Abstract
Introduction: Cancer has its own disease burden and patients usually suffer from symptom clusters when they are referred for palliative treatment. Identification of symptom cluster trajectories will help clinician to take into account measures that can optimize quality of life of palliative patients. Therefore the aim of this paper is to determine the overall prevalence of symptoms and symptoms clusters in different disease groups according to etiology at the time of first visit to Palliative care clinic by using HIS Palliative First Assessment note indicating Edmonton symptom scale.
Method: It’s a cross sectional study conducted in a tertiary care cancer hospital. Statistical analysis was carried out using the SPSS software (version 20.0; SPSS, Chicago, IL, USA). Continuous variables were stated as mean ± standard deviation and categorical variables were expressed as frequencies and percentages. Agglomerative hierarchical cluster analysis was used to create the symptom clusters.
Results: The most prevalent symptoms were pain (91.8%), Anxiety (88.5%), depression (87.4%), tiredness (84.1%), lack of appetite (74.7%), nausea (57.1%), drowsiness (50.5%) and shortness of breath (46.2%). Two symptom clusters were defined as a result of cluster analysis; depression, anxiety, pain, tiredness, lack of appetite and nausea, drowsiness and shortness of breath.
Conclusion: Symptom cluster study is a beneficial tool to improve overall patient’s health. By treating these symptom clusters, morbidity of palliative patients can be significantly decreased.
Keywords
Palliative care, Quality of Life assessment, Prevalence, Edmonton symptom assessment scale, Symptom clusters, Malignancies, Morbidity.
Introduction
Advanced cancer has a high disease burden and patients usually suffer from multiple symptoms impacting their quality of life. Cancer patients seldom present with a single symptom [1]. Symptoms may be a result of the disease itself or of the antineoplastic treatment. They can significantly limit a patient’s physical and social activities. Dodd et al., [2] were among the first researchers to use the term symptom clusters in their article on pain, fatigue, and sleep disturbances; and together with others they found that the occurrence of multiple symptoms independently predicts alteration in patients’ clinical condition, treatment outcomes and quality of life.
Symptoms cluster may be defined as two or more concurrent symptoms [3] which are systemic in nature [4], relatively independent of other clusters [5] and seldom occur in isolation [6]. These comorbid symptoms are directly associated with progression of the disease [6] which can shatter the quality of life, functional status, mood state [7], and can increase patients’ hyper vigilance towards further suffering [8]. In a qualitative study Dong et al. [8] reported that patients described these clusters as a roller coaster, due to their volatile interaction and fluctuation in nature. Traditionally isolated symptom management has been the focus of attention amongst health care providers [9]. However identification of symptoms cluster will efficiently assist us to understand the dynamic nature of symptom progression [10] and provide an avenue to target therapeutic interventions [2]. Understanding patient’s experience of symptoms cluster will facilitate effective symptoms management [11] thus drastically reducing patient’s distress.
Barallat et al. [12] described that patient’s experience of advanced disease is complex and multifaceted which impairs every aspect of an individual’s functioning. It is clear that cancer patients usually suffer from both physical and psychological issues. Health care professionals can have a tendency to focus mainly on treating physical symptoms, leaving psychological issues which may be equally distressing unaddressed. Most researches conducted on symptoms clusters have found that physical symptoms are statistically more prevalent among patients known to palliative care services. According to Kang et al. [10], in a large scale study conducted on change in symptoms intensity, physical symptoms like pain, fatigue and shortness of breath were found more frequently whereas depression came down in the list. Likewise, in a qualitative study, patients described their physical symptom as being restrained in a ‘vicious cycle’ of fatigue and weakness [8]. What people forget to understand is that, there is deep unseen anguish and torment caused by the psychological distress and anxiety among the patients living the few days of unpredictable life. The fact is psychological distress is the main reason behind those physical symptoms [13]. To be able to better care for these patients, we need to listen to the melody of their psychological pain and distress.
