Abstract
Background: Plasma is separated from cellular elements by centrifuge of whole blood, using a heavy spin and frozen the plasma to below –30°C within six hours of collection. Fresh frozen plasma (FFP) has recently gained more importance in clinics. FFP is indicated to control active bleeding in patients with disseminated intravascular coagulation, liver failure and thrombotic thrombocytopenic purpura. FFP contains antibodies capable of causing complications like hemolytic reactions, allergic reactions, alloimmunization, and circulatory overload. For this reason, several guidelines have been published to avoid unnecessary use and to establish a standard, even though improper use of FFP is every day.
Methodology: The objectives of this study were to evaluate “congruous and incongruous” usage of FFP, the effect of FFP transfusion on INR, and define the strategies to reduce misuse. This prospective study was conducted among 1,424 patients who received 3,703 FFP transfusions between January 2021 to December 2021 in MB Hospital, RNT, Udaipur, Rajasthan, India.
Results: 63.9% were females and 36.1% males who received 2,325 (62.8%) and 1,378 (37.2%) FFPs, respectively. A total of 62.8% of patients were transfused 65.9% FFPs appropriately, while 37.2% patients were transfused 34.1% inappropriately. The statistical analysis was performed using Microsoft Excel 2020.
Conclusions: There is a generalized and widespread irrational use of FFP among specialists. This study may help anticipate the dose of FFP required to improve the coagulation variables and set up policies to improve the utility and reduce the wastage of this vital blood product.
Keywords
Blood, FFP, INR, PT, aPTT, TTP
Key Messages
The hospital transfusion guidelines should be established based on existing international guidelines. Awareness programs for clinicians should be conducted regularly. Regular evaluation and audits may help to ensure optimal use of blood and component therapy.
Introduction
Blood is a crucial part of life as there is no other alternative to the human body's connective tissue. Blood is composed of blood cells suspended in plasma. Plasma, which constitutes 55% of body fluid, is mostly water (92% by volume) and contains proteins, glucose, mineral ions, hormones, carbon dioxide, urea, uric acid, oxygen, etc. (plasma being the primary medium for excretory product transportation). Plasma performs many essential functions within the body, like coagulation, supply of nutrients, removal of wastes, transport of hormones and signals, regulation of core body temperature, and hydraulic functions [1].
The use of Fresh Frozen Plasma (FFP) has significantly increased in the past few years, and its usage continues to increase. There are certain situations where FFP is indicated, such as in patients with coagulopathy resulting from disseminated intravascular coagulation (DIC) undergoing invasive procedures or having an active bleed in patients with liver failure with active liver failure bleed and patients for plasma exchange in thrombotic thrombocytopenic purpura (TTP). FFPs are also reserved for conditions requiring therapy in which replacement of multiple plasma constituents is needed or for which the specific constituent is not commercially available in purified injection or transfusion form and for reversal of Warfarin effect when immediate hemostasis is required [2,3].
However, there are many instances, such as specific factor deficiency prophylactic use of FFP, where FFP use is either controversial or not indicated [3,4] (Graphic illustration 1).
Graphic Illustration 1. Uses of FFP.
Criteria for Appropriate Transfusion of FFP as per American Association of Blood Banking (AABB) [4,5]
i. Active bleeding or before surgery or an invasive procedure in patients (adults & neonates) With acquired deficiencies of one or more coagulation factors as demonstrated by an increase Prothrombin Time (PT), Activated Partial Thromboplastin Time (aPTT), International Normalized Ratio (INR) when no alternative therapies are available or appropriate.
ii. Immediate correction of vitamin K deficiency or removal of warfarin effect in a patient with Active bleeding or before surgery or any invasive procedure (In conjunction with use of Prothrombin Complex concentrate).
iii. DIC or consumptive coagulopathy with active bleeding.
iv. TTP.
v. Active bleeding or before surgery or any invasive procedure in patients with congenital factor deficiencies of one or more coagulation factors when no alternative therapies are available or appropriate.
vi. Massive blood transfusion.
vii. Plasma should be transfused adequately i.e., 10-20 ml/kg
viii. Therapeutic Plasma Exchange
ix. Congenital deficiency of “C1 esterase inhibitor”.
