Abstract
Purpose: Routine inpatient EEGs have been part of epilepsy practices for years. We aim to improve current routine EEG practices by studying their role at a large university hospital. Methods: Inpatient routine EEGs from January-July 2021 were included and patients <5 yrs., EEGs repeated on the same patient were excluded. Indications, floor status, abnormality, day of study, neurology consultation, results, treatment changes, discharge status, and prior AED use were analyzed using SAS 9.4. Results: The mean age for 250 patients was 57.27 yrs., where 54.22% were males and 45.78% were females. Indications listed were 26.5% altered mental status, 59.83% seizures, and 13.65% others. 87.36% of ICU patients had abnormal EEG vs 73.75% of floor patients. A significant association (p=0.0147) was found between floor status and EEG results. Abnormalities were 44% generalized slowing, 23.6% focal slowing, 9.2% epileptiform activity, and 23.2% others. Treatment was changed in 21.03% with abnormal vs 5.56% with normal EEG. AEDs were added in 18.46% with abnormal vs 3.7% with normal EEG. A significant association (p=0.014) was found between Neurology consultation and treatment change and with AED addition respectively. EEG result was associated with treatment change and AED addition. “Abnormal EEG” was significantly associated with further study. A significant association (p=0.0351) was found between EEG results and discharge status. 53.82% of patients were not on AED before EEG vs 46.18%. Prior AED had no association with EEG results. Conclusions: It is helpful to consult Neurology. Longer duration of routine EEGs may not show abnormalities. Routine EEG facilitates discharges and guides further workup.
Keywords
Routine EEG, Epilepsy research, Quality improvement, Clinical practice, Hospital practice
Abbreviations
rEEG: Routine EEG; cEEG: Continuous EEG; AED: Antiepileptic Drug; IRB: Institutional Review Board
Introduction
EEG is a non-invasive and benign tool, that detects electrical activity in the brain. The minimum duration of EEG recording should be 20 min [1]. EEG is not only used to confirm or rule out seizures, but it is also indicated in the evaluation of cognitive change, syncope, psychiatric presentations, movement disorders (e.g., myoclonus, tremors), or unexplained unresponsiveness [2].
Interestingly, EEG can provide important information even when CT and MRI findings are normal [3]. EEG also helps in diagnosing status epilepticus as a cause of altered mental status or even when the patient is alert. Routine EEG in comatose patients after cardiac arrest helps in determining prognosis at the same time rules out seizures [4].
Routine EEG plays an important role in making a treatment plan, it has been studied to assess the effectiveness of anti-epileptic drug therapy and seen to help in safely weaning off anti-epileptic drugs in patients. It can assist in classifying seizure types as a result and adds to the appropriate selection of AED [5]. The yield of routine EEG increases with video monitoring and when used in an appropriate setting with provocation measures. It is also more helpful when performed sooner rather than later [6,7].
It is a reasonable alternative option over continuous EEG in resource-limited centers [8]. There are certain limitations to the use of routine EEG which included a short duration of recording and due to that, it may not record epileptiform discharges. There can also be inter-observer variability.
We felt the need to re-evaluate the relevance of routine EEG in inpatient settings as in current practices there are new and several modalities coming up to screen seizures. It has been found as a great screening tool previously but also it is important to evaluate its utility in disposition and treatment plans and the contributory factors.
Methods
It is a retrospective, observational study. Patients who underwent inpatient routine EEGs from January to July 2021 were included and those patients who were less than 5 years old and repeat studies on patients during the 6-month period were excluded. IRB approval was waived as this was a quality improvement project.
Included patient charts were reviewed for indications, floor status( ICU vs floor), neurology consultation (whether Neurology was involved or not), day of study (whether it was a weekday vs weekend, findings of the study, if any further workup was pursued if routine EEG was repeated within 10 days or not, if treatment was changed, whether an AED was added on the basis of the findings, if routine EEG helped in expediting discharge, total duration of the studies, and if patient was on prior AED at the time of the study.
Appropriate statistical analyses using SAS 9.4 were performed.
Results
From over 285 records found between January to July 2021, 250 patients were included. The mean age was noted to be 57.27 ± 19.05 years, and 54.22% were males and 45.78% were females. Among the listed indications during ordering the test, 26.5% of studies indicated altered mental status, 59.83% listed seizures and 13.65% listed a mix of other indications. The median duration of routine EEG was 37 minutes.
ICU vs floor status
The majority (64.52%) of study participants were on the floor while 35.48% of them were in the ICU. There was a significant (p=0.0147) association between ICU/Floor location and EEG results (Table 1). Of those who were in the ICU, 87.36% of them had an abnormal EEG versus 73.13% of those who were on the Floor.
