Abstract
Background: Adenosquamous carcinoma is a rare colorectal carcinoma with glandular and squamous histologic components. The proximal colon is a rare site for Adenosquamous carcinoma as compared to lower gastrointestinal tract. To the best of our knowledge, only a few cases of Adenosquamous Carcinoma of the proximal colon have been reported in the literature till date, with the incidence being <0.1%.
Case Presentation: We present a case of an elderly female aged 58 years 7 months who presented with generalized pain abdomen and loss of appetite. Right hemicolectomy with Ileo-colic anastomosis was done for her. Histopathologic examination and subsequent immunohistochemistry revealed a Moderately Differentiated Adenosquamous Carcinoma of the Ascending Colon.
Conclusion: Adenosquamous carcinoma of the colon are rare and have a worse prognosis than conventional adenocarcinoma. Early detection and radical surgical excision are important and adjuvant therapy can be considered, for better survival of the patient
Keywords
Adenosquamous carcinoma, Proximal colon, Hemicolectomy
Introduction
Colorectal carcinoma is one of the most malignant solid tumors in Western countries. With the exception of the lower rectum, most primary malignant colorectal tumors are adenocarcinomas.
The frequency of adenosquamous carcinoma of the colon is <0.1% [1-3]. The first case of colorectal adenosquamous carcinoma was reported by Herxheimer in 1907 and was described as a tumor with both adenocarcinoma and squamous cell carcinoma components. These tumors have a greater potential to metastasize as compared to conventional adenocarcinoma of the colon. Adenosquamous carcinoma, located in the ascending colon is rare and has a poor prognosis. Thus, early detection of adenosquamous carcinoma is important and treatment of choice is surgical resection followed by adjuvant chemotherapy.
An adenosquamous carcinoma in the lower gastrointestinal tract is a rare malignancy with a frequency of 0.02- 0.06% [4].
Adenosquamous carcinomas are more common in the pancreatico-biliary system, but have rare presentation in lower gastrointestinal tract.
The histogenesis of adenosquamous carcinoma is described by various theories which includes the presence of embryologic nests of ectodermal cells, squamous metaplasia of the intestinal mucosa or the presence of pluripotent stem cells of endodermal origin capable of multidirectional differentiation [5,6]. Clinical manifestations are similar to those of patients with colorectal adenocarcinoma, but the diagnosis is based on histologic findings and further evaluated with the aid of immunohistochemistry.
Here we report a case of adenosquamous carcinoma in a 58 year and 7 months old female who was diagnosed as carcinoma in a colonoscopic screening procedure. The diagnosis of adenosquamous carcinoma is totally based upon histology and immunohistochemistry.
Case Presentation
We present a case of a 58 year 7 months old female, who was a known case of carcinoma colon. She came to our hospital with complaints of generalized abdominal pain and loss of appetite. She is a housewife by occupation. Her vitals were stable at the time of presentation.
Her hemoglobin and CEA levels were 12.8 gm/dl and 4.6 ng/ml respectively. Other lab parameters were unremarkable.
An emergency laparotomy revealed a growth in the ascending colon with intussusception reaching up to the hepatic flexure. Multiple enlarged lymph nodes along the ileocolic, right colic and middle colic vessels were seen. Adhesions between the colon, omentum and gall bladder were present. No omental, or peritoneal and pelvic metastasis were seen. No free fluid seen. Liver appeared grossly normal.
Under general anesthesia, a Right Hemicolectomy with Ileocolic anastomosis was performed.