Methodology
This prospective study was carried out in Maharana Bhupal Government Hospital, Ravindra Nath Tagore (RNT) Medical College, Udaipur by Department of transfusion medicine from January 2021 to December 2021. This prospective observational study was conducted among 1,424 patients who received 3,703 FFP transfusions between January 2021 to December 2021 in all the clinical departments. Necessary approval of ethical clearance was taken from Institutional Ethics Committee. As it was a double-blinded study, neither the clinicians had prior knowledge of this survey nor any interference from the blood center whenever a request for FFP was made. At the end of each day, patients issued FFP units were identified from the requisition forms received at the blood bank. Information regarding patients and transfusion was collected from the Hospital Computer System, and the requisition forms were sent to the blood bank and from the case-files of the patients at bedside and blood bank records like issue register compatibility register and component register. The demographic details, including name, age, gender, weight, blood group, unique hospital identification number, department of admission, provisional clinical diagnosis and indication for transfusion, number of issues of FFP unit(s), were noted along with pre-and post-transfusion INR.
Abnormal PT and APTT were defined as >1.5-fold that of the control (INR >1.5).
Along with INR, the history of the previous transfusion, presence or absence of bleeding, an invasive or surgical procedure performed or planned, history of anticoagulant therapy, history of other supplements received like vitamin K, prothrombin complex etc. were also noted down.
Although some patients had received FFP transfusions more than once during the study period, only the first transfusion episode was included in the study for each patient. Transfusion episode was defined as each transfusion event when a patient was transfused with FFP.
The quantity or dose of FFP transfused in one transfusion episode was noted down either directly from the medical records of the patients if documented so by the clinician or the following formula calculated it:
Amount of FFP transfused= (a) * (b); where
a= number of FFP units transfused in one transfusion episode obtained from patient's medical record or blood bank issue register
b= quantity of FFP in each unit obtained from the component's records maintained in the department of Transfusion Medicine.
The PT was assayed and INR calculated on a Semi-Automated Coagulation Analyzer. (Stago, Model No. CA50, Sr. No. F6467). The pre-and post-transfusion INRs were calculated to study the effect of FFP on coagulation variables. The post-transfusion PT was calculated within an hour of the completion of the transfusion. Due to the short time gap between measurements of coagulation parameters, the total variation was assumed to be equal to the actual FFP-induced variation with no contribution from the biologic variation. The improvement in the INR per unit of FFP was calculated, and pre-transfusion INR was correlated with the improvement in INR per FFP, using Pearson's linear correlation. The number of patients who showed a significant improvement in the INR was determined using the following formula derived by Holland and Brooks.
Significant Change ≥ 8.9% (pre-transfusion INR)
According to this formula, a decrease of 8.9% or more in a pre-transfusion INR per unit of FFP was considered as a significant improvement.
Results
This study included 1,424 patients who had 3,703 FFPs transfusions during the defined study period between January 2021 and December 2021 in different departments. Among 1,424 patients 910 (63.9%) were females and 514 (36.1%) were male patients who received 2,325 (62.8%) and 1,378 (37.2%) FFPs respectively. In our study, out of a total of 1,424 patients, 740 (52.0%) patients were transfused appropriately; among them, 267 patients received supplements with FFP transfusion, so patients who only received FFP without any supplements were 473 and further studied for the effect of single unit FFP on pre-transfusion INR.
The study of enrolled patients showed that the maximum number of patients (34.6%) were below one year of age while the maximum number of FFPs (31.4%) were transfused to 21-30 years age group patients. Patients of more than 70 years were least in numbers (1%) and had the least number of transfusions (1.4%).
The study result was showed that adult was the maximum in numbers (47.0%), followed by neonates and infants (34.3%), child (11.2%), elderly (4.9%) and then adolescent (2.6%), which is minimum in number. Transfusion of FFPs was maximum in adults (68.7%) and minimum in the adolescent (4.2%) age group.
In current study maximum patients were having blood group B+ (31.9%) followed by O+ (29.4%), then A+ (24.3%) and AB+ (7.5%), Total negative blood group patients were only 2.5% distributed as O (Negative) 2.3%, B Negative 1.0%, A Negative 1.0%, and AB Negative 0.1%.
