Abstract
Background and study aim: Total elbow arthroplasty (TEA) has gained popularity in recent years, with most surgeons favoring cemented elbow prostheses. The objective of this study was to evaluate the outcome of our series and if specific radiological cementation criteria may predict clinical outcome.
Material and methods: All patients submitted to cemented TEA were retrospectively reviewed over a 10-year period in an institution. All radiographs performed in the immediate postoperative period were blindly evaluated and classified according to specific cementation criteria. The radiographs of the last medical appointment were also blindly evaluated for possible signs of loosening, with a minimum followup of 4 years. The complication rate, revision rate, average prosthesis survival and QuickDASH Score were also evaluated. Statistical analysis was then performed to evaluate whether cementation quality had an influence on clinical and radiological results.
Results: A total of 31 TEA were identified. Patients with an inadequate or marginal ulnar cementation were 9.2 times more likely of having a cubital loosening (p=0.032; OR=9.2[95% CI 1-91]). However, inadequate or marginal humeral cementation did not have a statistically significant association with the presence of humeral loosening (p=0.27). In our sample, there were 4 cases of aseptic loosening requiring revision. In all of them there were marginal or inadequate cementations in one of the components.
Conclusions: This work highlighted the importance of adequate cementation and radiological evaluation. From this study, we can conclude that poor ulnar cementation may predict radiological loosening and eventual need for revision. However, this loosening does not correlate with the patient’s clinical outcomes or the need for revision.
Keywords
Total elbow arthroplasty, Cementation criteria, Aseptic loosening, Quick DASH Score
Introduction
Total elbow arthroplasty (TEA) has gained popularity in recent years and the indications for performing this surgery have been expanding. Initially this arthroplasty was used predominantly in patients with severe rheumatoid arthritis of the elbow, however, nowadays, TEA has been performed also in other situations like osteoarthritis, comminuted intra-articular fractures or tumors [1].
Since the initial introduction by Park and Moreau in 1870, total elbow arthroplasty has evolved through the constrained design type, which requires extensive soft tissue resection, and unconstrained type, which has high dislocation rates [2-4]. Currently, semi-constrained TEA is the most widely used design.
Since the first TEA system using cement fixation was introduced in 1972 by Dee [3] numerous designs have become available and surgical techniques have been improved [5-7]. There are uncemented and cemented options, with most surgeons favoring nowadays cemented elbow prostheses [8-10].
Although the complication rate of TEA is higher than that of other joint arthroplasties [10-12], it is certain that the rate has decreased over the years with new and improved TEA designs and careful postoperative care [8].
Aseptic loosening is one of the most common causes of failure of the prosthesis in the long term [8,10,13,14]. Inadequate cementing has been recognized by some papers to contribute to this complication [10,15,16], however the current literature only offers sparse content on this matter.
So, the aim of this study was to analyze the results of our center in this type of arthroplasty and also most importantly to evaluate if specific cementation radiological criteria may predict clinical outcome and revision rate.
Material and Methods
This study was approved by the local ethics committee and was conducted in compliance with the standards of the Declaration of Helsinki.
It is a retrospective study of all the patients submitted to TEA by the same surgical team (2 experienced elbow surgeons) over a 10-year period (January of 2006 to January of 2016) in an institution.
All patients were characterized in terms of age, gender, comorbidities and diagnosis that led to the arthroplasty. All TEA were cemented.
Radiographs performed in the immediate postoperative period were collected and randomized. Then they were blindly evaluated always by the same experienced surgeon and classified according to Schneeberger cementation criteria [17] (adequate, marginal and inadequate). The degree of cementation was defined as adequate (Figure 1) when the cement extended beyond the tip of the prosthesis; as marginal (Figure 2) when the cement reached but did not extend past the tip of the prosthesis; and as inadequate (Figure 3) when the cement did not reach the tip of the prosthesis [17]. Some cases are exampled in Figures 1-3.

Figure 1. Case of adequate cementation in a GSB III prostheses.

Figure 2. Case of marginal cementation in a GSB III prostheses.

Figure 3. Case of inadequate cementation in a GSB III prostheses.
The radiographs of the last medical appointment, which had to be at least 4 years after surgery (range 4-14 years), were also blindly evaluated by the same surgeon for signs of loosening.
Radiographic loosening was graded as type I when there was a radiolucent line between the cement and prosthetic interface of 1 mm or more involving less than 50% of the overall interface; as type II when involving more than 50% of the entire interface; as type III when involving the entire interface; and as type IV in the case of gross loosening(17) (Figures 4 and 5).

Figure 4. Case with a grade 4 loosening.