The main objective of this study is to identify cluster symptom trajectories that will help clinician to take into account measures that can optimize quality of life of patients in a more dignified way and lead to peaceful management of their chronic illness as per their disease group. To achieve optimal level of care for patient with advanced cancer, there is a need of evidence based research to identify the group of diseases with most prevalent clusters, so that we can extend their meaningful survival, improve the quality of life and mend their suffering. Our study is the extension of other significant studies done previously on symptoms cluster in order to provide better care for the patient undergoing palliative therapy. This is the first study in our population thus making it unique that it will first focus on the most prevalent symptoms in all selected population and then the common symptoms in cluster form in different disease groups.
Materials and Methods
This is a cross sectional study design done in Pakistan on patients undergoing palliative treatment in a tertiary care cancer hospital.
I) Symptoms assessment and data collection
All patients who came to palliative medicine clinic in our center from June 2017 to Aug 2017 were enrolled in the study. As part of their initial assessment by the medical and nursing team, the Edmonton Symptoms Assessments Scale (ESAS), which is a very concise scale containing 8 symptoms that includes anxiety, depression, pain, drowsiness, tiredness, nausea lack of appetite and shortness of breath was completed for each patient. We preferred ESAS due to its simplicity and ease to use with minimal training. Research has shown that long and lengthy tools have less clinical utility especially in patients with advanced life limiting disease [14]. Symptoms were subjectively described by the patients according to their severity on a scale of 0-10, where 0 represents absence of symptoms and 10 indicates maximum severity index. We also recorded demographic variables such as age, gender, education level, marital status, social status, and disease.
II) Inclusion and exclusion criteria
All patients who were seen for the first time in the palliative medicine clinic during the study period were included. Any patients unwell enough to not be able to communicate actively were excluded.
III) Statistical analysis
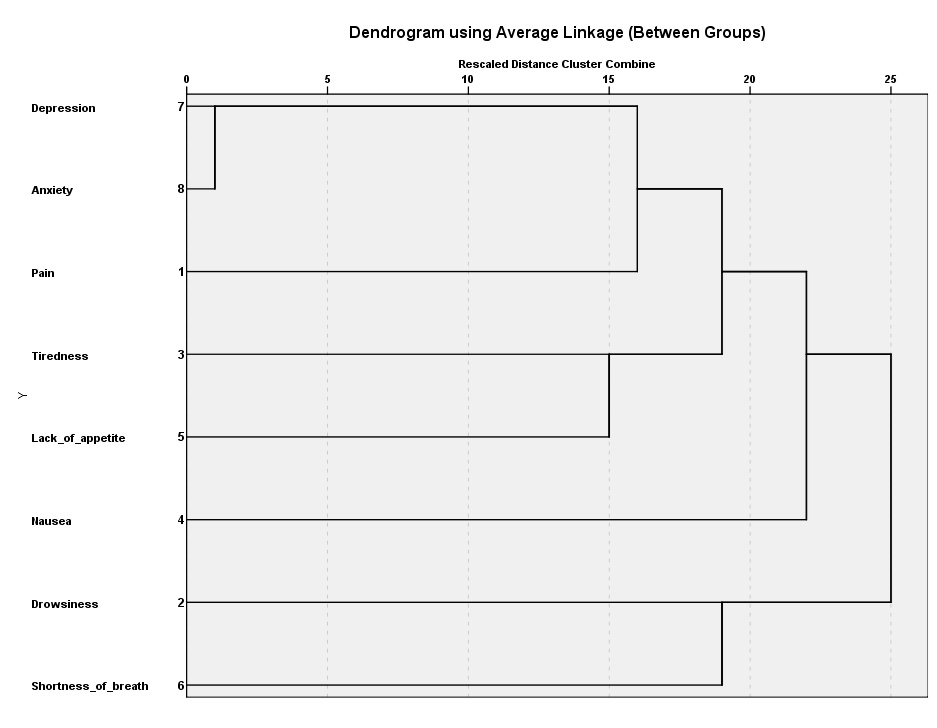
Statistical analysis was carried out using the SPSS software (version 20.0; SPSS, Chicago, IL, USA). Continuous variables were stated as mean ± standard deviation and categorical variables were expressed as frequencies and percentages. Symptoms prevalence was calculated by using the simple prevalence formula. Agglomerative hierarchical cluster analysis was used to create the symptom clusters. The symptoms with <40% prevalence were omitted from the cluster analysis. The distance between the clusters was calculated with euclidean distance. The created clusters were shown by dendrogram as shown in Figure 1.
