Abstract
Background: Systemic lupus erythematosus (SLE) is characterized by diverse symptoms including fever, joint pain, facial rash, blood in urine, and sores in the mouth. Neuropsychiatric SLE (NPSLE) refers to neurological and psychiatric manifestations in SLE patients after exclusion of other potential causes.
Case Presentation: A 21-year-old woman with established lupus nephritis presented with left-sided weakness, aphasia, confusion and focal neurological deficits. Imaging studies demonstrated multiple infarcts and central nervous system (CNS) vasculitis. Treatment with intravenous methylprednisolone and antibiotics led to clinical improvement.
Discussion: CNS vasculitis is a rare complication of SLE, manifesting as seizures, cognitive impairment, or stroke-like symptoms. MRI and angiographic studies aid in diagnosis, while early treatment with steroids and cyclophosphamide improves prognosis. Prompt immunosuppressive therapy is essential for better patient outcomes.
Conclusion: This case highlights the importance of recognizing NPSLE in lupus patients with neurological symptoms and underscores the necessity for timely diagnosis and intervention to mitigate potential morbidity.
Keywords
Neuropsychiatric Systemic Lupus Erythematosus (NPSLE), Lupus nephritis, Central nervous system vasculitis, Methylprednisolone, Immunosuppressive therapy
Introduction
Systemic lupus erythematosus (SLE) is a disease characterized by diverse symptoms including fever, joint pain, facial rash, blood in urine, and sores in the mouth. Neuropsychiatric SLE (NPSLE) refers to the neurological and psychiatric conditions seen in SLE patients, after ruling out other potential causes [1]. Diagnosing NPSLE presents significant challenges due to its wide range of clinical symptoms. Currently, there are no specific lab tests or imaging studies that can definitively diagnose NPSLE or aid in therapeutic decision-making. Typically, NPSLE symptoms appear early in the disease progression of SLE, predominantly affecting young women. Up to 45% of individuals with SLE may experience NPSLE, significantly contributing to the disease’s morbidity [2]. The development of NPSLE involves a complex interplay of factors, including various inflammatory cytokines, antibodies, and immune complexes, leading to damage of neurons through vasculopathy, cytotoxic, and autoantibody-mediated mechanisms [3].
CNS vasculitis remains a rare and underreported manifestation of SLE in the literature, highlighting the importance of increased clinical awareness and documentation through case reports. We present a rare case of CNS vasculitis in a patient with SLE and lupus nephritis.
Case Presentation
We describe a case of 21-year-old female presented with sudden onset of left-sided weakness, aphasia, and confusion. The patient was taking prednisolone and hydroxychloroquine for lupus nephritis when these symptoms suddenly developed.
On examination, the patient was vitally stable with a blood pressure of 145/90 mmHg and a Glasgow Coma Scale (GCS) score of 11/15. Cranial nerves were intact. Muscle tone was decreased in both the upper and lower limbs on the left side, while it was normal on the right side. Muscle strength was 1/5 in both the upper and lower limbs on the left side and 4/5 in both limbs on the right side. Reflexes were normal on the right side but brisk on the left side in both limbs, with an upgoing plantar reflex. Chest examination revealed bilateral basal crepitations, while the cardiovascular examination was unremarkable. The abdomen was soft and non-tender.