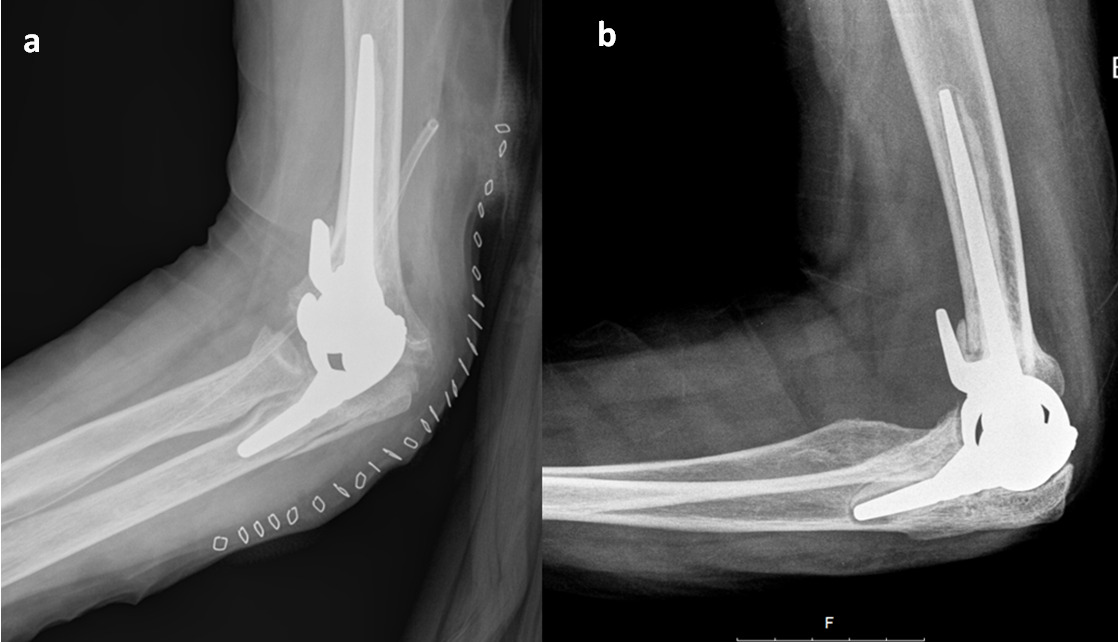
Figure 5. Case example. a) Immediate post-op radiograph showing inadequate and marginal cementation b) last follow-up radiograph showing grade III loosening.
The type of prosthesis placed, the surgical approach, surgery length, hospital length of stay, follow-up duration, complication rate, revision rate and prosthesis survival were also analyzed. Only all-cemented prostheses were selected.
As clinical outcomes, the arc of mobility and the QuickDASH Score were evaluated.
With all this data collected, it was then evaluated whether cementation quality had an influence on clinical and radiological results.
A minimum follow-up of 4 years was required.
Surgical procedure
The patient is placed in the full lateral position with the upper arm horizontal and the forearm hanging vertically. A midline posterior incision on the skin is used, avoiding the skin on the olecranon tip. The ulna nerve is identified proximally in the epineural fat at the medial border of the medial head of triceps and meticulous dissection is carried out distally to the first motor branch of the flexor carpi ulnaris. In all of the cases triceps sparing approach was used [18]. The cement is introduced into the humerus in a viscous state using a cement gun, followed by pressure packing. Cement is then inserted into the ulna canal using the same technique as in the humerus but with a thinner cannula. The prosthesis insertion was according to the standard manufacturer’s brochure technique for each prosthesis. An ulnar nerve transposition was typically not needed.
Post-operative care
A splint was applied with the elbow at 90 degrees of flexion; this remained in place until post-operative day 7. Passive range of motion (ROM) exercise was started around postoperative day 7, followed by active ROM exercise after post-operative day 14. By post-operative day 21–28, the active range of motion was expected to improve from 30 to 125 degrees in extension and flexion. A full range of daily activities was permitted after 6 weeks [17].
Statistical analysis
Descriptive statistics were calculated. Chi-square, t-test and Mann-Whitney U-test, depending on the variable analyzed, were used to compare different degrees of cementation with the clinical outcomes. A specific analysis for the most used prosthesis (GSB III) was also made.
A multivariate analysis was performed to explore the effects of potential confounders on the outcomes measured. Kaplan-Meier curves were used for the survival analysis. Pearson product-moment correlation was run to determine the relationship between radiological loosening and clinical outcomes.
