Abstract
Background: Tilt-table testing is safe and low-risk, but asystole of variable duration may be tilt-induced and, it was suggested that it could represent a life-threatening manifestation of vasovagal syncope. We performed a retrospective observational study evaluating the clinical characteristics and long-term outcome in patients with asystole during tilt-induced syncope.
Methods: A cohort of 552 patients referred for evaluation of recurrent syncope of unknown etiology underwent to a modified passive and active protocol tilt-table testing.
Results: 68% were positive to neurally mediated reflex syncope with 41 (11%) cases of asystole. Twenty-eight women (68%), mean age 26 ± 13 years and thirteen men, 31 ± 7 years had syncope with asystolic pause = 3 seconds during baseline, 27 of 41 (66%) or pharmacological challenge test, 14 of 41 (34%). The mean duration of asystole was 12.6 ± 11.3 seconds and, 80% of cases had sinus arrest = 5 seconds. 32 of 41 (78%) patients were successfully followed-up during a mean of 5.3 ± 1.5 years (range 1.5 to 8); 87.5% of patients had = 5 years of follow-up. Therapy was not guided based on the results of tilt-table testing and pharmacologic therapy with ß-blockers was generally effective. During long-term follow-up, only 12.5% had syncope recurrence and in 37.5% drugs were withdrawn after a long asymptomatic period.
Conclusion: Asystole during tilt-induced syncope does not necessarily predict adverse outcomes with most patients having a benign clinical course and improving with lifestyle changes and pharmacologic therapy and even spontaneously over a long-term follow-up.
Keywords
Asystole, Vasovagal syncope, Tilt-table test, Cardioinhibitory syncope, Vasodepressor syncope, Neurocardiogenic syncope, Tilt-induced asystole
Introduction
The vasovagal (VV) syncope, a variant of neurally mediated reflex syncopal syndromes is a common clinical entity and is one of a heterogeneous group of disorders of orthostatic intolerance that can be identified during an upright tilt table (TT) test. The clinical response to this test is varied, with a majority of the patients exhibiting a mixed response (vasodepressor-cardioinhibitory) and the remainder either a vasodepressor or cardioinhibitory predominant response depending on the relative degree of hypotension and bradycardia respectively [1]. The TT testing is safe and low-risk, but different rhythms and/or conduction disorders have been reported, including asystolic periods of variable duration and rarely atrioventricular block that end spontaneously, compatible with a VV reflex; even four decades ago, it was suggested that asystole may present as a life-threatening manifestation of neurally mediated syncope [2-4]. In this study, we performed a retrospective observational study evaluating the clinical characteristics and long-term outcome in patients with asystole during tilt-induced syncope.
Methods
Patient population
We selected subjects with episodes of recurrent syncope with at least two episodes during the previous 6 months, or a single episode of syncope associated with injury. A cohort of 552 consecutive patients referred to three tertiary and secondary care hospitals underwent TT testing. All of them without structural cardiovascular disease or arrhythmic episodes potentially explaining transient loss of consciousness (TLOC), absence of neurological diseases and negative response to carotid sinus massage. Patients were followed at 4 monthly intervals in the outpatient clinic during a minimum of 3 years. Information regarding recurrences events was obtained, and when requested, a new evaluation was performed. The long-term followup was obtained in an outpatient basis or by telephone information each year.
TT test protocol
Before the test, no patient was taking vasoactive drugs. The TT testing was performed in the fasting state and at least 10 minutes of supine rest, baseline heart rate (HR) and blood pressure (BP) were measured. All patients underwent to a modified passive protocol that consisted of 70° tilting lasting up to 30 minutes with continuous ECG trace and BP measurement using an automatic cuff baumanometer every 1 minute or more frequently in presence of premonitory symptoms, in these cases, patients were rapidly positioned in supine or Trendelenburg position. In the event of a negative passive TT testing and 10 minutes of supine rest the pharmacological challenge was made using protocols with intravenous infusion of isoproterenol (1 to 5 μg/min) or 1.25 mg of isosorbide dinitrate via sublingual tablets or spray, this active TT testing was programmed to 15 minutes or until syncope, whichever occurred first [5-7]. All patients gave written informed consent.