Abnormal EEG
Among abnormalities reported, 44% were noted to have generalized slowing, 23.6% showed focal slowing, 9.2% showed some epileptiform activity and 23.2% included other findings. Out of the studies reporting abnormal EEGs, only 4.66% were found to record seizures. There was a significant (p=0.0085) association of abnormal EEG results with the addition of an AED (Table 1). Treatment was changed in 20.92% with abnormal EEG while only 5.66% with normal EEG had a change in treatment. AEDs were added in 18.46% of patients with abnormal EEG vs 3.7% with normal EEG.
Neurology consultation
There was a significant (p=0.014) association between the treatment change and a neurology consultation. 97.73% of the study subjects who had a treatment change, also had a neurology consultation. 84.39% of those who did not still have a neurology consultation. Regarding AED addition for management, 18.37% of the participants that received abnormal EEG results had an addition of an AED. Only 3.77% percent of the individuals who had normal EEG results, had an addition of an AED. It was noted that there was a significant (p=0.037) association between the addition of an AED and neurology consultation (Table 1).
97.37% of the participants who had an AED added, also had a neurology consultation. For those who did not have an AED added, 84.83% of them received a neurology consultation. Significant association was found between Neurology consultation with treatment change and AED addition respectively.
|
Variables |
Normal EEG n (%) |
Abnormal EEG n (%) |
|
Floor n (%) |
42 (26.25) |
118 (73.75) |
|
ICU n (%) |
11 (12.64) |
76 (87.36) |
|
Two-sided p value = 0.0147, missing=3 |
||
|
Further diagnostics done |
5 (9.43) |
43 (21.94) |
|
Further diagnostics not done |
48 (90.57) |
153 (78.06) |
|
Two-sided p value = 0.034, missing=1 |
||
|
Seizures present |
0 (0.00) |
9 (4.66) |
|
Seizures absent |
56 (100.0) |
184 (95.34) |
|
Two-sided p value = 0.211, missing=4 |
||
|
Treatment changed |
3 (5.66) |
41 (20.92) |
|
Treatment not changed |
50 (94.34) |
155 (79.08) |
|
Two-sided p value = 0.008, missing=1 |
||
|
Addition of AED |
2 (3.77) |
36 (18.37) |
|
No addition |
51 (96.23) |
160 (81.63) |
|
Two-sided p value = 0.0085, missing=1 |
||
|
Discharged early |
20 (37.74) |
45 (22.96) |
|
Discharged later |
33 (62.26) |
151 (77.04) |
|
Two-sided p value = 0.035, missing=1 |
||
|
Prior AED use |
19 (35.85) |
96 (48.98) |
|
No prior AED use |
34 (64.15) |
100 (51.02) |
|
Two-sided p value = 0.120, missing=1 |
||
|
|
Neurology consulted |
Neurology not consulted |
|
Treatment changed |
43 (97.73) |
1 (2.27) |
|
Treatment not changed |
173 (84.39) |
32 (15.61) |
|
Two-sided p value = 0.0139, missing=1 |
||
|
Addition of AED |
37 (97.37) |
1 (2.63) |
|
No addition |
179 (84.83) |
32 (15.17) |
|
Two-sided p value= 0.036, missing =1 |
||
|
|
Normal EEG |
Abnormal EEG |
|
Duration of rEEG (min) |
37 ± 12.75 |
37 ± 18.37 |
|
p value = 0.659 |
||
Further workup and AED use
Some patients needed workup beyond routine EEGs. We broadly categorized them into continuous EEGs, MRI Brain, or lumbar punctures. It was noted that further studies were done in 21.94% of patients with abnormal EEG and 9.43% with normal EEG.
Day of the week and discharges
There was no significant association between the day of the week and discharge status. However, of the participants who were discharged, the majority (27.69%) were discharged on a Monday. Very few were discharged on Saturdays or Sundays.
