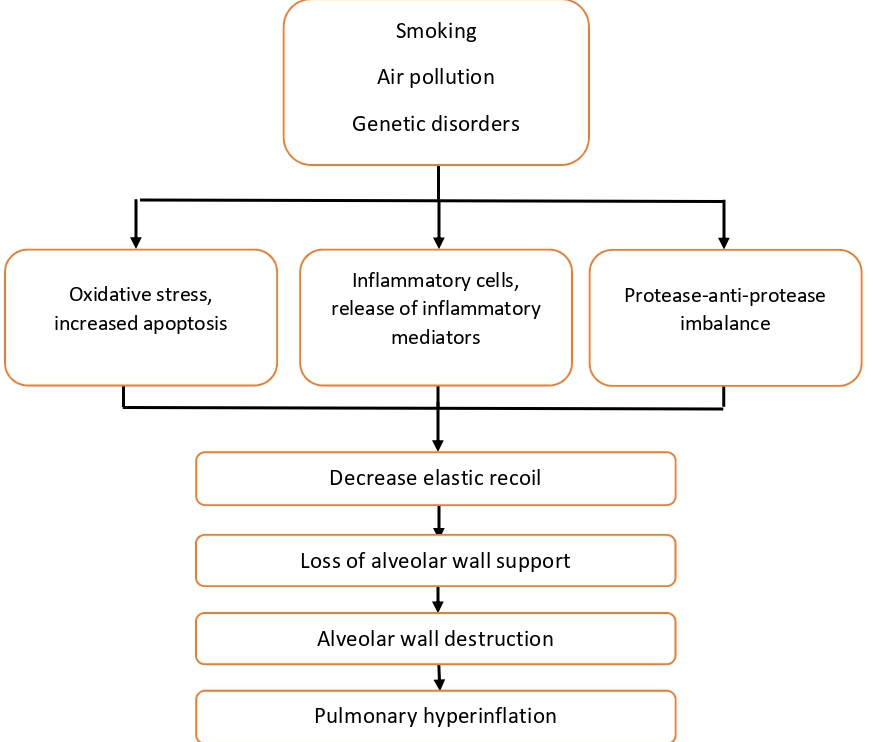
Hyperinflation is divided into two as static and dynamic pulmonary hyperinflation according to its physiopathogenesis. Emphysema is the most common cause of static hyperinflation. Lung parenchymal damage and loss of elastic recoil cause static lung hyperinflation. Loss of elastic fibers in the alveolar wall leads to a decrease in elastic recoil strength, loss of alveolar wall support structures, and premature closure of the airways during expiration. As a result, end expiratory lung volume, i.e. residual volume increases [2]. Emphysema and lung hyperinflation mechanism are schematized in Figure 1.
Figure1: Pathogenesis of emphysema and lung hyperinflation.
During exercise, before the alveolar air is fully exhaled, the initiation of inhalation causes dynamic lung hyperinflation. The increase in residual volume at rest becomes more pronounced with effort. The result is air trapping, or dynamic hyperinflation, which becomes much more exaggerated with exercise. The lungs, which become excessively swollen with dynamic hyperinflation, cannot stretch anymore. It becomes difficult for the patient to breath deeply, and the work of breathing increases. Respiratory muscles are strained due to increased air trapping and as a result, respiratory functions are impaired. Respiratory muscle fatigue develops. The clinical reflection of all this is shortness of breath and a decrease in functional capacity [3].
While the dynamic hyperinflation treatment is based on smoking cessation, bronchodilator drug therapy and PR, these treatments are insufficient in many patients. Lung transplantation (LTx) and Lung Volume Reduction Surgery (LVRS) are currently available for a selected group of patients. Endoscopic alternatives to LVRS have progressively gained acceptance and are currently employed in patients with emphysema.