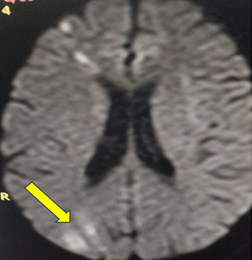
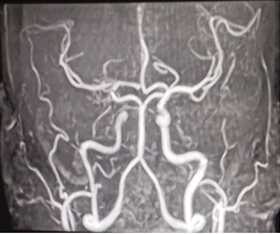
Laboratory investigations, including full blood count, renal profile, serum electrolytes, viral profile, and C-reactive protein, were within normal limits while the erythrocyte sedimentation rate (ESR) was raised. Liver function tests showed a mildly elevated ALT (Table 1). A 24-hour urinary protein test revealed a total protein of 2,694 mg. Urine analysis showed 15–20 pus cells and urine culture indicated heavy growth of Klebsiella. As part of the diagnostic workup, cerebrospinal fluid (CSF) analysis was performed to rule out infectious or inflammatory etiologies of central nervous system involvement. The CSF results were within normal limits, with no evidence of infection, elevated protein, or pleocytosis. Additionally, a thorough cardiac evaluation—including echocardiography and electrocardiogram—was conducted to exclude cardioembolic sources of stroke. Both investigations were unremarkable, supporting the diagnosis of CNS vasculitis secondary to systemic lupus erythematosus. MRI of the brain (Figures 1–3) revealed Cortical based areas of abnormal signal intensities involving right frontal lobe & right posterior parietal and occipital lobes predominantly in the watershed zones appearing hyperintense on T2/FLAIR, hypointense on T1WI showing diffusion restriction on DWI. Right head of caudate and lentiform nucleus show similar signal intensities appearing hyperintense on T2/FLAIR, hypointense on T1WI showing diffusion restriction on DWI. The Computed Tomography Angiogram (CTA) and Magnetic Resonance Angiogram (MRA) (Figure 4) also demonstrated multiple vessel stenoses. Although the calabrese’s criteria is used for diagnosis primary angiitis/vasculitis of the CNS; for secondary causes the diagnosis is based on radiological findings in the setting a systemic inflammatory disease (SLE in our case), in rare cases a brain biopsy may be needed to confirm the diagnosis.
Figure 1. Axial T2-weighted MRI of the brain revealing multiple acute infarcts in the right hemisphere, predominantly in the parietal, occipital, and temporal lobes.
Figure 2. Axial FLAIR MRI view of the brain highlighting the extent of infarcts in the right hemisphere, with significant involvement of the posterior cerebral artery territory.
Figure 3. Axial T1-weighted MRI of the brain showing the infarcts in the right hemisphere, with emphasis on the involvement of deep white matter regions.
Figure 4. MRA demonstrating multiple vessel stenoses, particularly in the right middle cerebral artery and posterior circulation.
|
Investigation |
Result |
Normal Range |
|
TLC |
10.7 |
4–11 |
|
DLC
|
Neutrophils: 74% |
40–75% |
|
Lymphocytes: 20% |
20–45% |
|
|
Monocytes: 4% |
2–10% |
|
|
Hemoglobin |
14 g/dL |
12–16 g/dL |
|
Platelets |
228 x 10^3/μL |
150–450 x 10^3/μL |
|
Blood urea |
34.45 mg/dL |
18–45 mg/dL |
|
Creatinine |
0.46 mg/dL |
0.1–1.0 mg/dL |
|
Liver profile
|
Bilirubin: 0.46 mg/dL |
0.1–1.0 mg/dL |
|
ALT: 191 U/L |
10–50 U/L |
|
|
ALP: 58 U/L |
35–104 U/L |
|
|
ESR |
60 mm/1st hr |
0–20 mm/1st hr |
|
CRP |
0.4 mg/dl |
<1.0 mg/dl |
|
Serum electrolytes
|
Sodium: 104 mmol/L |
135–150 mmol/L |
|
Potassium: 3.9 mmol/L |
3.5–5.0 mmol/L |
|
|
Chloride: 104 mmol/L |
98–108 mmol/L |
|
|
Viral profile
|
HbsAg: Negative |
Negative |
|
Anti-HCV: Negative |
Negative |
During her hospital stay, the patient received intravenous methylprednisolone 1 gram daily for five days, leading to a marked clinical improvement. Her Glasgow Coma Scale (GCS) score improved from 11/15 on admission to a full score of 15/15. Neurologically, there was partial recovery in motor function, with muscle strength improving from 1/5 to 3/5 on the left side in both upper and lower limbs by the time of discharge. Although some residual weakness persisted, the patient was able to follow commands, articulate short phrases, and engage in basic daily activities with assistance. She was also treated with ceftriaxone for her urinary tract infection and showed complete resolution of systemic symptoms. The patient was discharged on a maintenance regimen including Prednisolone, Mycophenolate mofetil, and cyclophosphamide, with plans for outpatient physiotherapy and close neurology follow-up to monitor further neurological recovery.
Discussion
Systemic Lupus Erythematosus (SLE) is an autoimmune condition with manifestations of clinical signs and reportable symptoms being a clue to the multi-systemic effects that it can cause. Any organ can be affected, from CNS and kidneys to mesothelial and hematopoietic systems. CNS involvement has been reported in the younger demographic groups with more advanced disease with symptoms including seizures, defective cognition, psychotic features, cranial neuropathy, and vascular involvement [4].