Definitions
In either passive or active TT testing, it was considered positive if a vasovagal response occurred with syncope defined as a transient state of unconsciousness characterized by spontaneous recovery or during the return to supine position. The vasovagal syncope international study (VASIS) classifies a variety of responses induced during TT testing, including cardioinhibitory responses: 2A type syncope with bradycardia <40 bpm for more than 10 seconds (s), or non-significant asystolic pause (<3s) and 2B type with significant asystolic pause (>3s) [1,8].
Statistical analysis
Data are expressed as mean ± 1 standard deviation. Statistical analysis is described as paired and unpaired twotailed Student’s t-test. A p value of ≤ 0.05 was considered significant.
Results
General clinical data
552 patients referred for evaluation of recurrent syncope of unknown etiology underwent TT testing. The patients had a mean time of historical syncope of 12.6 ± 6.6 months (range 6 to 24) with 4.2 ± 3.2 (range 1 to 12) syncope episodes in the six months preceding the TT testing vs their median lifetime syncope frequency (2 faints/year, p<0.01). 38 of 41 (92.7%) had syncope while standing, 39 of 41 (95%) had prodromal symptoms and 2 of 41 patients (4.9%) had previous history of trauma during spontaneous syncope and in any case, there was no clinical suspicion of asystole during spontaneous syncope (evaluated by suggestive clinical picture of Stokes-Adams crisis). 375 of 552 (68%) were TT testing positive to neurally mediated reflex syncope with 41 of 375 (11%) cases of asystole (7.4% of all tests) (Table 1).
| Total | TT-induced asystole | p | |
|---|---|---|---|
| Patients | 552 | 41 (7.4%) | |
| Women | 68% | ||
| Mean age (years) | 28.5 ± 10 | 26 ± 13 women 31 ± 7 men |
NS |
| History of syncope (months) | 12.6 ± 6.6 | 12.7 ± 7.1 | NS |
| Prodromal symptoms | 96.3 % | 95 % | NS |
| Injury during spontaneous syncope | 5.1 % | 4.9 % | NS |
| Number of syncopal episodes (before TT test) | 2.1 ± 0.5 | 4.2 ± 3.2 | < 0.01 |
| TT positive for VV syncope | 68% | 11% | |
| TT positive | 18.1 ± 7.8 | 61% vs 39% (baseline vs drug challenge) |
< 0.05 |
| Syncope time from tilting (minutes) | 10.8 ± 5.3 vs 7.1 ± 8 (baseline vs drug challenge |
< 0.05 | |
| Asystole duration (seconds) | - | 12.6 ± 11.3 | |
| Follow-up (years) | 5.3 ± 1.5 | ||
| No syncope recurrence (β-blocker therapy) | - | 87.5% | |
| Pharmacologic withdrawn (after at least 24 months) | - | 37.5% | |
| Cardiac pacing | 0 | 3 | |
| TT: Tilt-Test; VV: Vasovagal | |||
Study population
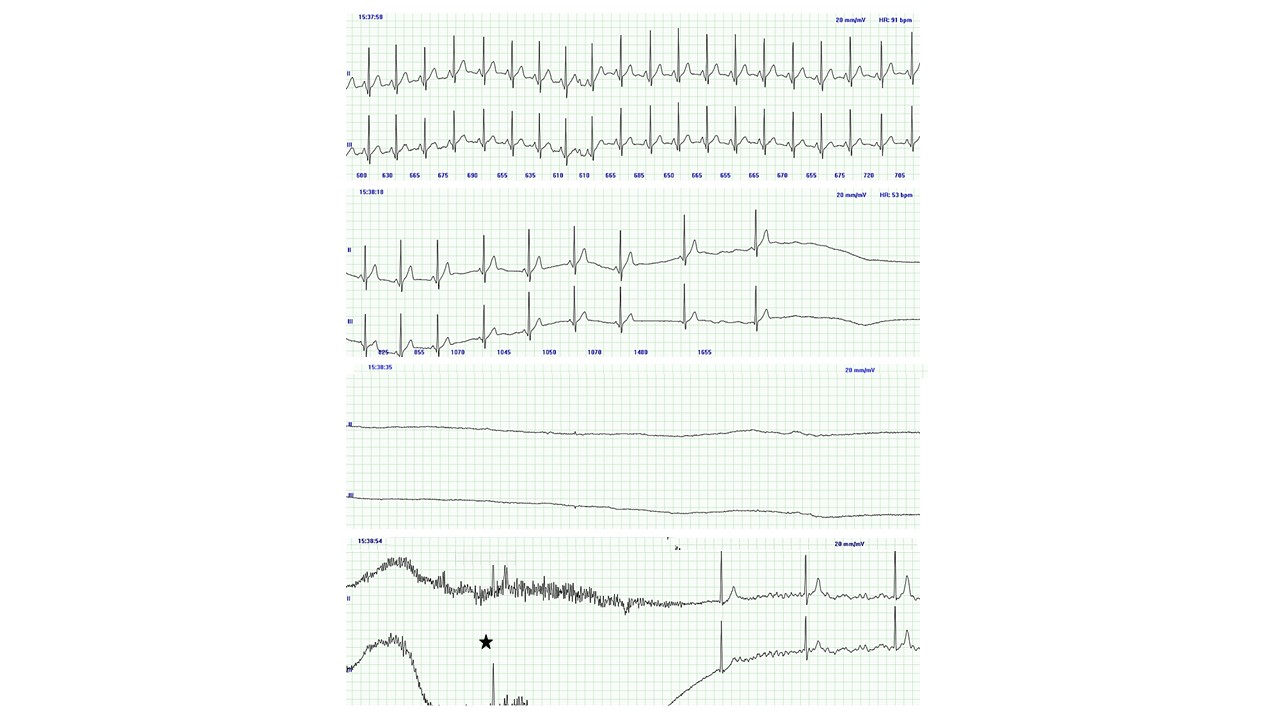