Results
A total of 31 TEA were identified (Table 1). There were 23 women (two with bilateral TEA) and 6 men, with a mean age of 59 ± 15 years (28-81).
| Number of TEA (n) |
31 |
| Patients (bilateral) |
29 (2) |
| Female: Male |
23:6 |
| Mean Age, years |
59 ± 15 (28-81) |
| % Rheumatoid Arthritis |
52% (15) |
| Surgical time, min |
129 ± 31 (78-195) |
| Hospitalization time, days |
3.5 ± 1.5 (2-7) |
| Mean follow-up, years |
8 (4-13) |
| TEA: Total Elbow Arthroplasty | |
Table 1: Sample Characteristics.
Rheumatoid arthritis was the most common diagnosis for TEA, accounting for about 50% of cases, followed by post-traumatic arthritis in 35% of cases. There was no statistical difference in terms of the outcomes measured (clinical, revision rate, complication rate or survival) when we consider different type of diagnosis for the indication of the TEA.
The surgery took on average 129 ± 31 minutes (78-195), with the triceps sparing approach being the preferred one in all of the cases. The mean time of hospitalization was 3.5 ± 1.5 days (2-7).
The semi-constrained prosthesis GSB III (Zimmer®) was the most frequently used prosthesis in 13 cases (42%). The other prosthesis used were Latitude (Tornier®) (n=7), Discovery (Biomet®) (n=4), Conrad Morrey (Zimmer®) (n=4) and Nexel (Zimmer®) (n=3). All prosthesis used were cemented (Table 2).
| GSB III , Zimmer® |
13 (42%) |
| Latitude, Tornier® |
7 (23%) |
| Discovery, Biomet® |
4 (13%) |
| Conrad Morrey, Zimmer® |
4 (13%) |
| Nexel, Zimmer® |
3 (9%) |
| All of the prostheses were full cemented and semi-constrained type. | |
Table 2. Types of Prostheses (%).
The minimum follow-up for this study was 4 years (range 4-13) with a mean follow-up of 8 years.
The overall median survival of the prostheses was 82 months. The GSB III prosthesis had the highest median survival of 111 ± 44 months compared to the remaining prostheses with a median survival of 71 ± 40 months. Although not statistically significant (p=0.092), this difference was considered clinically relevant, despite the reduced number of cases.
The overall 2- and 5- year survival rate was 86% and 75%, respectively.
The overall 5- year survival rate for the GSB III prosthesis which was the most used prosthesis was 85%.
There was a 50% rate of postoperative complications and a revision rate of 26%. Considering all the 31 TEAS, 8 of them (26%) needed revision with a mean follow-up of 8 years.
The complications that needed revision were the 4 cases of aseptic loosening (Figures 4 and 5), 3 cases of infection and 1 case of periprosthetic fracture following trauma. The other 7 cases of complication were: 1 case of radial nerve lesion, 2 cases of permanent sensitive neuropathy of the cubital nerve, 2 cases of triceps ruptures and 2 cases of ankylosis.
In general, patients were reasonably satisfied with the surgery. Considering only the patients that didn’t need a revision surgery the Quick DASH score at the time of the study was on average 37 ± 17. When we consider all patients involved in the study the Quick DASH score was on average 50 ± 26.
Patients with depression (n=6) had worse Quick DASH scores (83 ± 11) and a higher prosthesis revision rate (50%).
The arc of mobility, evaluated in all cases at 1 year of follow-up, was on average 15º to 115º extension/flexion and 55º to 60º promo/supination.
Cubital cementation was adequate in 39% of cases, marginal in 58% of cases and inadequate in one case (3%). Humeral cementation was adequate in 51% of cases, marginal in 46% of cases and inadequate in one case (3%).
Patients with an inadequate or marginal ulnar cementation are 9.2 times more likely of having a cubital loosening at >50% of the prosthesis interface (p<0.05; OR=9.2 [95% CI 1-91]).
However, curiously, inadequate or marginal humeral cementation did not have a statistically significant association with the presence of humeral loosening at >50% of the interface (p=0.27).
In our sample, there were 4 cases of aseptic loosening requiring revision. In all of them there was marginal or inadequate cementation in one of the components (Figures 4 and 5).
There was no need for revision in the cases with adequate cementation.
Applying the spearman correlation, it was possible to demonstrate that there is no correlation between the degree of cubital or humeral radiological loosening and the Quick DASH Score (p>0.05).
Looking specifically at the most used prosthesis GSB III (n=13), we also found a statistical association between inadequate/marginal cubital cementation and grade 3/4 loosening (p=0.043). Of the 13 cases, 5 cases had inadequate or marginal ulnar cementation and 2 of those cases ended up needing revision due to aseptic loosening.
Discussion
TEA is an uncommon surgery and still not well studied comparing with other arthroplasties. This work highlighted the importance of adequate cementation and the importance of radiological evaluation.