In the present study majority of patients from general medicine (62.1%) were transfused appropriately by indication, followed by the Pediatrics Department (61.3%), Obstetrics & Gynecology Department (60.4%) and then General Surgery (55.7%), which is the least appropriately transfused by indication. Even though some departments showed a high percentage of appropriateness by indication but the number of patients who received transfusion was meagre in these departments like the Cardiology Department (4 patients/100%), Neurosurgery Department (14 patients/100%), Pediatric Surgery Department (7 patients/100%), Radiotherapy Department (4 patients/80%), CTVS Department (12 patients/80%), Orthopedics Department (19 patients/65.5%). Department wise distribution of FFP requests and transfused FFPs are provided in Tables 1 & 2.
| Department | No. of patients | % | No. of FFPs | % |
|---|---|---|---|---|
| General Medicine | 179 | 12.6 | 815 | 22 |
| Pediatrics | 633 | 44.5 | 741 | 20.0 |
| Radiotherapy | 4 | 0.3 | 22 | 0.6 |
| Cardiology | 3 | 0.2 | 11 | 0.3 |
| General Surgery | 158 | 11.1 | 370 | 10 |
| Neurosurgery | 17 | 1.2 | 63 | 1.7 |
| Orthopedics | 33 | 2.3 | 104 | 2.8 |
| Pediatric Surgery | 8 | 0.5 | 7 | 0.2 |
| Obstetrics &Gynecology | 373 | 26.2 | 1522 | 41.1 |
| CTVS | 16 | 1.1 | 48 | 1.3 |
| Total | 1424 | 100 | 3703 | 100 |
Table 1: Department wise distribution of FFP requests and number of FFPs.
| Departments | No. of Patients | No. of FFPs |
|---|---|---|
| Medical | 797 (56%) | 2018 (54.50%) |
| Surgical | 627 (44%) | 1685 (45.50%) |
| Total | 1424 (100%) | 3703(100%)) |
Table 2: FFP requirements in Medical v/s Surgical departments.
Range of pre-transfusion INR was from 1.6 to 16.8 with standard deviation (SD) 3.8423 [median 2.800 & mean 4.817] while post-transfusion INR were range 0.8 to 11.2 with SD 1.8437 [median 1.900& mean 2.576]. Improvement in the INR per unit of FFP was range 0.0 to 8.0 with SD 1.4507 [median 0.400 & mean 1.004]. A positive linear relationship was found between the pre-transfusion INR and improvement in INR per unit of FFP. The Pearson's correlation coefficient (r) was 0.87 (degree of freedom 490), showing that the net improvement in INR was more with a higher pre-transfusion INR. Using the formula derived by Holland and Brooks, a change of 8.9% or more in the pre-transfusion INR per unit of FFP was considered as a significant change. Out of 473 patients, 349 patients (73.7%) showed a significant improvement in the pre-transfusion INR, and 124 patients (26.3%) showed no significant benefit. We found that with a low pre-transfusion INR, the proportion of patients showing significant improvement in INR was low, while most patients with a higher pre-transfusion INR showed a significant improvement in INR. This statistical analysis is portrayed in Graph 1.
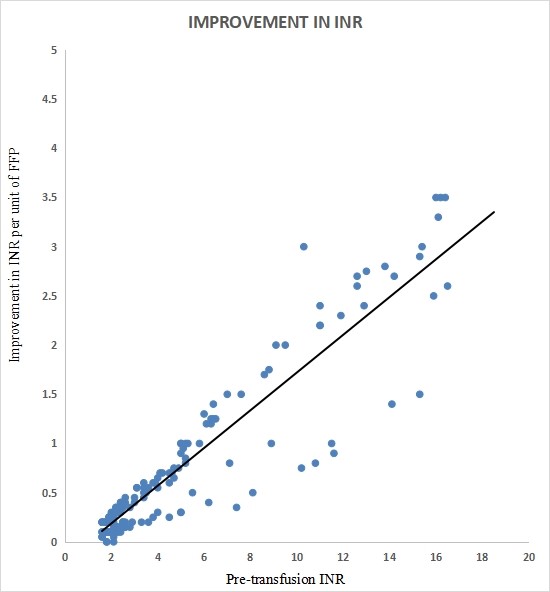
Graph 1. Change in the INR after FFP transfusion.