Twenty-eight women (68%) mean age 26 ± 13 years (range 14 to 54) and thirteen men, 31 ± 7 years (range 23 to 42) had syncope with 2B type cardioinhibitory response with asystolic pause ≥ 3s during baseline, 25 of 41 (61%) or pharmacological challenge test 16 of 41 (39%), (p<0.05). The mean duration of asystole was 12.6 ± 11.3s (range 3.5 to 57, median 9.8); the 80% of cases had sinus arrest ≥ 5s and 32% >10 s and an isolated case with high-grade AV block. Rapidly progressive sinus bradycardia was present in all cases that ended in sinus arrest and coincided with or was preceded by a moderate or significant vasodepressor response. The syncope episode occurred after a mean of 10.8 ± 5.3 minutes (range 1.5 to 18, median 12) of upright TT test vs 7.1 ± 8 minutes (range 3 to 19, median 4.2) during the pharmacological phase (p<0.05). The shortest time for a syncope episode during tilting was 91 s in a 17 years-old woman with secondary autonomic failure (juvenile diabetes mellitus) during passive TT testing phase with 26s of sinus arrest (Figure 1). All patients had prodromal symptoms of median duration except the patient with juvenile diabetes who had a relatively abrupt onset of syncope.
In 62% of cases, we observed a tendency to progression to asystole or asystole of longer duration that followed progressive sinus bradycardia and/or AV junctional rhythm during the time to return to the supine or Trendelenburg position (this took about <10 s). All cases of asystole ≥ 10 s had Stokes-Adams crisis and always occurred after the patients had fallen and in most with rapid recovery a few seconds after returning to the supine position. The postictal confusion state was closely correlated with the duration of the asystole.
Follow-up and treatment
32 of 41 (78%) patients with tilt-induced asystole were successfully followed-up during a mean period of 5.3 ± 1.5 years (range 1.5 to 8, median 5.2); 87.5% of patients had ≥ 5 years of follow-up. All patients were recommended to increase water and salt intake, advised to avoid triggers, and taught to recognize prodromal symptoms to perform appropriate maneuvers as soon as possible to try to abort syncope. Therapy was not guided based on the results of TT testing and all patients were initially treated empirically with β-blockers drug titration (pindolol, metoprolol, propranolol or bisoprolol) and due to failure and/or intolerance in 7 of 32 patients were indicated: the mineralocorticoid (fludrocortisone, in three), serotonin reuptake inhibitors (paroxetine, fluoxetine, in two), sympathomimetic agonist (norfenefrine, in one) and the antiarrhythmic with parasympatholytic effects (disopyramide, in one). Permanent cardiac pacing was suggested initially in the first cases of patients with the longest asystolic time (≥ 10s), but the majority refused, and only 3 of 32 patients had undergone cardiac pacing based on poor response up to three pharmacological agents used alone or in combination.