When we look at the report from the Norwegian Arthroplasty Register [10] with 838 total elbow replacements analyzed, cement was used for fixation of both components in 641 cases. In 153 cases, only the ulnar component was cemented and in 5 cases, only the humeral component was cemented. In 26 cases, none of the components were fixated with cement. They found that the cases with an uncemented ulna component regardless of humeral fixation (n=31) had a 3 times higher risk for revision compared with those with a cemented ulnar component (RR, 2.98; 95% CI, 1.55-5.72; P=0.001). Although the use of cement for the humeral component did not influence survival, cementation of the ulnar component was associated with increased prosthesis survival.
This report also supports our results on the importance of adequate ulnar cementation, since we found that an inadequate or marginal ulnar cementation is 9.2 times more likely of having a loosening. Another study by Heide et al., found also that the revision of the ulna component was more likely with uncemented fixation than with cemented fixation [19].
In some previous studies, the ulnar component has been said to be the component more prone to loosening [10,19,20], and this also may be an explanation to our results.
The importance of cementing techniques in reducing aseptic loosening has been shown in several midterm and long-term follow-up studies. Morrey et al. [15] found that the loosening rate in their series correlated inversely with success in eliminating radiolucent lines at the bone-cement interface and in ensuring that the cement extended past the tip of the prosthesis. Schneeberger et al., [17] also showed a significant association between poor cementing technique and occurrence of loosening of the humeral component.
Our results, also supports the fact that poor ulnar cementation may predict radiological loosening and eventual need for revision.
According to numerous papers, the most frequent cause of revision TEA is aseptic loosening [10,20,21]. That was also the case in our study, representing 50% of the revision cases (4 in 8). In all of them marginal or inadequate cementation was found in one of the components.
Our overall 5- year survival rate was 75%. For the GSB III, which was the most used prostheses, the 5- year survival rate was 85%. This increased survival with the GSB III may be explained by the larger experience of the elbow team in our hospital with this prosthesis and also because they are one of the most recent prostheses used. However, this overall survivorship is slightly inferior to the one found in other studies. The overall 5-year survivorship of the Norwegian registry was 92% (10). This is similar to the results in the Finnish register [22] and the Danish register [1]. In a study on knee arthroplasty, the investigators found a significantly higher revision rate at low-volume hospitals compared with high-volume hospitals [23]. In a study from the Scottish register [24], better survival rate of the implants of surgeons who perform >10 cases per year were demonstrated. It is reasonable to believe that the same goes for TEA in our hospital, which has a mean of 3 cases per year.
It should be noted that despite the experienced team of elbow surgeons and fulfilled the manufacturer's recommendations, marginal cementation was found in a large number of cases. It will be important in the future to obtain more effective cementation methods such as high viscosity cement, restrictors and more suitable cementation cannulas for the diameter of the medullary canal of the humerus and ulna in order to place and hold the cement distally to the tip of the stem.
Furthermore, patients with fracture sequelae have been found to have higher risk of revision compared with those with inflammatory arthritis [10,25]. In our study, there was also a high number of TEA used for diagnosis other than inflammatory arthritis, like post-traumatic arthritis in 35% of the cases, and this also may explain our poorest results in terms of survivorship. Despite this slightly inferior survivorship, our patients were generally satisfied with the surgery and had reasonable QuickDASH Score (average 37 ± 17).
Our study as the limitation of being a relatively small cohort, however, it is the largest sample analyzed in the Iberian Peninsula and done only at one center. Unlike hip and knee replacements, where a larger number of cases are operated upon, most series of total elbow replacement have small samples. A larger study involving multiple centers would provide adequate number of cases to validate the utility of this specific cementation criterion as a predictor of failure.
TEA is an uncommon surgery and still not well studied comparatively with other arthroplasties. This work highlighted the importance of adequate cementation and the importance of radiological evaluation.
From this study, we can conclude that poor ulnar cementation may predict radiological loosening and eventual need for revision. However, this detachment does not correlate with the patient's symptomatology or degree of disability, which is why many patients with radiological detachment had no need for revision.
References
2. R. D. Elbow Arthroplasty. Proc R SocMed. 1969;62:1031-5.
3. Dee R. Total replacement arthroplasty of the elbow for rheumatoid arthritis. The Journal of Bone and Joint Surgery. British Volume. 1972 Feb;54(1):88-95.
4. Friedman RJ, Lee DE, Ewald FC. Nonconstrained total elbow arthroplasty: development and results in patients with functional class IV rheumatoid arthritis. The Journal of Arthroplasty. 1989 Jan 1;4(1):31-7.