Bronchoscopic Lung Volume Reduction mechanism
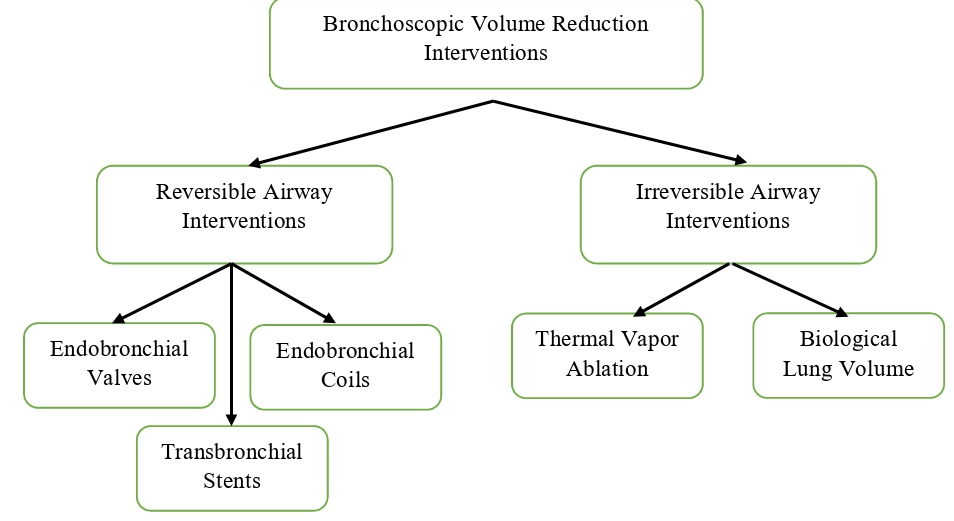
Due to the high morbidity and mortality rates in both LTx and LVRS, minimally invasive methods have come to the fore in order to reduce the lung volume in patients with emphysema. Bronchoscopic lung volume reduction (BLVR) may be considered in COPD patients with advance emphysema who are symptomatic and have refractory hyperinflation despite optimal medical therapy and PR [4]. The pathophysiological principles of the LVRS is to removel the worst affected parts of the emphysematous lung, which helps to normalize the diaphragmatic and chest wall mechanics [5]. On the other hand the BLVR interventions acts based on a different physiological mechanism. They can be evaluated in two groups. The first group is reversible airway interventions. This group includes endobronchial valves, endobronchial coils and transbronchial stents. Interventional substances used in this group could potentially be withdrawn if complications develop. The second group includes irreversible airway interventions such as thermal vapor ablation and biological lung volume reducton that act by inducing an inflammatory / fibrotic response or permanent obstruction of the distal airways [6] (Figure 2).
Figure 2: Bronchoscopic Volume Reduction Interventions.
Bronchoscopic lung volume reduction reduces air trapping, corrects elastic recoil, increases expiratory flow, and enables the rib cage and diaphragm to function more effectively by re-establishing the normal relationship between the lungs and the chest wall. Clinically, dyspnea decreases, exercise capacity increases, and improvement in all components of quality of life is achieved [7]. In a retrospective study, it was reported that the cases who underwent BLVR had longer surveillance compared to those who did not receive BLVR [8].
BLVR patient selection is important for the success of the procedure and patient safety. FEV1 and DLCO are key inclusion and exclusion parameters used to determine eligibility for surgery and/or bronchoscopic intervention. In patients with high exercise capacity and non-upper lobe emphysema distribution, LVRS was found to be more mortal than medical therapy alone. LVRS should not be recommended for these patients [9]. Disease phenotype, exercise capacity, FEV1 and the presence of collateral circulation should be taken into account in the selection of BLVR patients [10]. UK National Institute for Healthcare Excellence (NICE) guidance states that lung volume reduction treatment option should be considered in COPD cases with FEV1 less than 50%, 6-minute walking distance below 140 meters and shortness of breath worsens the quality of life (Medical Research Council dyspnoea score of ≥ 4) [11]. A study examining the NICE criteria reported that a thershold value of 140 meters is appropriate [12]. Therefore, if exercise capacity increases with PR before undergoing BLVR, there is no need for bronchoscopic procedures with a high complication rate and high cost, and the disease management can only be done with medical treatment. This information has made it a necessity to undergoing PR before BLVR.