During the first years, mean follow-up duration of 2 ± 1 years no syncope was experienced by 72% of patients under continuous β-blocker therapy, mainly metoprolol (75%) or bisoprolol (20%). During the follow-up, no patient accepted a new TT testing for evaluation of the therapeutic response. β-blockers related side effects at short-term occurred in 15% that were more tolerated in the long-term with dose adjustment. Discontinuation because of intolerable side effects occurred in only 2 of 32 patients and 5 of 32 for poor clinical response. During the long-term follow-up, mean 5.3 ± 1.5 years only 12.5% of patients had at least one syncope recurrence. In 12 of 32 (37.5%) drugs were withdrawn after a minimum asymptomatic period of 24 months, with no clinical recurrence in ten and a single clinical relapse in two after 36 months. In any case, there was no clinical suspicion of asystole during spontaneous syncope.
All three patients who undergone cardiac pacing (two, dual-chamber in DDD mode) reported improve with a decrease or early disappearance of VV syncopal episodes, even though, in one case the atrial lead was dislodged, and another one patient was pacing in single-chamber VVIR mode. In the mid-term follow-up, due to few recurrences, cardiac pacing was programmed to only sensing mode and spontaneous infrequent syncope episodes were without asystole, and in all three the long-term outcome was with no recurrences.
Discussion
Although VV syncope has a good clinical evolution, little is known about the prognosis of patients who, during an upright TT testing have an asystolic response and this is associated with therapeutic challenges, which frustrate the physician and patient because is often unpredictable and sometimes unsatisfactory, notably the potential benefit of pacing therapy.
Asystole during tilt-induced syncope
Our study had an incidence of asystolic cardioinhibitory response during TT testing of 11% (7.4% of all tests) of young adults with history of recurrent syncope, similar to the previously reported incidence of 7.1% in adults.
There are differences in the incidence reported of tiltinduced asystole that may be due essentially to different populations and tilt protocols. According to reports the mean incidence occurs in 14% of patients during passive protocols and higher with pharmacological challenge test, 21% in adults and approximately 4.5% in children and adolescents with recurrent syncope [9,10].
TT testing is recognized as a valuable diagnostic tool for the identification of patients with unknown origin syncope. However, in VV syncope the outstanding problem is its clinical reproducibility; previous studies have shown that the clinical results are not always reproducible in individual patients and, it is even worse in the case of tiltinduced asystole [11,12]. According to Foglia-Manzillo G et al. [13], only 36% of patients with an initial asystolic TT testing had an asystolic response on repeat TT test, 24% still had a positive response, but without asystole and notably, 40% of patients had a negative repeat TT testing. In healthy young volunteers (25 ± 4 years) with no history of syncope undergoing TT a significant asystolic response (mean 10 s) was documented in 3 of 7 (43%) of those who had a positive TT testing, 7 of 75 (9%) [14]. Therefore, the prognostic significance cannot be based exclusively on the result of the TT testing.
One of the relevant findings from our series was that tiltinduced asystole pattern did not occur in a strictly pure form, that is, it was preceded seconds by vasodepression, or it was a mixed pattern with a very predominant cardioinhibitory response. These results are consistent with early studies that reported up to one-half of the cases the asystolic response was present with a slow simultaneous hypotension and bradycardia or preceded by significant vasodepressor component [15,16]. The hemodynamic profiles during tilting in 2B type syncope was consistent with constant BP, until 2 minutes before syncope when quickly going down to 57 ± 19% of the baseline value with decrease of vascular resistance of 76 ± 12 % at the time of syncope. HR increased to 125 ± 30% of the baseline 3 minutes before syncope, then decreased and resulted in asystole. Therefore, authors considered that in type 2B of tilt-induced syncope BP fall coincides with or occurs before the HR falls [15].
