Abstract
Introduction: Ischemic optic neuropathies are prevalent diseases and important cases of vision loss. In particular, non arteritic ischemic optic neuropathy (NAION) is the most common cause of optic neuropathy after 50 years of age and the etiology of NAION involves risk factors from the patients and some drugs as triggers, like triptans, selective agonists of 5-HT1 receptors. The use of triptans also has few associations with NAION in the literature, making the report of this case important to improve the clinical suspicion of this entity on migraine patients and highlights the importance of correct use of these medications.
Case report: We report a case of a 50-year-old woman with no cardiovascular risk factors. She had a history of seven consecutive days of migraine attacks and abuse of triptans. Two days after improving her headache and keep taking Naratriptan, she awoke in the morning with unilateral painless altitudinal visual deficit, with neurological and fundoscopic examination compatible with NAION.
Conclusion: This case is important to show us the correlation of migraine and ischemic optic neuropathy, but also to show the correlation of triptans, used for migraine treatment, with NAION.
Keywords
Optic neuropathy, Triptans, Migraine, Case report
Introduction
Ischemic optic neuropathy, defined by a damage to the optic nerve secondary to ischemia, is the most common optic neuropathy after 50 years of age [1]. The most common site of ischemic insult to the optic nerve is in its anterior portion, named anterior ischemic optic neuropathy (AION) and, when it afflicts the posterior portion, it is called posterior ischemic optic neuropathy (PION). The AION may be divided also by the etiology of the ischemia: on arteritic anterior ischemic optic neuropathy (AAION) and NAION. NAION is much more common than AAION, and AAION is usually secondary to giant cell arteritis [1].
There are some risk factors for NAION, like patients who have crowded nerve heads with small optic cups, cardiovascular risk factors like diabetes mellitus, hypertension, and some drugs (most commonly associated with amiodarone and phosphodiesterase inhibitors) [1].
The relationship between migraine and ischemic optic neuropathy is uncertain, and the disease may be a risk factor for NAION, especially in younger patients [1]. There are few case reports of this association. Selective agonist of serotonin 5-HT1 receptor (triptans) are drugs commonly used to treat migrainous attacks, and the correlation of triptans abuse and ischemic optic neuropathies are even less described in the literature, highlighting the importance to describe the correlation of, not only the disease, but also its treatment as a possible trigger to a patient’s vision loss, because the correct identification of this correlation lead to a correct diagnosis and follow up.
Case Report
A 50-year-old female patient had sudden loss of visual acuity upon awakening. The patient had a history of migraine-type headache, with frequent attacks in recent days, and had taken Naratriptan 5 mg/day orally for pain relief for seven consecutive days before the current clinical presentation, exceeding the dose limitations and number of consecutive days using the drug. She had no cardiovascular risk factors. Before the onset of vision loss, she did not have any headache for two days, but kept on taking triptans, afraid of rebound headaches. She was using no migraine prophylactic medication at the moment. She was notably afflicted with the acute and painless vision loss, going to multiple emergency departments.
Her neurological examination revealed an afferent pupillary defect in the left eye and an inferior altitudinal defect in the same eye. Visual acuity with correction for distance on the right eye was 20/20 and the left eye was 20/80.
Fundoscopic examination showed a collapsed retina in both eyes. In the left eye, there was hyperemic and poorly delimited optic nerve with edema in all its extension, making it difficult to quantify excavations. The right eye showed no abnormalities.
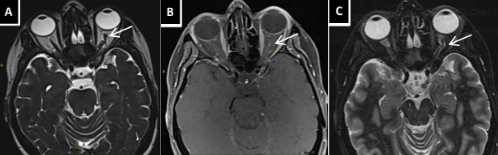
Cerebral MRI with orbital study showed signs of left optic nerve papillitis without alteration of signal intensity, suggesting NAION (Figure 1). Her inflammatory panel, consisting of c reactive protein and erythrocyte sedimentation rate were normal, and she had no clinical profile that suggested giant cell arteritis. Her coagulation blood tests with prothrombin time, thrombin time and screening for coagulation disorders were unremarkable. There were no cardiovascular risk factors detected, and there was no evidence of systemic vascular disease.
Figure 1. (A) Axial Stir - Protrusion of the left optic nerve head; (B) Axial T1 gadolinium enhanced - Optic nerve impregnation; (C) Axial T2 Flair -Tortuosity of the intraorbital division of the optic nerve.
Antiplatelet therapy was introduced and Naratripan was discontinued. The patient showed progressive improvement of vision in the left eye after the drug was discontinued. She was discharged 5 days after admission, presenting with visual clouding in left eye with lower altitudinal predominance and in a "crescent moon" character with upward concavity.
Discussion
NAION is a multifactorial disease involving an ischemic process resulting from microvascular disease that impairs the blood supply to the optic nerve. The clinical manifestation is characterized by a sudden, unilateral, and painless vision loss, more common upon awakening. The incidence is higher on male patients and on patients older than 50 years old.
There are few case reports of migrainous ischemic optic neuropathy [2,3], the possible mechanism of the migraine related cases is transient focal neurological dysfunction that affects the anterior pathways of the vision, causing ischemic optic neuropathy [2]. The case reports of this association are more common in patients with visual aura, and during migraine attacks [3]. In our case, despite the frequent migraine episodes during the week (mostly without aura), the vision loss occurred on a period without headache or aura, and the main hypothesis was the abuse of triptans, because of the overdosage and the number of consecutive days using the drug.
Some commonly prescribed drugs have been described as a trigger for ischemic optic neuropathies, the main ones being phosphodiesterase type 5 inhibitors, amiodarone, linezolid, ethambutol, and isoniazid. There are few descriptions about the use of selective serotonin 5-HT1 receptor agonists, but some case reports associate NAION and triptans [4]. The cessation of the trigger is one of the most important measures to prevent the progression of vision loss, and in our case, the improvement of the symptoms may be asscoiated with the correct identification of the responsible drug and its discontinuation.
Conclusion
Although triptans have action in the treatment of migraine, their abuse can have serious cardiovascular side effects. We consider that this drug had an additional effect in reducing the perfusion pressure of the ciliary artery circulation, resulting in the visual change described. In this regard, pertinent use and proper guidance is recommended when prescribed such medications.
Competing Interests
We declare no conflict of interest.
Funding
No financial assistance was received in support of the study.
References
2. Katz B, Bamford CR. Migrainous ischemic optic neuropathy. Neurology. 1985 Jan 1; 35(1):112-114.
3. Lee AG, Brazis PW, Miller NR. Posterior ischemic optic neuropathy associated with migraine. Headache: The Journal of Head and Face Pain. 1996 Sep; 36(8):506-10.
4. Chiari M, Manzoni GC, van de Gejin EJ. Ischemic optic neuropathology after sumatriptan in a migraine with aura patient. Headache: The Journal of Head and Face Pain. 1994 Apr;34(4):237-8.