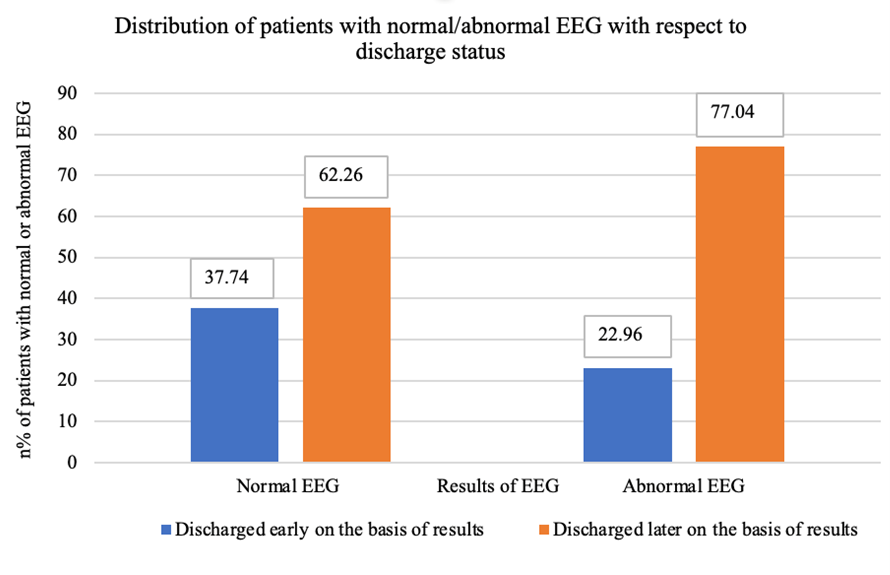
There was a significant (p=0.0351) association between EEG results and discharge status. 37.74% of individuals with a normal EEG were able to be discharged compared to only 22.96% of those with an abnormal EEG (Figure 1).
Figure 1. Distribution of patients with normal/abnormal EEG with respect to discharge status.
Use of AEDs prior to the study
There was a relatively even number of individuals who were on an AED prior to the EEG. 53.82% of individuals were not on an AED, while 46.18% of them were on an AED prior to the EEG. There was no significant association between prior use of AED and abnormal EEG results.
Duration of the EEG
We found that there was no significant association between the duration of routine EEG with abnormalities on EEG.
Discussion
Routine EEGs have been in use since the 1930s [10]. However, due to the presence of more complex testing and the increased ability of large hospitals to run continuous EEGs, it is helpful to revisit the indications for which routine EEGs are being ordered, the yield of the procedure and what are the best practices.
We found that most indications used were for “seizures” and the next most cited indication was “altered mental status”. Per American Epilepsy Society guidelines there is level B evidence to evaluate for new-onset seizures [11].
In our sample, 78% of the EEGs were abnormal. Out of the abnormal studies, only 9.2% showed epileptiform activity and only 4.6% recorded seizures. When EEG was ordered for an indication of new-onset seizure, Neufeld et al. showed that over 69% of their sample was abnormal, and over 21% showed epileptiform activity, and similar findings have been found in other studies [2,12].
However, we observed that there was a statistically significant association of higher abnormalities with ICU status, this suggests that there is a higher chance of having abnormal EEG in the ICU. This can be attributed to the fact that most patients in the ICU are likely to be more encephalopathic and may develop epileptogenesis due to secondary causes than the ones on the floor. This could give EEG results that show associated findings. Scozzafava et al. have described the inadequacy of a standard 20-minute routine EEG in ICU patients resulting in a low seizure detection rate and no association with outcomes. We extended research to all inpatient studies done, and all routine EEGs (standard or extended) to find the yield of the study overall and our sample size was relatively bigger [13].
Mussavi et al. have described the importance of abnormal CT and US findings for the cause of neonatal seizures and their use simultaneously with EEG in diagnosing seizures. We tried to further describe how routine EEGs were helpful as a screening tool and in changing management by itself and when further studies such as imaging were required. We also described the further use of MRI in our study [14].
The yield of routine EEG by itself may or may not help in determining the course of treatment, however involving Neurology opinion early may help in determining further treatment and workup.
Previous studies do not describe the importance of Neurology consultation for routine EEG. We found that regardless of abnormalities Neurology consults helped in changing treatment or adding AEDs. Currently, the hospital policy is to compulsorily consult Neurology when ordering a continuous EEG, but not necessarily for a routine EEG. However, it may save more time later, and expedite contingency plans if Neurology is involved earlier.
Only over 22% of patients who had abnormal findings received further testing. Multiple studies show that additional tests can help in increasing the yield of findings in patients [15].
Routine EEG results helped in the addition of an AED. It also helped in expediting discharge. One would think that continuous EEG studies than routine EEGs would expedite the discharge due to more findings and appropriate treatment plans, but it has been studied before that there is no difference in discharge between the two [16,17].
In our sample, the median study duration was 37 minutes, although there was no significant association of the duration with abnormalities on EEG. However, this duration is close to other studies that have found 40 minutes an optimal duration for a routine EEG [18].
The limitations of our study were that we did not compare the yield of a continuous EEG with the routine EEGs on the same patient. The duration of hospital stay was not accounted for, and disposition to rehab centers and skilled nursing were not considered. However, many of these patients had other problems which may or may not have contributed to the discharge status, confounders being socioeconomic reasons, age, primary disease, and other factors impending discharge.
Conclusion
Routine EEG still holds a lot of value in clinical practice. It helps in expediting discharges, and even changing management or adding AEDs. It also helps more when neurology is involved as a consulting team.