In an analysis of the temporal relationship between asystole and TLOC in tilt-induced syncope the main finding was that in 34%, asystole started after the onset of TLOC or within a short time (≤ 3s) before, then, it was very unlikely that asystole would have been the prime cause of TLOC. The median of the mean BP at the onset of asystole was higher when this occurred early than when it occurred late, ≥ 3 seconds (45.5 mmHg vs. 32.0 mmHg, respectively [16]. The fact that mean BP was higher for early than for late asystole suggests that vasodepression was less pronounced in early asystole and reasonably likely to be the prime cause of TLOC. However, BP at the onset of TLOC is likely to represent the combined effects of vasodepression and cardioinhibition and, there is no practical way to dissociate them [16]. It means that, vasodepressor component is almost invariably present to some degree, this is a relevant practical knowledge since the report of tilt-induced asystole causes medical uncertainty and questions about its prognostic significance, so, leads the clinical physician to consider cardiac pacing as firstline treatment and it is not easy to convince that this is a misleadingly consideration [16,17].
Long-term prognosis of tilt-induced asystole
Previous isolated reports associated tilt-induce asystolic response with clinically more severe symptoms and with a worst prognosis (so-called malignant VV syncope) [2,3]. The natural history of patients with VV syncope is largely unknown, particularly with regard to the clinical recurrences in the cases of tilt-induced asystole and the response to therapeutic options. However, in the last reports the long-term clinical evidence supports a different knowledge. The clinical course of this group of patients was benign overall, with no deaths and a low percentage of recurrences and, appeared to be not different from that of non-asystolic patients and even when not completely satisfactory, pharmacological treatment was generally effective to prevent asystole inducibility as well as syncopal recurrences [9,10,18-22]. During the long-term follow-up from our series only 12.5% of patients had at least one syncope recurrence and was not different from patients without asystole during the TT test; this report is one of the longest durations outcome follow-up, therefore, we can support that young adult patients with tilt-induced asystole may be safely and effectively managed with lifestyle changes and pharmacological therapy; the best clinical response was with β-blockers, which is probably explained because cardioinhibitory patients have an attenuated hemodynamic responses with higher epinephrine levels, then sympathetic predominance in their modulation of autonomic responses at syncope compared with patients with a negative TT testing and patients with vasodepressor syncope, and even, according to other reports more than a third of our series the drugs were withdrawn after an asymptomatic period [23,24].
Our patients had a long-term follow-up and with treatment not guided based on the result of the TT testing in terms of choosing cardiac pacing by prolonged asystole during tiltinduced syncope; this was in part because most patients refused, but also because at the time we agreed that there was not compelling evidence about the advantage of cardiac pacing as a first-line therapy [25,26]. Therefore, TT testing has not been proved to be a more useful tool in selecting therapy for patients with VV syncope and especially in the setting of tilt-induced asystole. It is noteworthy that, the three patients in our series who undergone cardiac pacing the indication was made based on poor response to various drugs or combinations even when there was no clinical evidence of spontaneous recurrent syncope with asystole, insistence suggestion of the referring physician and, at the time after some uncontrolled and not blinded small trials of pacemaker reported a benefit [27-29]. In these cases, we consider that a possible placebo effect was involved.
The majority of patients with prolonged asystole during TT testing respond well to lifestyle changes (increase water-salt intake, advised to avoid triggers, and recognize prodromal symptoms), physical maneuvers and/or pharmacological therapy. According to other reports, the clinical outcome of asystolic patients after TT testing appeared to be not different from that of non-asystolic patients. Therefore, there is a poor correlation between spontaneous syncope and the response pattern induced during the TT testing. To date, there are no reports that implies a worse prognosis in terms of syncope recurrence, injuries, major cardiac events, or sudden cardiac death after initial evaluation and during long term followup [18,20,22]; In the same way, even very prolonged asystole on TT testing (range ≥ 15 to 90 seconds) does not necessarily predict adverse outcome with most patients improving spontaneously over a long-term follow-up (3 to 9 years) [30,31]. Therefore, the term malignant VV syncope is not supported and should no longer be used. Efficacy of pacing in VV syncope has been discussed since several years, due to contrasting results of studies conducted so far and unclear or non-uniform patient selection criteria. According to Raviele A [21], at present, an aggressive treatment with cardiac pacing should not represent the standard therapy of tilt-induced asystole but should be reserved only for the few highly selected cases, on a single patient basis. On the other hand, it should also be noted the critical role played by the implantable loop recorder (ILR) in screening, with the ability to document the cardiac rhythm during spontaneous syncope, which would not otherwise be available. ISSUE-3 demonstrate that when spontaneous syncope is documented to be associated with asystole, cardiac pacing is beneficial. However not always abolish it, due to the associated vasodepressor component, then 25% had syncopal recurrence despite cardiac pacing therapy [32]. The benefits of a physiological pacing algorithm with contractility sensor (DDD-CLS), has been reported recently in patients with tilt-induced asystole in well-designed trials (SPAIN and Biosync) [33,34]. The most recent published Biosync trial described the effectiveness of DDD-CLS cardiac pacing in patients mean aged 63 ± 12 years with severe recurrent VV syncope and tilt-induced asystole [34].