Figure 1. Dendrogram analysis of symptoms cluster.
IV) Ethical consideration
Waiver of Informed consent is considered since data was collected retrospectively from Hospital information system (HIS) and it does not need direct patient contact. The data from this study was analyzed on SPSS and recoding was done for Medical record (MR) numbers to keep confidentiality.
Results
Table 1 presents the baseline description of 182 patients with a mean age and standard deviation of 48.91 ± 16.47 years. The majority of the patients were female (52.2%) with around (85.7%) were married. Additionally, most of the patients presented to palliative services with metastatic disease (69.8%) and majority of the patients were known about their disease status (89.6%). Furthermore, the prevalent diagnose was GI (28.6%), breast (15.9%) and head and neck (19.8%) respectively. Details of patient’s demographic characteristics and disease distributions are given in Table 1 and 2 respectively.
| Variables | Categories | N (%) |
|---|---|---|
| Age in years | mean ± SD* | |
| Sex | Female | 95 (52.2%) |
| Male | 87 (47.8%) | |
| Marital status | Single | 22 (12.1%) |
| Married | 156 (85.7%) | |
| Divorced | 4 (2.2%) | |
| Education status | No education | 63 (34.4%) |
| Literate | 45 (24.7%) | |
| School | 44 (24.2%) | |
| College or above | 30 (16.5%) | |
| Income of household | Up to 20k | 96 (52.7%) |
| Above 20k | 86 (47.3%) | |
| Metastasis status | No | 55 (30.2%) |
| Yes | 127 (69.8%) | |
| Disease known to patient | No | 19 (10.4%) |
| Yes | 163 (89.6%) | |
| Dependents | None | 43 (23.6%) |
| 01-Feb | 45 (24.7%) | |
| 03-Apr | 94 (51.6%) | |
| Referral to dietician | Low Risk | 100 (54.9%) |
| Medium Risk | 63 (34.6%) | |
| High Risk | 19 (10.4%) | |
| Mental score | mean ± SD* | 4.49 ± 2.91 |
| *standard deviation | ||
| Disease origin | Frequency |
|---|---|
| Head and neck | 36 (19.8) |
| Gastroesophageal | 52 (28.6%) |
| Breast cancer | 29 (15.9%) |
| Urology | 23 (12.6%) |
| Solid Tumor | 25 (13.7%) |
| Others | 11 (6.0%) |
| Hematological malignancies | 6 (3.3%) |
I) Symptoms prevalence and severity on admission
The most prevalent symptoms were pain (91.8%), anxiety (88.5%), depression (87.4%), tiredness (84.1%), lack of appetite (74.7%), nausea (57.1%), drowsiness (50.5%) and shortness of breath (46.2%). Furthermore, symptoms were sub divided in to most prevalent diagnosis; Gastro- Intestinal (GI), head and neck and breast as shown in Tables 4-6 respectively. Two symptom clusters were defined as a result of cluster analysis; depression, anxiety, pain, tiredness, lack of appetite and nausea, drowsiness and shortness of breath.