Why is There a Need for Pulmonary Rehabilitation in Bronchoscopic Lung Volume Reduction?
The 2016 Expert Panel Report on Endoscopic Lung Volume Reduction focused on the patient selection and discussed available endoscopic techniques [4]. In 2017, researchers indicated that patients should receive optimal medical therapy as defined by the Global Initiative for Chronic Obstructive Lung Disease [13] and they have completed PR or a structured physical therapy program, and quit smoking definitively [14]. Despite this report, there are no studies supporting the importance of PR in volume reduction operations. It is highly probable that the statement in the report was created by considering the effect of PR on COPD and LVRS cases. Such patients typically have severe ventilatory limitation and disability and are at high risk of preoperative and postoperative complications. In COPD cases, PR increases exercise capacity and quality of life and reduces dyspnea [15,16]. It has been revealed that PR in LVRS cases increases exercise tolerance and muscle function [17]. PR in addition to LVRS, improves static lung function, gas exchange, and quality of life compared with PR alone [18].
Pulmonary rehabilitation administered before LVRS is safe and effective [9,19]. In the The National Emphysema Treatment Trial (NETT) study, PR led to significant improvements in peak exercise workload, walking endurance, dyspnea, and quality of life [9]. Improvements in peak aerobic capacity and muscle strength can also result from PR before LVRS [19].
In the Bronchoscopic expert panel [20] published in 2019, attention was drawn to the existence of only 2 PR clinical studies on this subject. Of these, Solve trial (NCT03474471) is still in recuiting status. The other study is prospective randomized controlled study in which and hospital-based versus home-based PR gains were compared (The study is discussed in the section “Pulmonary rehabilitation before bronchoscopic lung volume reduction”) [21].
Pulmonary Rehabilitation Content in Bronchoscopic Lung Volume Reduction
The content of PR that should be administered in BLVR is not clear. Pulmonary rehabilitation program content for individuals preparing for BLVR or LVRS generally follows existing PR guidelines for individuals with COPD. Pulmonary rehabilitation program content for individuals preparing for the prosedure includes chest hygiene techniques, breathing exercises, aerobic and strengthening training and education [22]. The educational component includes detailed explanations of the procedure and post prosedural mobilization processes. After the prosedure, PR includes progressive mobilization, breathing exercises and bronchial clearance technics.
Pulmonary Rehabilitation before Bronchoscopic Lung Volume Reduction
The necessity of receiving PR or structured physical therapy program before BLVR has caused rehabilitation strategies to be included in the treatment routines of these cases. In contrast, there are very few clinical studies on PR efficiancy before BLVR. In our literature review, we found only one published study about PR before BLVR [21]. The study is a prospective, randomized, controlled study. Patients received either home-based or hospital-based PR for 8 weeks. Hospital-based group program involved 8 weeks of twice-weekly supervised sessions; it included education, breathing exercises, treadmill walking, cycle ergometer, arm ergometer training and strengthening training. Exercise intensity was predetermined to be 80% of the maximum heart rate, and it was gradually increased taking the severity of dyspnea perception and fatigue ratio as the basis. Strengthening training was recommended over resistance targets which were set at loads equivalent to 40% of a 1-repetition maximum (1RM). Home-based group program included education, breathing exercises, upper and lower extremity strenghthening exercise with free weights and free walking for at least four days weekly during the eight weeks. It was recommended that resistance targets were set at loads equivalent to 40% of a 1RM. Daily free walking is recommended for all patients. The method of the calculating number of free walking laps based on the six-minute walk test. This study, demonstrated that both home-based and hospital-based PR provided significant and similar improvements in the dyspnea and symptom scores but exercise capacity was only significantly increased in the hospital-based PR [21].