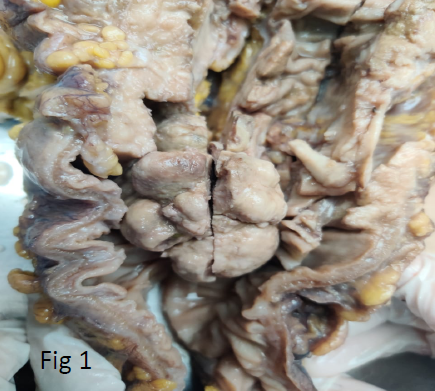
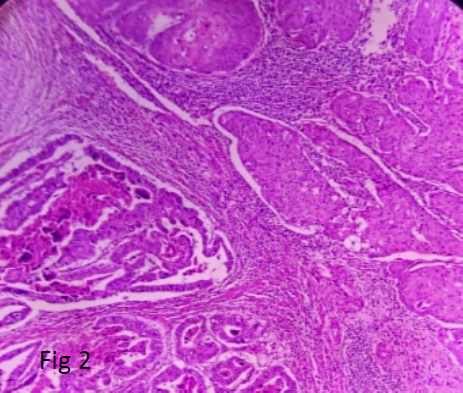
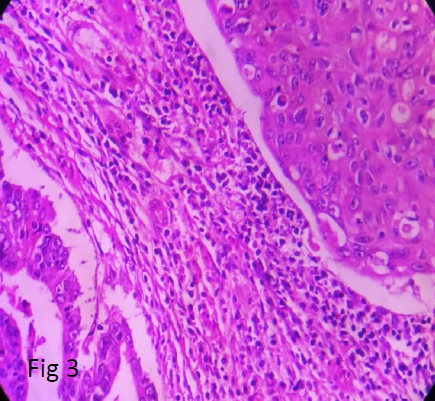
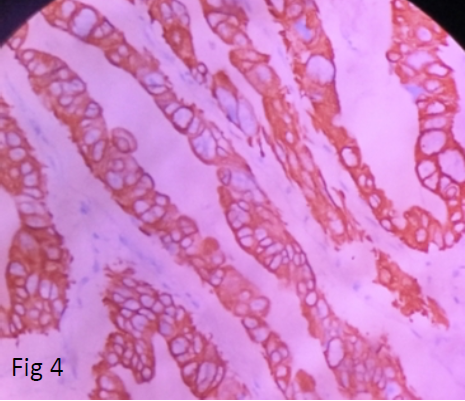
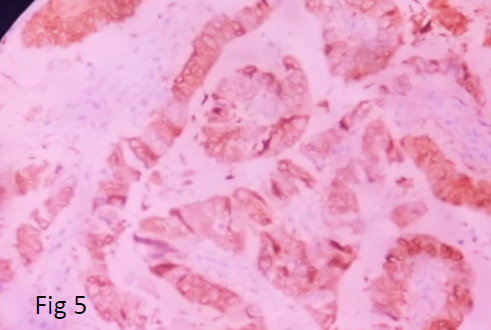
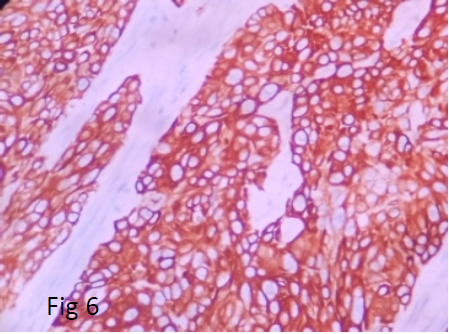
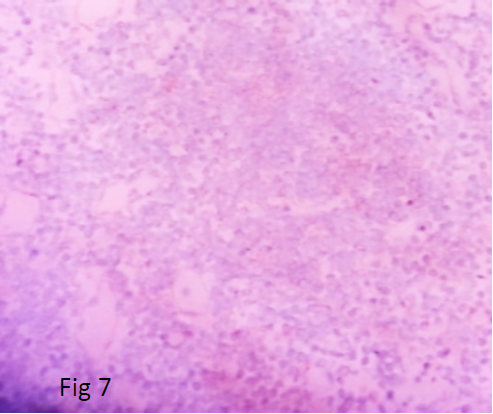
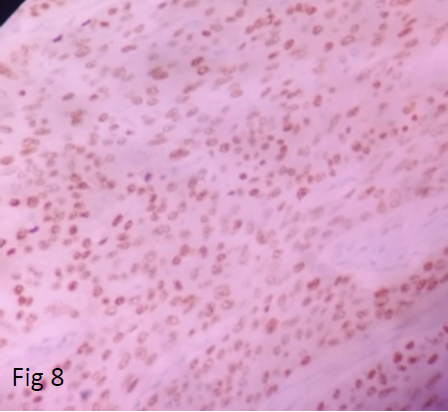
The resected specimen measured 34 cm in length. A circumferential polypoidal mass was seen in the ascending colon measuring 9.1x6.5x5.6 cm (Figure 1). The histopathologic examination of the tumor showed a biphasic morphology with a malignant glandular component and solid sheets of malignant squamous cells with keratinization (Figures 2 and 3). The tumor was seen permeating the muscularis propria into the pericolic soft tissue. The histologic grade was moderately differentiated. The resected small intestine and appendix were negative for malignancy. Lymph nodes dissected were uninvolved. The TNM staging as per AJCC 8th Edition was pT3N0 and DUKE STAGE B. On immunohistochemistry, the squamous component revealed positivity for CK5/6, p-40 and p-63 while the glandular component was positive for CK20, CDX-2 and SATB2. (Refer Table 1) (Figures 4-8).
Figure 1. Gross photograph of growth in the ascending colon.
Figure 2. Microphotograph showing biphasic elements – glandular and squamous component (H & E – 100x).
Figure 3. Microphotograph showing biphasic elements – glandular and squamous component (H & E – 400X).
Figure 4. Immuno reactive score 2+ in neoplastic cells (Non immuno reactive in squamous element) (IHC STAIN CK20, 400X).
Figure 5. Immuno reactive score 3+ in neoplastic cells (Non immuno reactive in squamous element) (IHC STAIN CDX2, 400X).