| Variable of Symptom (Range of Severity) | With Symptom | Sex | ||
|---|---|---|---|---|
| N | Prevalence (%) | Male | Female | |
| Pain | 167 | 91.8 | 79 | 88 |
| Anxiety | 161 | 88.5 | 72 | 89 |
| Depression | 159 | 87.4 | 72 | 87 |
| Tiredness | 153 | 84.1 | 71 | 82 |
| Lack of appetite | 136 | 74.7 | 65 | 71 |
| Nausea | 104 | 57.1 | 44 | 60 |
| Drowsiness | 92 | 50.5 | 39 | 53 |
| Shortness of breath | 84 | 46.2 | 29 | 55 |
| Variable of Symptom (Range of Severity) | With Symptom | Sex | ||
|---|---|---|---|---|
| N | Prevalence (%) | Male | Female | |
| Pain | 35 | 97.2 | 22 | 13 |
| Tiredness | 34 | 94.4 | 20 | 14 |
| Anxiety | 32 | 88.9 | 19 | 13 |
| Depression | 32 | 88.9 | 19 | 13 |
| Lack of appetite | 26 | 72.2 | 14 | 12 |
| Drowsiness | 16 | 44.4 | 7 | 9 |
| Shortness of breath | 14 | 38.9 | 5 | 9 |
| Nausea | 12 | 33.3 | 7 | 5 |
| Variable of Symptom (Range of Severity) | With Symptom | Sex | ||
|---|---|---|---|---|
| N | Prevalence (%) | Male | Female | |
| Pain | 47 | 90.4 | 27 | 20 |
| Anxiety | 45 | 86.5 | 25 | 20 |
| Depression | 45 | 86.5 | 25 | 20 |
| Tiredness | 45 | 86.5 | 29 | 16 |
| Lack of appetite | 42 | 80.8 | 27 | 15 |
| Nausea | 37 | 71.2 | 22 | 15 |
| Shortness of breath | 24 | 46.2 | 14 | 10 |
| Drowsiness | 23 | 44.2 | 15 | 8 |
| Variable of Symptom (Range of Severity) | With Symptom | Sex | ||
|---|---|---|---|---|
| N | Prevalence (%) | Male | Female | |
| Pain | 27 | 93.1 | 0 | 27 |
| Anxiety | 26 | 89.7 | 0 | 26 |
| Tiredness | 26 | 89.7 | 0 | 26 |
| Depression | 24 | 82.8 | 0 | 24 |
| Lack of appetite | 22 | 75.9 | 0 | 22 |
| Drowsiness | 19 | 65.5 | 0 | 19 |
| Shortness of breath | 19 | 65.5 | 0 | 19 |
| Nausea | 19 | 65.5 | 0 | 19 |
Discussion
The most prevalent symptom identified in our study was pain 91.8% making it an important factor which can trigger other symptoms. Previous studies have identified that pain is a very significant symptom known to any palliative care service. Chwistek [15] stated that there is complex neurophysiological mechanism behind pain which makes it a substantial concern in palliative setting. Cancer patients with pain can present with numerous cognitive, emotional and psychosocial symptoms [16]. Therefore, effective pain assessments and management are important aspects of palliative care services and can significantly impact the quality of life of a patient. Practitioners need to address myths related to opioid dependency and make opioids available for pain management [17,18].
The prevalence of psychological symptoms like anxiety and depression accounts for 88.5% and 87.4% respectively. The same findings were noticed in a retrospective study and it was identified that 79 (37%) palliative patients had depression and 94 (44%) had anxiety [13]. In the same study, a comparison was done among patients with high level of anxiety/depression with those without it and it was found that these patients had intensified levels of nausea, drowsiness, pain and poor appetite. Studies from Delgado et al. [13], Shad et al. [18] and Lancker et al. [19] have also shown that there could be bidirectional relation between psychological symptoms and sensitivity towards the perception of physical symptoms. This makes it clear that higher level of psychological issues can trigger physical symptoms and vice versa. The underlying cause could be due to biological factors and physiological response of body towards cancer and its treatment, but regardless of the cause, palliative patients need holistic approach towards symptom management. A meta-analysis of 94 interview based studies on prevalence of depression, anxiety, and adjustment disorder in oncological, hematological, palliative care patients showed that the prevalence of depression was significantly high among cancer patients as compared to non-cancer patients [20]. Moreover, the same meta-analysis estimated that advancement in cancer treatment and increase survival rates have dramatically increased the prevalence of many psychological issues among cancer patients (calculating 340,000 people in the UK and 2 million in the USA with major depression and cancer at any time). The situation is not different in our part of the world but due to the lack of awareness and stigmatization of psychological issues, these problems are usually either ignored or considered taboo to discuss [21]. In addition to this, psycho oncology is still its infancy and there are only few hospitals in our country where comprehensive phycology services are integrated in palliative care [21].