CNS can be involved in 30–40% of cases but due to its complex and variable presentation, the diagnosis can be a challenging task and usually not the first one in the list of differentials [5–7]. The vessels in the CNS can be involved as well exhibiting symptoms with resemblance to other diseases of the central nervous system like hematomas, memory loss, infections, and stroke [6–8]. The involvement of vessels is in the form of vasculitis with the vessels appearing thick-walled with a narrow lumen when studied with brain Magnetic Resonance Imaging (MRI) [6]. The consequences can be dramatic and variable, often leading to neurological deficits and diminished quality of life. Vessels may become weakened and leaky, leading to hemorrhage, or may become occluded, causing ischemia of the supplied territory [8,9]. Angiographic images can narrow down the list of possible causes and can be beneficial in ruling out some of the common causes including atherosclerosis [10].
Several case reports illustrate the severity and complexity of CNS vasculitis in SLE. One such case involved a 41-year-old man who developed seizures, cognitive impairment, and myalgia following a respiratory infection. Further investigations confirmed SLE with antiphospholipid syndrome and cerebral vasculitis. Immunosuppressive therapy led to improved MRI findings, emphasizing the need to consider SLE in young patients presenting with neuropsychiatric symptoms [11].
A case series was published which showed that four cases of SLE after 16 years of diagnosis present with CNS vasculitis. MRI showed thickening of vascular walls and ischemic brain changes, as well as vascular stenosis. These patients showed improvement on imaging studies following treatment with glucocorticoids and cyclophosphamide [7].
A retrospective study involving 41 patients with SLE revealed that primary CNS involvement was not rare, but there was an unexpected rise in movement disorders. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were within the normal range [12].
Additionally, a case report described a neonate presenting with ischemic stroke associated with SLE, with no other manifestations [10]. Another patient presented with psychosis without any other manifestation of SLE. The patient was using acenocoumarol for amaurosis fugax and had low titers of ANAs and anti-dsDNA antibodies, low enough to develop NPSLE [13].
In a case report, a 62-year-old woman initially diagnosed with cerebral infarction, suspected to be due to atherosclerosis. However, recurrent strokes prompted further investigation, and vessel wall MRI revealed arterial wall enhancement, confirming cerebral arteritis. This case highlights the insidious progression of medium-sized arteritis in SLE, which may lead to vascular occlusion regardless of disease activity [9].
Similarly, a case of neuropsychiatric systemic lupus erythematosus (NPSLE) described a female patient presenting with stroke-like symptoms, headache, vertigo, and palpable purpura. Further investigations confirmed large-vessel cerebral vasculitis alongside cutaneous small-vessel vasculitis. This case underscores the rarity of cerebral large-vessel involvement in SLE and its varied clinical presentation [14].
The CNS involvement is not limited to the younger and elderly population. Even the newborns are not spared and exhibit symptomatic stroke with the unfortunate fate of having permanently damaged CNS vessels for the rest of their lives [15]. Though the prognosis can be good with prompt treatment initiatives, it requires a high index of suspicion and vigilance on the part of the attending physician [16].
CNS vasculitis should be amongst the top differentials in any patient with pre-existing SLE. Diagnosis requires a CT scan followed by an MRI with a brain biopsy reserved for inconclusive and suspicious cases. A much favorable prognosis can be expected by early institution of a regimen including initial intravenous administration of high-dose steroids which is followed by a prolonged course of oral cyclophosphamide and steroids [14].
Conclusion
CNS vasculitis in SLE is a rare but serious complication requiring early recognition. Our case highlights the importance of MRI and angiographic studies in diagnosis and differentiation from other cerebrovascular conditions. Prompt treatment with high-dose steroids and cyclophosphamide is essential for better outcomes. Although our patient improved significantly, our observations were only for short term. Further high quality prospective studies are needed to address long term outcomes in such patients.
Data Availability
All the relevant data regarding the patient is available upon reasonable request from the corresponding author.
Acknowledgment
None
Conflict of Interest
The authors have no conflict of interest to declare
Funding
None
Patient Consent
Informed consent was signed by the patient’s father.