In our study total of 62.8% of patients were transfused 65.9% FFPs appropriately, while 37.2% of patients were transfused 34.1% FFPs inappropriately. Details are provided in Tables 3 and 4.
| Indication | No. of patients | % |
|---|---|---|
| A- DIC with bleeding | 118 | 8.8 |
| B- Raised INR with bleeding/ hemorrhage | 448 | 33.5 |
| C- Raised INR before or during surgery | 225 | 16.8 |
| D- Massive transfusion | 23 | 1.7 |
| E- Removal of Warfarrin effect | 11 | 0.8 |
| G- During hemorrhage with normal INR | 136 | 10.2 |
| H- Raised INR without bleeding/ hemorrhage | 103 | 7.8 |
| I- During surgery without any raise in INR | 47 | 3.5 |
| J- Volume replacement | 35 | 2.6 |
| K- Hypoproteinemia | 4 | 0.3 |
| L- Massive transfusion: where ratio of RCC to FFP is not corrected | 11 | 0.8 |
| M- Nutritional support | 4 | 0.3 |
| N- Other - inappropriate | 172 | 12.9 |
Table 3: Indication v/s number of patients.
| Indication | FFPs | % |
|---|---|---|
| Appropriate | 2440 | 65.9 |
| Inappropriate | 1263 | 34.1 |
| Total | 3703 | 100 |
Table 4: Indication v/s Number of FFPs.
Total 82.4% of patients were transfused appropriately by dose, and 17.6% were transfused inappropriately. Appropriate by dose in different departments showed a range of appropriateness as Pediatrics Department showed 97.6% appropriateness by dose while Obstetrics & Gynecology Department Showed 80.6%, General Medicine Department showed 74.4% and Orthopedics Department showed 65.5% appropriateness by dose. The general surgery department showed only 42.1% appropriateness. Department with less number of FFP requisitions also showed a wide range inappropriateness by dose such as Pediatric Surgery Department 85.7%, Radiotherapy Department 80.0%, Neurosurgery Department 71.4%, CTVS 60.0%, Cardiology Department 50.0%.
Overall appropriateness of FFP transfusion was considered if transfusion was appropriate by indication and dose. In our study, a total of 53.0% of patients were overall appropriately transfused while 47.0% were inappropriately transfused. Pediatrics department patients were transfused appropriately in the highest percentage compared to others. They were transfused 59.8% appropriately followed by Obstetrics & Gynecology department 51.9% followed by General Medicine department 49.0% followed by Orthopedics department 41.4% then least appropriately transfusion had done by General Surgery department that is only 32.1%. Department with few numbers of FFP requisition showed a different type of appropriateness pattern among them Pediatric Surgery and Neurosurgery department patients were transfused most appropriately 85.7% and 71.4% respectively and department of Radiotherapy, CTVS and Cardiology patients were transfused 60.0%, 53.3% and 50.0% respectively.
In the current study, we analyzed that 64.6% FFPs were transfused by indication for 61.7% of patients and 86.5% FFPs transfused appropriately by dose for 82.4% of patients.
Overall, 58.0% FFPs were transfused appropriately for 53% patients while 42% FFPs were transfused inappropriately for 47% patients. The current study found that 56% of medical and 44% of surgical patients were transfused appropriately with 54.50% and 45.50% FFPs, respectively.