Our study results also identified that the prevalence of lack of appetite was 74.7%, nausea 57.1%, and drowsiness 50.5%. Substantial correlation always exists between tiredness and lack of appetite. Persistent loss of appetite and poor oral intake over an extended period of time is a major predictor for tiredness among palliative patients. These findings were also identified in a study on symptoms clusters among palliative patients and their impact on quality of life. It was found that the prevalence of fatigue, taste changes and lack of appetite was more than 70% [11]. A multicenter observational study conducted in Japan reported that the majority of patients referred to palliative service were suffering from moderate to severe cancer related fatigue, suggesting that it as a potentially problematic as pain [16]. The highest mean severity score for tiredness and loss of appetite was also seen in a study on non-pain symptoms among palliative care patients [22]. The primary site of cancer in most of the patients in our study group was colorectal and gastro-esophageal which could be the reason behind the intensity of GI related symptoms but there could be other contributing factors. A longitudinal study of consecutive cohort for (n=7772) palliative patients seen over a time period of 6.3 years also confirmed strong association between nausea, altered bowel habit and loss of appetite among palliative care patients [23]. These symptoms were more apparent in GI related malignancies. Excessive use opioids to manage debilitating pain, multi organ dysfunction [24] and systematic inflammatory response [25] to counter cancer and its treatment are major causes behind these symptoms among palliative patients. Thus it is strongly recommended that palliative care provider should have adequate knowledge of the pathophysiological mechanism behind gastrointestinal symptoms in order to better evaluate the cause and plan treatment strategies accordingly [26].
We also sought to identify the prevalence of various symptoms in different disease group. Understanding inter-group symptoms variation would assist the clinician to predict potential symptoms in the specific disease group. Three major disease groups were identified in our study which includes gastrointestinal cancers 52 (28.6%), head and neck tumors 36 (19.8%) and breast cancers 29 (15.9%). The prevalence of symptoms varied according to different disease groups. It was found that in all three disease groups; pain remained the most common cause of suffering among patients seeking palliative care. Our analysis also indicated that a physical symptom like tiredness was more common among patients with head and neck cancer as compared to the other disease groups. In contrast, the burden of psychological symptoms like anxiety and depression was relatively high among patients with gastrointestinal and breast cancer. The prevalence of shortness of breath was relatively low in all three disease groups.
The other important component that we analyzed in our study was prevalence of symptom clusters. Two symptom clusters were defined as a result of cluster analysis. These clusters are presented by dendrogram as shown in Figure 1. First cluster: depression, anxiety, pain, tiredness, lack of appetite; Second cluster: nausea, drowsiness and shortness of breath.
Our analysis shows strong association between depression and anxiety which was also identified in quite few studies done on symptom clusters [11,14]. The strong association of psychological symptoms with the prevalence of pain and loss of appetite is a major significant finding that came out in our study. This could be due to the fact that pain perception is increased when an individual is mentally distressed or vice versa. In previous researches, inflammatory and neuro immune markers were found to be associated with pain, depression and fatigue cluster but further investigation is warranted [21,22,27]. Considering these findings, it is recommended that patients should be encouraged to have an understanding of interaction among these symptoms [28]. This can only be done if the practitioners are also aware of the association between different symptom clusters [8].
In the second cluster, shortness of breath came in close association with drowsiness and nausea. This was a very unique manifestation in our study but the close association between these three symptoms was difficult to rationalize. Disease origin, biological factors and metastasis could be the reason behind co-occurrence of these symptoms but further study to rationalize contributing factor is recommended [29].