On the other hand, there remains a knowledge gap between the proposed benefit of pacing in VV syncope and the physiological understanding of the limited effect that pacing might have, contradictory results between physiologic theory and trial evidence underlying pacing treatment at present cannot be explained and more investigation is needed to solve the dilemma [35]. According to Brignole et al. [32], it must be emphasized that the decision of cardiac pacing needs to be undertaken in the clinical context of a benign condition which frequently affects young patients, who usually have a more prolonged prodromes before TLOC.
In major studies evaluating the role of the cardiac pacing were included patients with high mean age, history of recurrent syncope beginning in middle or older age, frequent injuries probably due to lack of prodrome, and more morbidities (hypertension, diabetes) and concomitant medications, which is not the case in the vast majority of young adults.
The 2017 ACC/AHA/HRS [36] and 2018 ESC [37] guidelines recommend pacing as reasonable for patients over the age of 40 years with recurrent VV syncope and spontaneous pauses (Class IIb, LOE B-R) [36], and in patients with tilt-induced asystolic response with recurrent frequent unpredictable syncope (Class IIb, LOE B) [37], but advises against pacing in the absence of a cardioinhibitory response.
Conclusion
We conclude that TT testing is recognized as a valuable diagnostic tool for the identification of patients with unknown origin syncope, but due to its low reproducibility it is limited for selecting therapy especially in the setting of tilt-induced asystole. Tilt-induced asystole pattern did not occur in a strictly pure form, that is, it was preceded seconds by vasodepression, or it was a mixed pattern with a very predominant cardioinhibitory response.
In young adult patients with asystole during tiltinduced syncope, even when prolonged, usually does not imply a worst prognosis either for future clinical events or pharmacologic therapy, therefore, the prognostic significance cannot be based exclusively on the result of the TT. In general, the long-term follow-up the clinical outcome is benign with an acceptable response to drug treatment and most patients improving spontaneously over time. Then, according to current guidelines cardiac pacing is not the first line therapy but could be considered with its limitations only for not young high selected patients and, strictly on an individual basis.
Study Limitations
This was a retrospective study, with all its known limitations. A relatively small number of patients but, in about 80% the clinical evolution was long-term followup. We do not use finger plethysmography for noninvasive beat-to-beat BP continuous recording, but this is not strictly necessary in daily basis clinical practice. TT testing control for clinical outcome or pharmacologic therapy were not performed partly because we consider the poor reproducibility of the test. The treatment was not randomized, then precluding the analysis of the therapeutic efficacy.
Conflicts of Interest
No conflicts of interest.
Funding Statement
No grant supports.
Author Contributions
Enrique Velázquez-Rodríguez: Conceptualization, Methodology, Writing- Original draft preparation, Visualization, Investigation; María de Jesús Fernández- Muñoz: Methodology, Validation, Investigation, Resources; Marcelo Jiménez-Cruz: Methodology, Validation, Investigation, Resources.
References
2. Folino A, Buja GF, Martini B, Miorelli M, Nava A. Prolonged cardiac arrest and complete AV block during upright tilt test in young patients with syncope of unknown origin-prognostic and therapeutic implications. Eur Heart J 1992; 13(10):1416-21.
3. Maloney JD, Jaeger FJ, Fouad-Tarazi FM, Morris HH. Malignant vasovagal syncope: prolonged asystole provoked by head-up tilt. Case report and review of diagnosis, pathophysiology, and therapy. Cleve Clin J Med 1988; 55(6):542-8.