Conflicts of Interest
There are no conflicts of interest.
Funding Statement
There is no funding to be disclosed.
Authors Contribution
The principal Author has full access to the data and has the right to publish this data. All authors participated in a meaningful way in the preparation of the manuscript (in the design or conceptualization of the study, interpretation of data, or drafting manuscript).
References
2. Phamnguyen TJ, Szekely A, Swinburn S, Babu S, Boland-Freitas R, Reutens D, et al. Usefulness and yield of routine electroencephalogram: a retrospective study. Intern Med J. 2023 Feb;53(2):236-241.
3. Rodríguez Quintana JH, Bueno SJ, Zuleta-Motta JL, Ramos MF, Vélez-van-Meerbeke A, the Neuroscience Research Group (NeuRos). Utility of Routine EEG in Emergency Department and Inpatient Service. Neurol Clin Pract. 2021 Oct;11(5):e677-e681.
4. Westhall E, Rossetti AO, van Rootselaar AF, Wesenberg Kjaer T, Horn J, Ullén S, et al. Standardized EEG interpretation accurately predicts prognosis after cardiac arrest. Neurology. 2016 Apr 19;86(16):1482-90.
5. Hasan TF, Tatum WO. When should we obtain a routine EEG while managing people with epilepsy? Epilepsy Behav Rep. 2021 May 3; 16:100454.
6. Grau-López L, Jiménez M, Ciurans J, Barambio S, Fumanal A, Becerra J. Diagnostic Yield of Routine Electroencephalography With Concurrent Video Recording in Detecting Interictal Epileptiform Discharges in Relation to Reasons for Request: A Prospective Study of 1,080 Video-Electroencephalograms. Journal of Clinical Neurophysiology. 2017;34(5):434-437.
7. McGinty RN, Costello DJ, Kinirons P, McNamara B. Diagnostic Yield of Routine EEG in Adults with Active Epilepsy. Ir Med J. 2019 Jan 15;112(1):851.
8. Rossetti AO, Schindler K, Sutter R, Rüegg S, Zubler F, Novy J, et al. Continuous vs Routine Electroencephalogram in Critically Ill Adults With Altered Consciousness and No Recent Seizure: A Multicenter Randomized Clinical Trial. JAMA Neurol. 2020 Oct 1;77(10):1225-1232.
9. Williams GW, Lüders HO, Brickner A, Goormastic M, Klass DW. Interobserver variability in EEG interpretation. Neurology. 1985 Dec;35(12):1714-9.
10. Stone JL, Hughes JR. Early history of electroencephalography and establishment of the American Clinical Neurophysiology Society. J Clin Neurophysiol. 2013 Feb;30(1):28-44.
11. Krumholz A, Wiebe S, Gronseth GS, Gloss DS, Sanchez AM, Kabir AA, et al. Evidence-based guideline: Management of an unprovoked first seizure in adults: Report of the Guideline Development Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2015 Apr 21;84(16):1705-13.
12. Neufeld MY, Chistik V, Vishne TH, Korczyn AD. The diagnostic aid of routine EEG findings in patients presenting with a presumed first-ever unprovoked seizure. Epilepsy Res. 2000 Dec;42(2-3):197-202.
13. Scozzafava J, Hussain MS, Brindley PG, Jacka MJ, Gross DW. The role of the standard 20 minute EEG recording in the comatose patient. J Clin Neurosci. 2010 Jan;17(1):64-8.
14. Mussavi M, Khanzadeh S, Sadeghvand S, Hasanpour E, Akbari M, Nasiri S, et al. Evaluation of brain CT scan, sonography and EEG findings in neonates with seizure. Iran J Child Neurol. 2022 Jul 16;16(3):183-91.
15. Drenthen GS, Jansen JFA, Gommer E, Gupta L, Hofman PAM, van Kranen-Mastenbroek VH, et al. Predictive value of functional MRI and EEG in epilepsy diagnosis after a first seizure. Epilepsy Behav. 2021 Feb;115:107651.
16. Eskioglou E, Stähli C, Rossetti AO, Novy J. Extended EEG and non-convulsive status epilepticus: Benefit over routine EEG? Acta Neurol Scand. 2017 Sep;136(3):272-276.
17. Ney JP, van der Goes DN, Nuwer MR, Nelson L, Eccher MA. Continuous and routine EEG in intensive care: utilization and outcomes, United States 2005-2009. Neurology. 2013 Dec 3;81(23):2002-8.
18. Miskin C, Carvalho KS, Valencia I, Legido A, Khurana DS. EEG Duration: The Long and the Short of It. J Child Neurol. 2015 Nov;30(13):1767-9.