Apart from the aforementioned study, there is another trial, clinical number NCT04347044 that has not been published yet. The study is a retrospective parallel design study. The data of patients undergoing BLVR intervention will be analyzed retrospectively. Patients will be divided into two groups as patients with and without PR before the procedure, and changes in functional levels of patients will be compared. The importance of the study is that there is a control group in which PR was not received before the procedure. With the publication of the article, it is thought that supportive information about the importance of PR before volume reduction operations may emerge.
Pulmonary Rehabilitation after Bronchoscopic Lung Volume Reduction
There is only one study published on the effectiveness of PR after BLVR [23]. In the study, the effect of PR on pulmonary functions and exercise capacity was examined. Pulmonary rehabilitation program was an in-hospital, multidisciplinary, 4-week intervention that included optimization of the pharmacologic treatment and a 3-h session daily consisting of supervised incremental exercise until achieving 30 min of continuous cycling or treadmill walking at 50-70% of the maximal load calculated based on the initial 6-min walking test. The muscle trainning content included abdominal, upper and lower-limb muscle exercise with supported and unsupported activities (lifting progressively increasing lightweights, 300 to 500 g), shoulder, and full arm circling. In addition to these, there were patient and family education lessons and nutritional and psychosocial counseling, when appropriate. As a result of the study, it was revealed that BLVR increases pulmonary functions and exercise tolerance [23].
It should not be forgotten that complications such as COPD exacerbation, chest pain, mild bleeding, pneumonia, pneumothorax (px), and respiratory failure may develop after BLVR [24]. In a study, it was reported that in emphysema cases with an FEV1 of less than 20%, px developed in 20% of the cases who underwent BLVR [25]. Possible complications should be taken into consideration especially in the application of respiratory exercises and chest hygiene techniques.
Future Directions
More studies are needed to emphasize the effectiveness and importance of PR before and after BLVR. It is a handicap that it is not possible to conduct a prospective randomized study with a control group without PR, since PR has become a necessity before LVRS or BLVR and is included in the guidelines. On the other hand, new studies should be conducted in larger case pools to design a specific program for these cases.
Based on the foregoing we can draw the following conclusions:
• It is a necessity for patients to be included in the PR program before undergoing BLVR.
• Symptomatic improvement and increase in exercise capacity are achieved with PR before and after BLVR.
• Different PR organization models can be applied to these patients, but according to the available data, hospital-based PR programs seem to be more effective in these cases.
Conflict of Interest Statement
The work has not been published before in any language, is not being considered for publication elsewhere, and has been read and approved by author. There are no conflicts of interest around this study.
References
2. van Geffen WH, Kerstjens HA. Static and dynamic hyperinflation during severe acute exacerbations of chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease. 2018;13:1269-77.
3. O’Donnell DE. Hyperinflation, dyspnea, and exercise intolerance in chronic obstructive pulmonary disease. Proceedings of the American Thoracic Society. 2006;3(2):180-4.
4. Herth FJF, Slebos DJ, Criner GJ, Shah PL. Endoscopic Lung Volume Reduction: An Expert Panel Recommendation - Update 2017. Respiration; International Review of Thoracic Diseases. 2017;94(4):380-8.
5. Lefrak SS, Yusen RD, Trulock EP, Pohl MS, Patterson A, Cooper JD. Recent advances in surgery for emphysema. Annual Review of Medicine. 1997;48:387-98.
6. Trotter MA, Hopkins PM. Advanced therapies for COPD-What’s on the horizon? Progress in lung volume reduction and lung transplantation. Journal of Thoracic Disease. 2014;6(11):1640-53.
7. Fessler HE, Scharf SM, Ingenito EP, McKenna RJ, Jr., Sharafkhaneh A. Physiologic basis for improved pulmonary function after lung volume reduction. Proceedings of the American Thoracic Society. 2008;5(4):416-20.
8. Welling JBA, Hartman JE. Patient Selection for Bronchoscopic Lung Volume Reduction. 2020;15:871-81.
9. Ries AL, Make BJ, Lee SM, Krasna MJ, Bartels M, Crouch R, et al. The effects of pulmonary rehabilitation in the national emphysema treatment trial. Chest. 2005;128(6):3799-809.