5. Kudo H, Iwano K. Total elbow arthroplasty with a non-linked surfacereplacement prosthesis in patients who have rheumatoid arthritis. A long-term follow-up study. J Bone Jt Surg Am. 1990;72:355-62.
6. Madsen F, Gudmundson GH, Søjbjerg JO, Sneppen O. The Pritchard Mark II elbow prosthesis in rheumatoid arthritis. Acta Orthopaedica Scandinavica. 1989 Jan 1;60(3):249-53.
7. O'Driscoll SW, An KN, Korinek SA, Morrey BF. Kinematics of semi-constrained total elbow arthroplasty. The Journal of Bone and Joint Surgery. British Volume. 1992 Mar;74(2):297-9.
8. Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. Journal of Shoulder and Elbow Surgery. 2009 May 1;18(3):449-56.
9. Gschwend N. Present state-of-the-art in elbow arthroplasty. Acta Orthopaedica Belgica. 2002 Apr 1;68(2):100-17.
10. Krukhaug Y, Hallan G, Dybvik E, Lie SA, Furnes ON. A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994-2016. Journal of Shoulder and Elbow Surgery. 2018 Feb 1;27(2):260-9.
11. Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. The Journal of Bone and Joint Surgery. British Volume. 2011 Mar;93(3):293-7.
12. Patil N, Cheung EV, Mow CS. High revision rate after total elbow arthroplasty with a linked semiconstrained device. Orthopedics (Online). 2009 May 1;32(5):321.
13. Aldridge JM, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis. Journal of Bone and Joint Surgery-Series B. 2006;88(4):509-14.
14. Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. The Journal of Bone and Joint Surgery. 1998 Sep 1;80(9):1327-35.
15. Morrey BF, Bryan RS, Dobyns JH, Linscheid RL. Total elbow arthroplasty. A five-year experience at the Mayo Clinic. The Journal of Bone and Joint Surgery. American Volume. 1981 Sep 1;63(7):1050-63.
16. Corradi M, Frattini M, Panno B, Tocco S, Pogliacomi F. Linked semi-constrained total elbow prosthesis in chronic arthritis: results of 18 cases. Musculoskeletal Surgery. 2010 May;94(1):11-23.
17. Schneeberger AG, Hertel R, Gerber C. Total elbow replacement with the GSB III prosthesis. Journal of Shoulder and Elbow Surgery. 2000 Mar 1;9(2):135-9.
18. Pierce TD, Herndon JH. The triceps preserving approach to total elbow arthroplasty. Clinical Orthopaedics and Related Research®. 1998 Sep 1;354:144-52.
19. Van Der Heide HJ, De Vos MJ, Brinkman JM, Eygendaal D, Van Den Hoogen FH, de Waal Malefijt MC. Survivorship of the KUDO total elbow prosthesis—comparative study of cemented and uncemented ulnar components: 89 cases followed for an average of 6 years. Acta Orthopaedica. 2007 Jan 1;78(2):258-62.
20. Ikävalko M, Tiihonen R, Skyttä ET, Belt EA. Long-term survival of the Souter-Strathclyde total elbow replacement in patients with rheumatoid arthritis. The Journal of Bone and Joint Surgery. British Volume. 2010 May;92(5):656-60.
21. Little CP, Graham AJ, Carr AJ. Total elbow arthroplasty: a systematic review of the literature in the English language until the end of 2003. The Journal of Bone and Joint Surgery. British Volume. 2005 Apr;87(4):437-44.
22. Skyttä ET, Eskelinen A, Paavolainen P, Ikävalko M, Remes V. Total elbow arthroplasty in rheumatoid arthritis: a population-based study from the Finnish Arthroplasty Register. Acta Orthopaedica. 2009 Jan 1;80(4):472-7.
23. Badawy M, Espehaug B, Indrekvam K, Engesæter LB, Havelin LI, Furnes O. Influence of hospital volume on revision rate after total knee arthroplasty with cement. The Journal of Bone and Joint Surgery. 2013 Sep 18;95(18):e131.
24. Jenkins PJ, Watts AC, Norwood T, Duckworth AD, Rymaszewski LA, McEachan JE. Total elbow replacement: outcome of 1,146 arthroplasties from the Scottish Arthroplasty Project. Acta Orthopaedica. 2013 Jan 1;84(2):119-23.
25. Kraay MJ, Figgie MP, Inglis AE, Wolfe SW, Ranawat CS. Primary semiconstrained total elbow arthroplasty. Survival analysis of 113 consecutive cases. The Journal of Bone and Joint Surgery. British Volume. 1994 Jul;76(4):636-40.