We have seen that patients regardless of their malignancies may have common overlapping symptoms in the form of clusters. It is imperative that these clusters be identified early on in their assessment so that appropriate multidisciplinary management can be initiated. This will not only reduce the morbidity associated with advanced disease but will also help in improving the patient’s quality of life at this fragile time in their disease trajectory. In light of our findings, we have initiated multi-disciplinary team meetings on a weekly basis where all new cases referred to the service are discussed in the presence of physicians, nurses, psychologists, nutritionist pharmacists and physiotherapists to formulate comprehensive multidisciplinary individualized management plans for all patients.
Identifying and managing symptoms clusters can improve a patient’s health in the palliative setting [29]. Even though the disease has advanced, palliative care can enhance the quality of life for such patients during the terminal stages of their illness [30]. It is noted that by identifying the relationship among the symptom clusters, better symptom control leading to enhancement in the general wellbeing of a patient can be achieved. By identifying symptom clusters, palliative care multi-disciplinary teams can improve patient’s care and well-being by treating these clusters as per disease group in a more appropriate way [7,30-32].
Limitations of this study
Limitations of this study include sampling from a single center only.
Conflicts of Interest
The authors declare no conflict of interest.
References
2. Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. In: Oncology nursing forum 2001 Apr 1 (Vol. 28, No. 3).
3. Aktas A, Walsh D, Rybicki L. Symptom clusters: myth or reality?. Palliative Medicine. 2010 Jun;24(4):373-85.
4. Lacasse C, Beck SL. Clinical assessment of symptom clusters. In: Seminars in oncology nursing 2007 May 1 (Vol. 23, No. 2, pp. 106-112). WB Saunders.
5. Miaskowski C, Aouizerat BE. Is there a biological basis for the clustering of symptoms?. In: Seminars in oncology nursing 2007 May 1 (Vol. 23, No. 2, pp. 99-105). WB Saunders.
6. Omran S, Khader Y, McMillan S. Symptom clusters and quality of life in hospice patients with cancer. Asian Pacific journal of cancer prevention: APJCP. 2017;18 (9):2387.
7. Fan G, Hadi S, Chow E. Symptom clusters in patients with advanced-stage cancer referred for palliative radiation therapy in an outpatient setting. Supportive cancer therapy. 2007 May 1;4(3):157-62.
8. Dong ST, Butow PN, Agar M, Lovell MR, Boyle F, Stockler M, Forster BC, Tong A. Clinicians' Perspectives on Managing Symptom Clusters in Advanced Cancer: A Semistructured Interview Study. Journal of pain and symptom management. 2016 Apr 1;51(4):706-17.
9. Jiménez A, Madero R, Alonso A, Martínez-Marín V, Vilches Y, Martínez B, Feliu M, Díaz L, Espinosa E, Feliu J. Symptom clusters in advanced cancer. Journal of pain and symptom management. 2011 Jul 1;42(1):24-31.
10. Kang JH, Kwon JH, Hui D, Yennurajalingam S, Bruera E. Changes in symptom intensity among cancer patients receiving outpatient palliative care. Journal of pain and symptom management. 2013 Nov 1;46(5):652-60.
11. Rha SY, Lee J. Symptom clusters during palliative chemotherapy and their influence on functioning and quality of life. Supportive Care in Cancer. 2017 May 1;25 (5):1519-27.
12. Barallat E, Nabal M, Canal J, Trujillano J, Gea-Sánchez M, Larkin PJ, Downing MG. The Spanish adaptation of the palliative performance scale (version 2) among Cancer patients at the end of life: psychometric properties. Journal of pain and symptom management. 2017 Oct 1;54(4):570- 7.
13. Delgado-Guay M, Parsons HA, Li Z, Palmer JL, Bruera E. Symptom distress in advanced cancer patients with anxiety and depression in the palliative care setting. Supportive Care in Cancer. 2009 May 1;17 (5):573-9.
14. Kirkova J, Aktas A, Walsh D, Rybicki L, Davis MP. Consistency of symptom clusters in advanced cancer. American Journal of Hospice and Palliative Medicine®. 2010 Aug;27(5):342 -6.