10. Gordon M, Duffy S, Criner GJ. Lung volume reduction surgery or bronchoscopic lung volume reduction: is there an algorithm for allocation? Journal of Thoracic Disease. 2018;10(Suppl 23):S2816-S23.
11. Hopkinson NS, Molyneux A, Pink J, Harrisingh MC. Chronic obstructive pulmonary disease: diagnosis and management: summary of updated NICE guidance. BMJ. 2019;366:l4486.
12. Buttery SC, Lewis A, Kemp SV, Banya W, Quint JK, Steiner MC, et al. Lung volume reduction eligibility in patients with COPD completing pulmonary rehabilitation: results from the UK National Asthma and COPD Audit Programme. BMJ Open. 2020;10(11):e040942.
13. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report: GOLD Executive Summary. The European Respiratory Journal. 2017;49(3):1700214.
14. van Agteren JE, Hnin K, Grosser D, Carson KV, Smith BJ. Bronchoscopic lung volume reduction procedures for chronic obstructive pulmonary disease. The Cochrane Database of Systematic Reviews. 2017;2:CD012158.
15. Pehlivan E, Yazar E, Balci A, Kilic L. Comparison of Compliance Rates and Treatment Efficiency in Home Based with Hospital-Based Pulmonary Rehabilitation in COPD. Turkish Thoracic Journal. 2019;20(3):192-7.
16. Deepak TH, Mohapatra PR, Janmeja AK, Sood P, Gupta M. Outcome of pulmonary rehabilitation in patients after acute exacerbation of chronic obstructive pulmonary disease. The Indian Journal of Chest Diseases & Allied Sciences. 2014;56(1):7-12.
17. Rochester CL. Pulmonary rehabilitation for patients who undergo lung-volume-reduction surgery or lung transplantation. Respiratory Care. 2008;53(9):1196-202.
18. Criner GJ, Cordova FC, Furukawa S, Kuzma AM, Travaline JM, Leyenson V, et al. Prospective randomized trial comparing bilateral lung volume reduction surgery to pulmonary rehabilitation in severe chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1999;160(6):2018-27.
19. Debigaré R, Maltais F, Whittom F, Deslauriers J, LeBlanc P. Feasibility and efficacy of home exercise training before lung volume reduction. Journal of Cardiopulmonary Rehabilitation. 1999;19(4):235-41.
20. Herth FJF, Slebos DJ, Criner GJ, Valipour A, Sciurba F, Shah PL. Endoscopic Lung Volume Reduction: An Expert Panel Recommendation - Update 2019. Respiration; International Review of Thoracic Diseases. 2019;97(6):548-57.
21. Pehlivan E, Yazar E, Balci A, Turan D, Demirkol B, Cetinkaya E. A comparative study of the effectiveness of hospital-based versus home-based pulmonary rehabilitation in candidates for bronchoscopic lung volume reduction. Heart & Lung : The Journal of Critical Care. 2020.
22. Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/ European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. American Journal of Respiratory and Critical Care Medicine. 2013;188(8):e13- 64.
23. Bianchi L, Bezzi M, Berlendis M, Marino S, Montini A, Paneroni M, et al. Additive effect on pulmonary function and disability of intensive pulmonary rehabilitation following bronchoscopy lung volume reduction (BLVR) for severe emphysema. Respiratory Medicine. 2018;143:116- 22.
24. Gulsen A. Bronchoscopic lung volume reduction using coil therapy: complications and management. Advances in Respiratory Medicine. 2020;88(5):433-42.
25. Darwiche K, Karpf-Wissel R, Eisenmann S, Aigner C, Welter S, Zarogoulidis P, et al. Bronchoscopic Lung Volume Reduction with Endobronchial Valves in Low- FEV1 Patients. Respiration; International Review of Thoracic Diseases. 2016;92(6):414-9.