Figure 6. Immuno reactive score 2+ in neoplastic cells (Mainly in squamous element) (IHC STAIN CK5/6, 400X).
Figure 7. Immuno reactive score 2+ in neoplastic cells (Only in squamous element) (IHC STAIN P40, 400X).
Figure 8. Immuno reactive score 2+ in neoplastic cells (Mainly in squamous element) (IHC STAIN P63, 400X).
| Antibody | [Clone] - | Interpretation |
|---|---|---|
| CK-7- | [OVTL] - | Non-Immuno reactive score ‘0’ in neoplastic cells |
| CK-20 - | [SP33] - | Immuno reactive score 2+ in neoplastic cells (Non immuno reactive in squamous element) |
| CDX-2- | [EP25] - | Immuno reactive score 3+ in neoplastic cells (Non immuno reactive in squamous element) |
| CK5/6 - | [EPR1600Y] - | Immuno reactive score 2+ in neoplastic cells (Mainly in squamous element) |
| p40 – | [ZR-8] - | Immuno reactive score 2+ in neoplastic cells (Only in squamous element) |
| p63 - | [4A4] - | Immuno reactive score 2+ in neoplastic cells (Mainly in squamous element) |
| SATB 2- | [EP281] - | Immuno reactive score 3+ in neoplastic cells (Non immuno reactive in squamous element) |
The patient had an uneventful postoperative recovery and was started on adjuvant chemotherapy.
Discussion
An adenosquamous carcinoma in the lower gastrointestinal tract is a rare malignancy.In 1996, Petrelle et al. [3] described 5 males and 2 females diagnosed as having adenosquamous carcinoma. 5 of them were located in the rectum and 3 had ulcerative colitis.
In 1999, Cagir et al. [1] reported 145 cases of adenosquamous carcinoma, out of which 53% cases were located in sigmoid colon, rectum and anus and only 28% in right colon (caecum and ascending colon) and rest in the middle segment.