4. Milstein S, Buetikofer J, Lesser J, Goldenberg IF, Benditt DG, Gornick C, et al. Cardiac asystole: a manifestation of neurally mediated hypotension-bradycardia. J Am Coll Cardiol 1989; 14(7):1626-32.
5. Fitzpatrick AP, Theodorakis G, Vardas P, Sutton R. Methodology of head-up tilt testing in patients with unexplained syncope. J Am Coll Cardiol 1991; 17(1):125– 30.
6. Almquist A, Goldberg IF, Milstein S, Chen MY, Chen XC, Hansen R. Provocation of bradycardia and hypotension by isoproterenol and upright posture in patients with unexplained syncope. N Engl J Med 1989; 320(6):346–51.
7. Bartoletti, A, Alboni, P, Ammirati, F, Brignole M, A Del Rosso, Foglia-Manzillo G, et al. “The Italian Protocol”: a simplified head-up tilt testing potentiated with oral nitroglycerin to assess patients with unexplained syncope. Europace 2000; 2(4):339–42.
8. Brignole M, Menozzi C, Del Rosso A, Costa S, Gaggioli G, Bottoni N, et al. New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Vasovagal Syncope International Study. Europace 2000; 2(1):66–76.
9. Oslizlok P, Allen M, Griffin M, Gillette P. Clinical features and management of young patients with cardioinhibitory response during orthostatic testing. Am J Cardiol 1992; 69(16):1363-5.
10. Deal BJ, Strieper M, Scagliotti D, Hulse E, Auld D, Campbell R, et al. The medical therapy of cardioinhibitory syncope in pediatric patients. Pacing Clin Electrophysiol 1997; 20(7):1759-61.
11. Kochiadakis GE, Kanoupakis E, Rombola AT, Igoumenidis NE, Ghlouverakis GI, Vardas PE. Reproducibility of tilt table testing in patients with vasovagal syncope and its relation to variations in autonomic nervous system activity. Pacing Clin Electrophysiol 1998; 21(5):1069-76.
12. Omar AR, Ng K-S, Ng W-L, Sutandar A. Reproducibility of tilt-table test result in patients with malignant neurocardiogenic syncope. Intern Med J 2004; 34(8):504–6.
13. Foglia-Manzillo G, Romano M, Corrado G, Tagliagambe LM, Tadeo G, Spata M, et al. Reproducibility of asystole during head-up tilt testing in patients with neurally mediated syncope. Europace 2002; 4(4):365–7.
14. Dhala A, Natale A, Sra J, Deshpande S, Blanck Z, Jazayeri MR, et al. Relevance of asystole during head-up tilt testing. Am J Cardiol 1995; 75(4):251-4.
15. Nowak L, Nowak F, Jankco S, Dorwarth U, Hoffmann E, Botzenhardt F. Investigation of various types of neurocardiogenic response to head-up tilting by extended hemodynamic and neurohumoral monitoring. Pacing Clin Electrophysiol 2007; 30(5):623–30.
16. Saal DP, Thijs RD, van Zwet EW, Bootsma M, Brignole M, Benditt DG, et al. Temporal relationship of asystole to onset of transient loss of consciousness in tilt-induced reflex syncope. JACC Clin Electrophysiol 2017; 3(13):1592-98.
17. Sutton R. Asystole and Loss of Consciousness. JACC Clin Electrophysiol. 2017; 3(13):1599–600.
18. Pérez-Paredes M, Picó Aracil F, Sánchez-Villanueva JG, Florenciano-Sánchez R, Expósito-Ordóñez E,Gonzálvez-Ortega M, et al. Long-term prognosis of patients with syncope of unknown origin in prolonged asystole induced by the head-up tilt test. Rev Esp Cardiol 1997; 50(5):314-19.
19. Lacroix D, Kouakam C, Klug D, Moreau LG, Vaksmann G, Kacet S, et al. Asystolic cardiac arrest during head-up tilt test: incidence and therapeutic implications. Pacing Clin Electrophysiol 1997; 20(11):2746-54.
20. Barón-Esquivias G, Pedrote A, Cayuela A, Vale JI, Fernández JM, Arana E, et al. Long-term outcome of patients with asystole induced by head-up tilt test. Eur Heart J 2002; 23(6):483–89.