Discussion
FFP, which came into use in the 1940s, has gained more importance in the clinic, and significant rises are reported in US [5]. For this reason, several guidelines have been published to avoid unnecessary use and to establish a standard while clinicians are deciding on the use of FFP. However, the literature still reports that improper use of FFP every day despite these guidelines. However, sufficient data are unavailable concerning the use of FFP transfusion, especially in Emergency Departments where transfusion practices are numerous in India. This study aimed to analyze the use of FFP and evaluate the audit of the transfusion. FFP usage was called Appropriate if appropriate by indication according to AABB guidelines & appropriate by dosage [6,7]. Appropriateness of FFP usage by indication is based on the guidelines published by AABB. These include active bleeding or before surgery or an invasive procedure in patients (adults & neonates with acquired deficiencies of one or more coagulation factors as demonstrated by an increased PT, APTT, or INR), immediate correction of vitamin K deficiency or removal of Warfarin effect in a patient with active bleeding or before surgery or any invasive procedure (In conjunction with the use of Prothrombin Complex concentrate). The other examples of appropriate uses are DIC or consumptive coagulopathy with active bleeding, TTP, active bleeding or before surgery or any invasive procedure in patients with congenital factor deficiencies of one or more coagulation factors when no alternative therapies are available or appropriate, massive blood transfusion, therapeutic Plasma Exchange, and congenital deficiency of "C1 esterase inhibitor .
AABB also defines appropriateness of FFP usage by dose, which states infusion of 10-15 ml/kg body weight of the patient as an optimum dose of FFP.
The FFP transfusion episodes are divided as appropriate if both the indication for transfusion and dose transfused were appropriate and inappropriate if the indication and or dose were inappropriate.
Typical examples for inappropriate transfusion of FFP are for volume replacement, correction of hypoalbuminemia, nutritional support, immunoglobulin replacement, raised INR without bleeding, FFP transfused without any raise in INR (during surgery), during hemorrhage with normal INR, prophylactically without bleeding, in massive transfusion ratio of RCC to FFP not correct, request forms of patients with INR<1.5, and plasma transfused in inadequate volume (<10ml/kg) at least 10ml/kg body weight of plasma should be transfused) [2].
Study Limitations
This study has a few crucial limitations, like we could not assess the actual effectiveness of FFP transfusions due to inadequate data and insufficient documentation. The result of the study cannot be generalized to the population due to differences in indications needed in different hospitals and differences in knowledge and practices in the clinicians. Finally, this was a single-center study; multicenter studies are needed to investigate these issues on a broader scale and analyze the potential roles of setting level factors such as academic competitiveness and availability of health services.
Conclusion
In this study, the above-mentioned guidelines were used as the reference standard, and overall appropriateness of FFP transfusion was considered if transfusion were appropriate by indication and dose both. In our study total of 53.0% of patients were overall appropriately transfused while 47.0% were inappropriately transfused in terms of indication and amount transfused. These included inadequately documented transfusion episodes and documented inappropriate indications and/or doses. The most common appropriate indication for FFP usage was raised INR with bleeding/ hemorrhage followed by raised INR before or during surgery followed by DIC with bleeding. The Pearson's correlation coefficient (r) was 0.87, signifying a positive linear correlation that the net improvement in INR was more with higher pre-transfusion INR.
References
2. Kulkarni N. Evaluation of fresh frozen plasma usage at a medical college hospital-A two-year study. International Journal of Blood Transfusion and Immunohematology (IJBTI). 2012 Jan 1(2):16-20.
3. Sameer MA, Dagar V, Deshpande SA. Appropriate and Inappropriate Use of Fresh Frozen Plasma (FFP) and Packed Cell Volume (PCV). International Journal of Health Sciences and Research. 2014;4(9):37-42.
4. Jayanthi N, Pitchai R. Audit of fresh frozen plasma usage and study the effect of fresh frozen plasma on the pre transfusion and post-Transfusion international normalized ratio. International Journal of Current Medical And Applied Sciences. 2015;7:34-9.
5. Richa S, Chetna J. An audit of appropriate use of blood components in tertiary care hospital. Int J Med Sci Educ. 2015;2(3).
6. Lingegowda JB, Jeyakumar JD, Muddegowda PH, Pitchai R, Gopal N, Sinha P. An audit of requests for fresh frozen plasma in a tertiary care center in South India. Journal of Laboratory Physicians. 2016 Jan;8(01):041-4.
7. Bhagwat SN, Sharma JH. A retrospective audit of appropriateness and monitoring of fresh frozen plasma transfusions in a tertiary care hospital. International Journal of Contemporary Medical Research. 2017;4:1562-7.