Frizelie et al. [5] reported different results about the location. In the report on 44 patients with adenosquamous and squamous carcinomas in the colon proximal to 8 cm from the dentate line, right sided lesions were not common (43%) and were more prone to metastasize especially to the liver, peritoneum and lung.
The histogenesis of adenosquamous carcinoma is described by various theories which includes the presence of embryologic nests of ectodermal cells, squamous metaplasia of the intestinal mucosa or the presence of pluripotent stem cells of endodermal origin capable of multidirectional differentiation [6,7]. Clinical manifestations are similar to those of patients with colorectal adenocarcinoma, but the diagnosis is based on histologic findings and further evaluated with the aid of immunohistochemistry [8].
Cagir et al. reported a mean patient survival of 12 months and an overall survival of 30.7%. Patients with distal segment lesions have a longer survival as compared to those with proximal and middle segment lesions.
Features predicting poor prognosis include right sided lesion, ulcerated or annular carcinomas, node positive disease, Grade 3 or Grade 4 cancer and stage IV disease.
In our case, it was a right sided lesion with an annular presentation. Prognosis is worse as compared to conventional adenocarcinoma.
Treatment is only surgical resection of the tumor, followed by adjuvant chemotherapy. The role modality is not known exactly, because of the rarity of the tumor.
Conclusion
Adenosquamous carcinoma of the colon are rare and have a worse prognosis than conventional adenocarcinoma. Early detection and radical surgical excision are important and adjuvant therapy can be considered, for better survival of the patient.
Ethics Approval and Consent to Participate
Written consent has been obtained from the patient.
Consent for Publication
Written consent is obtained.
Availability of Data and Material
Dharamshila Narayana Superspeciality Hospital, New Delhi.
Competing Interests
No conflict of interest.
Authors' Contributions
| CONCEPT OF STUDY | P, HMA |
| DEFINITION OF INTELLECTUAL CONTENT | P, HMA |
| LITERATURE SEARCH | P, HMA |
| CLINICAL/EXPERIMENTAL STUDIES | P, HMA |
| DATA ACQUISITION | P, HMA |
| DATA ANALYSIS | P, HMA |
| MANUSCRIPT PREPARATION | P, HMA |
| MANUSCRIPT EDITING | HMA, P |
| MANUSCRIPT REVIEW | HMA, P |
Acknowledgements
I would like to acknowledge the entire technical staff and my dear colleagues of the Department of pathology, Dharamshila Narayana Superspeciality Hospital, New Delhi.
References
2. Masoomi H, Ziogas A, Lin B, Barleben A, Mills S, Stamos MJ, et al. Population-based evaluation of adenosquamous carcinoma of the colon and rectum. Diseases of the Colon and Rectum. 2012 May;55(5):509-14.
3. Petrelli NJ, Valle AA, Weber TK, Rodriguez-Bigas M. Adenosquamous carcinoma of the colon and rectum. Diseases of the Colon and Rectum. 1996 Nov;39(11):1265-8.
4. Herxheimer G. Ober heterologue cancroide. Beitr Pathol Anat. 1907;41: 348–412.
5. Frizelle FA, Hobday KS, Batts KP, Nelson H. Adenosquamous and squamous carcinoma of the colon and upper rectum. Diseases of the Colon and Rectum. 2001 Mar 1;44(3):341-6.
6. Kontozoglou TE, Moyana TN. Adenosquamous carcinoma of the colon—An immunocytochemical and ultrastructural study. Diseases of the Colon and Rectum. 1989 Aug;32(8):716-21.
7. Cerezo L, Alvarez M, Edwards O, Price G. Adenosquamous carcinoma of the colon. Diseases of the Colon and Rectum. 1985 Aug 1;28(8):597-603.
8. Juturi JV, Francis B, Koontz PW, Wilkes JD. Squamous-cell carcinoma of the colon responsive to combination chemotherapy. Diseases of the Colon and Rectum. 1999 Jan;42(1):102-9.