21. Raviele A. Tilt-induced asystole: a useful prognostic marker or clinically unrelevant finding? Eur Heart J 2002; 23(6):433–37.
22. Guaraldi, P, Calandra-Buonaura G, Terlizzi, R, Cecere A, Solieri L, Barletta G, et al. Tilt-induced cardioinhibitory syncope: a follow-up study in 16 patients. Clin Auton Res 2011; 22(3): 155–60.
23. Holmegard HN, Benn M, Kaijer M, Haunso S, Mehlsen J. Differences in autonomic balance in patients with cardioinhibitory and vasodepressor type of reflex syncope during head-up tilt test and active standing. Comparative study. Scand J Clin Lab Invest 2012; 72(4):265-73.
24. Vanderheyden M, Goethals M, Nellens P, Andries E, Brugada P. Different humoral responses during head-up tilt testing among patients with neurocardiogenic syncope. Am Heart J 1998; 135(1):67–73.
25. Fitzpatrick A, Theodorakis G, Ahmed R, Williams T, Sutton R. Dual chamber pacing aborts vasovagal syncope induced by head-up 60° tilt. Pacing Clin Electrophysiol 1991; 14(1):13-9.
26. Benditt DG, Petersen M, Lurie KG, Sutton R. Cardiac pacing for the prevention of recurrent vasovagal syncope. Ann Intern Med 1995; 122(3):204-9.
27. Connolly SJ, Sheldon R, Roberts RS, Gent M. The North American Vasovagal Pacemaker Study (VPS). J Am Coll Cardiol 1999; 33(1):16-20.
28. Sutton R, Brignole M, Menozzi C, Raviele A, Alboni P, Giani P, et al. Dual chamber Pacing in the treatment of neurally mediated tilt-positive cardioinhibitory syncope: pacemaker versus no therapy: a multicenter randomized study. The Vasovagal Syncope International Study (VASIS) Investigators. Circulation 2000; 102(3):294-9.
29. Connolly SJ, Sheldon R, Thorpe KE, Roberts RS, Ellenbogen KA, Wilkoff BL, et al. VPS II Investigators. Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope: Second Vasovagal Pacemaker Study (VPS II): a randomized trial. JAMA 2003; 289(17):2224-9.
30. Carvalho MS, Reis Santos K, Carmo P, Cavaco D, Parreira L, Morgado F, et al. Prognostic value of a very prolonged asystole during head-up tilt test. Pacing Clin Electrophysiol 2015; 38(8):973–79.
31. Sau A, Mereu R, Taraborrelli P, Dhutia NM, Willson K, Hayat SA, et al. Long-term follow-up of patients with prolonged asystole of greater than 15 s on head-up tilt testing. Int J Cardiol 2016; 203(1):482-5.
32. Brignole M, Menozzi C, Moya A, Andresen D, Blanc JJ, Krahn AD, et al. Pacemaker therapy in patients with neurally mediated syncope and documented asystole: Third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation 2012; 125(21):2566-71.
33. Barón-Esquivias G, Morillo CA, Moya-Mitjans A, Martínez-Alday J, Ruiz-Granell R, Lacunza-Ruiz J, et al. Dual-chamber pacing with closed loop stimulation in recurrent reflex vasovagal syncope: The SPAIN Study. J Am Coll Cardiol 2017; 70(14):1720-28.
34. Brignole M, Russo V, Arabia F, Oliveira M, Pedrote A, Aerts A, et al. Cardiac pacing in severe recurrent reflex syncope and tilt-induced asystole. Eur Heart J 2021; 42(5):508–16.
35. de Jong JSY, Jardine DL, Lenders JWM, Wieling W. Pacing in vasovagal syncope: A physiological paradox? Heart Rhythm 2020; 17(5 Pt A):813-20.
36. Shen WK, Sheldon RS, Benditt DG, Cohen MI, Forman DE, Goldberger ZD, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: Executive summary. J Am Coll Cardiol 2017; 70(5):620-63.
37. Brignole M, Moya A, de Lange FJ, Deharo J-C, Elliott PM, Fanciulli A, et al. ESC Scientific Document Group. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J 2018; 39(21):1883-1948.