Author Contribution
Abdul Majid and Ayub Khan wrote the original manuscript and did supervision. Muhammad Osama and Shahid Ali did data curation and formal analysis. Muhammad Noman, Hafsa Salim and Farhan Shahzad contributed to writing the original draft, review and editing. All authors have contributed in conception and design of the study and final approval of the manuscript.
References
2. Magro–Checa C, Zirkzee EJ, Huizinga TW, Steup–Beekman GM. Management of neuropsychiatric systemic lupus erythematosus: current approaches and future perspectives. Drugs. 2016 Mar;76(4):459–83.
3. Liu Y, Tu Z, Zhang X, Du K, Xie Z, Lin Z. Pathogenesis and treatment of neuropsychiatric systemic lupus erythematosus: A review. Front Cell Dev Biol. 2022 Sep 5;10:998328.
4. Pawlak–Buś K, Schmidt W, Leszczyński P. Neuropsychiatric manifestations and their attribution to systemic lupus erythematosus: a retrospective single–center study in a Polish population. Polish Archives of Internal Medicine. 2022 Nov 25;132(11):16319.
5. Abraham P, Neel I, Bishay S, Sewell DD. Central nervous system systemic lupus erythematosus (CNS–SLE) vasculitis mimicking Lewy body dementia: a case report emphasizing the role of imaging with an analysis of 33 comparable cases from the scientific literature. Journal of Geriatric Psychiatry and Neurology. 2021 Mar;34(2):128–41.
6. Mishima K, Ayano M, Nishida T, Tatsutani T, Inokuchi S, Kimoto Y, et al. Use of 18F–Fluorodeoxyglucose–Positron Emission Tomography/Computed Tomography to successfully diagnose central nervous system vasculitis in systemic lupus erythematosus and antiphospholipid syndrome: a case report. Modern Rheumatology Case Reports. 2021 Jul;5(2):278–84.
7. Rodrigues M, Galego O, Costa C, Jesus D, Carvalho P, Santiago M, et al. Central nervous system vasculitis in systemic lupus erythematosus: a case series report in a tertiary referral centre. Lupus. 2017 Nov;26(13):1440–7.
8. Habes YMN, Ahmaro M, Dwikat Y, Jobran AW, Abunejma FM, Abdulrazzak M. Stroke as an unusual initial presentation of ‘malignant’middle cerebral artery infarction involvement in systemic lupus erythematosus. Annals of Medicine and Surgery. 2023 Nov 16;86(1):517–21.
9. Nishigaichi A, Oiwa H, Hosokawa Y, Hayashi M, Mine N, Nomura E, et al. A case of systemic lupus erythematosus associated with cerebral arteritis: a case report and case–based literature review. Nagoya Journal of Medical Science. 2020 Nov;82(4):807–14.
10. Saini AG, Sankhyan N, Bhattad S, Vyas S, Saikia B, Singhi P. CNS vasculitis and stroke in neonatal lupus erythematosus: a case report and review of literature. European Journal of Paediatric Neurology. 2014 May;18(3):444–8.
11. Wolf J, Niedermaier N, Bergner R, Lowitzsch K. Zerebrale Vaskulitis als Erstmanifestation eines systemischen Lupus erythematodes. DMW–Deutsche Medizinische Wochenschrift. 2001 Aug 24;126(34–35):947–50.
12. Joseph FG, Lammie GA, Scolding NJ. CNS lupus: a study of 41 patients. Neurology. 2007 Aug 14;69(7):644–54.
13. Rowshani A, Remans P, Rozemuller A, Tak P. Cerebral vasculitis as a primary manifestation of systemic lupus erythematosus. Annals of the Rheumatic Diseases. 2005 May;64(5):784–6.
14. Böckle B, Jara D, Aichhorn K, Junker D, Berger T, Ratzinger G, et al. Cerebral large vessel vasculitis in systemic lupus erythematosus. Lupus. 2014 Nov;23(13):1417–21.
15. Chen C, Huang J, Hsu J, Chung C, Lin K. Neonatal lupus complicated by hemorrhagic stroke. Lupus. 2012 Dec;21(14):1582–5.
16. Kang I, Hutchinson G. Central nervous system vasculitis in systemic lupus erythematosus: a case successfully treated with cyclophosphamide and steroids. JCR: Journal of Clinical Rheumatology. 1997 Dec;3(6):349–52.