15. Chwistek M. Recent advances in understanding and managing cancer pain. F1000Research. 2017;6.
16. Iwase S, Kawaguchi T, Tokoro A, Yamada K, Kanai Y, Matsuda Y, Kashiwaya Y, Okuma K, Inada S, Ariyoshi K, Miyaji T. Assessment of cancer-related fatigue, pain, and quality of life in cancer patients at palliative care team referral: a multicenter observational study (JORTC PAL-09). PloS one. 2015 Aug 5;10(8):e0134022.
17. Doherty M, Khan F, Biswas FN, Khanom M, Rahman R, Tanvir MM, Akter F, Sarker M, Ahmad N. Symptom prevalence in patients with advanced, incurable illness in Bangladesh. Indian journal of palliative care. 2017 Oct;23(4):413.
18. Shad A, Ashraf MS, Hafeez H. Development of palliative-care services in a developing country: Pakistan. Journal of pediatric hematology/oncology. 2011 Apr 1;33:S62-3.
19. Van Lancker A, Beeckman D, Verhaeghe S, Van Den Noortgate N, Van Hecke A. Symptom clustering in hospitalised older palliative cancer patients: A cross-sectional study. International journal of nursing studies. 2016 Sep 1;61:72-81.
20. Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview- based studies. The lancet oncology. 2011 Feb 1;12(2):160-74.
21. Jovindah S, Sheikh HS. PSYCHO-ONCOLOGY: RATIONALE AND ITS PAKISTANI PERSPECTIVE. Journal of Cancer & Allied Specialties.;3(3).
22. Al-Shahri MZ, Eldali AM, Al-Zahrani O. Nonpain symptoms of new and follow-up cancer patients attending a palliative care outpatient clinic in Saudi Arabia. Indian journal of palliative care. 2012 May;18 (2):98.
23. Clark K, Smith JM, Currow DC. The prevalence of bowel problems reported in a palliative care population. Journal of pain and symptom management. 2012 Jun 1;43(6):993 -1000.
24. Özalp GŞ, Uysal N, Oğuz G, Koçak N, Karaca Ş, Kadıoğulları N. Identification of symptom clusters in cancer patients at palliative care clinic. Asia-Pacific journal of oncology nursing. 2017 Jul;4(3):259.
25. Kelly DL, Dickinson K, Hsiao CP, Lukkahatai N, Gonzalez-Marrero V, McCabe M, Saligan LN. Biological basis for the clustering of symptoms. In: Seminars in oncology nursing 2016 Nov 1 (Vol. 32, No. 4, pp. 351-360). WB Saunders.
26. Cherwin CH. Gastrointestinal symptom representation in cancer symptom clusters: a synthesis of the literature. InOncology nursing forum 2012 Mar (Vol. 39, No. 2, p. 157). NIH Public Access.
27. Kwekkeboom KL, Tostrud L, Costanzo E, Coe CL, Serlin RC, Ward SE, Zhang Y. The role of inflammation in the pain, fatigue, and sleep disturbance symptom cluster in advanced Cancer. Journal of pain and symptom management. 2018 May 1;55(5):1286-95.
28. Kwekkeboom KL. Cancer symptom cluster management. In: Seminars in oncology nursing 2016 Nov 1 (Vol. 32, No. 4, pp. 373-382). WB Saunders.
29. Xiao C. The state of science in the study of cancer symptom clusters. European Journal of Oncology Nursing. 2010 Dec 1;14 (5):417-34.
30. Esper P. Symptom clusters in individuals living with advanced cancer. InSeminars in oncology nursing 2010 Aug 1 (Vol. 26, No. 3, pp. 168-174). WB Saunders.
31. Hwang KH, Cho OH, Yoo YS. Symptom clusters of ovarian cancer patients undergoing chemotherapy, and their emotional status and quality of life. European Journal of Oncology Nursing. 2016 Apr 1;21:215- 22.
32. Gough N, Koffman J, Ross JR, Riley J, Judson I. Symptom burden in advanced soft- tissue sarcoma. Journal of pain and symptom management. 2017 Mar 1;53(3):588-97.