Commentary
Transpedicular screw placement techniques are technically plaintiffs have relied on navigation intraoperative which is limited by its high cost, limited use of a fluoroscope with the radiological overexposure of the personnel of health and patient offers limited help when placing screws, and vertebral anatomical modifications especially in patients with degenerative pathology result an index of placement-related complications suboptimal of the screws [1,2].
Since its introduction by Roy-Camille [3] and Louis [4] in the seventies, the use of screws pedicle has increased markedly to the present day. The causes of its success compared to non-instrumented arthrodesis, based on better consolidation percentages of vertebral fusions in the lumbosacral spine [5,6], especially in patients with lysis and a more comfortable postoperative period for the patient. Regarding complications, neurological are the most serious of complications Common and their incidence varies between authors and especially decreases with the experience of surgeon. These types of complications occur due to invasion of the canal by inserting a screw excessively medial, inferior or lateral and are associated occasionally to dural ruptures.
Lumbar roots only occupy the upper third and anterior of the foramen, so the most dangerous for pedicle rupture is the lower cortex and medial. The medial location can provoke a dural rupture and nerve root injury that comes out immediately below the pedicle instrumented. Bottom location can catch the root in its elbow at the bottom of the pedicle, in the foramen. The lateral location can injure the root of the upper level to the pedicle instrumented, like a herniated disc extraforaminal. The cephalic location of the screw in the vertebral body can cause rape the disc space of a non-fused segment and have the potential risk of accelerating the disc degeneration. In front of the vertebral body, in the lumbar area, we find vital structures such as the aorta and vena cava, and in the sacral area the autonomous plexuses responsible for the correct sexual function, internal iliac veins and L5 roots in front of lateral body area vertebral of S1 [7,8], so a screw that protrude excessively past the body vertebral could damage the aforementioned structures.
According to Roy-Camille [9] there is a security space 2 mm epidural adjacent to the pedicle and according to Gertzbein and Robbins [10] 2 mm more subarachnoid safety before damaging the root or the marrow, therefore there are four millimeters theoretically “allowed” channel entry before root or spinal damage.
Another problem added to the screw outlet of the pedicle is the loss of grip of that screw with the biomechanical commitment that it entails.
For George [11] a screw that drills or breaks the pedicle loses 11% of grip strength being able to compromise the stability of the fixation vertebral.
Pedicle instrumentation, was approved by the FDA in 1976 to treat cases of spondylolisthesis grade III and IV. Later in 1998, the FDA approved their use as systems class II that could be used in cases of Use of transpedicular screws in the treatment of spinal instability isthmic and degenerative spondylolisthesis, fractures and dislocations, spinal deformities, spinal tumors and treatment of pseudoarthrosis by previous fusion. Until at that time its use was limited to the dorsal, lumbar spine and sacral; its use in the cervical spine was contraindicated, in infectious processes, congenital malformations and others.
With the advent of better systems with greater versatility advances are now aimed at improving techniques placement of these implants trying to reduce trans and postoperative complications.
The purpose of the system is to immobilize and stabilize the spinal mobile segments as a complement to the posterolateral or interbody fusion spinal fusion. This technique offers a number of clinical and biomechanical benefits, mainly exploiting the cylindrical anatomy of the pedicle which gives it greater bone anchorage and therefore greater strength and rigidity within the vertebra. From their beginnings to the present day, these systems have changed their structural shape and the material they are made, making them simpler to fit, versatile, more resistant, compatible with imaging studies and with less chance of rejection.
Previously they were made bone fusion without instrumentation that forced the patient to stay in bed until a good development callus bone or to wear a corset for 3-6 months. Though there were instrumentation type sublaminar wiring with Luque rods and hooks, with the limitation of that more healthy segments had to be fused, the material is steel and in many cases it couldn’t properly reduce injuries.
The fixation provided by this system is quite rigid and has very effective control over mobility spinal success rates based on fusion quality and restoring the morphology of the spine show superiority and fluctuate depending on the pathology between 90-95% for degenerative pathology.
In cases of fracture, there is a 99% success in merger rates which corresponds to the results that were obtained where the 23 cases (100%) traumatic are well fused radiologically and clinically. In cases of tumor pathology, the objective fixation is pain control that is achieved in 87% of cases and neurological preservation achieving that 47% of cases have some degree of recovery.
The system involves the three columns of Dennis, the support given by the previous column is fine important to decrease the risk of failure as it shares loads and mechanical stress is minimized on the screw that can cause it to break. The loads it resists are of a translational and torsional type.
Prior to the placement of any instrumentation system, it is necessary to have radiological studies and imaging that allow us to assess the degree of instability, angulation, compromised spinal canal and the diameter of the pedicles. It is important for the surgeon to know very well the surgical anatomy of pedicle and its relationship to the dural sac and roots nervous. This is much more important when working in the dorsal and cervical region due to the amount of structures that are at risk and the smaller size of pedicles.
Contraindications relative to the use of screws transpedicular are very few and almost limited to quality of the bone where the screw is to be inserted, as well because osteopenics and osteoporotics could be a contraindication although in mild cases this can be corrected with the application of polymethylmethacrylate on screw holes to increase screw fixation within the bone.
The learning curve to assimilate a certain practice implies that the systematic repetition of a new task leads to improve the skill to perform it.
This optimization in the performance of the activity is very noticeable during the early stages, reaching then a steady state known as a plateau [12]. Gonzalvo et al. described that the asymptote for the placement of thoracic pedicle screws number percutaneous in an inexperienced spinal surgeon is found close to 180 screws (approximately 45 cases) [13].
Minimally screw insertion techniques invasive theoretically present a learning curve technically more demanding, long and difficult in compared to conventional open technique [14].
We know that there are currently 3 techniques for the placement of transpedicular screws: free hand; Fluroscopy and Systems by navigation.
The Free Hand is the placement of screws through anatomical knowledge; it is the first to be used in the 1960s; it is the one with the lowest percentage of wellplaced screws, but it does not present the risk associated with fluoroscopy.
Fluoroscopy (Figure 1) is a technique that uses anatomical knowledge and the help of 2-dimensional images and therefore with errors less than free hand but that in some series consulted is close to 8-10% of incorrectly positioned screws.
Within the Fluoroscopy technique there are 2 possibilities; Perform it with the Standard technique (which with experience the use of the fluoroscope can be minimized up to a single shot per intervention) and the Minimally invasive technique (in which for a single level of surgery no less than 10-14 shots will be necessary in the hands of surgeons with experience).
Annual exposure to 5 REM (5,000 milliREM) is currently allowed.
A 1-level MIS type intervention offers an exposure between 10 and 40 mREM.
Radiation exposure can be decreased if the ray emitter is under the table. Devices with memory are used (since the firing time is reduced by 24 “against 59” and it is also complemented by: Leaded apron. Thyroid protection. Protective glasses <90%. Anti-radiation glove <40%).
And lastly the navigation systems, among them one of the best known is the o-arm (Figure 2) that converts 2D images into 3D: allowing a higher rate of well positioned screws close to 100% (99.7% in the best series) but it has as a counterpart the cost of the system and the radiation; although this is 50% lower than that presented in the fluoroscopy technique.
We discovered that placing between 120 and 200 pedicle screws provides a degree of precision necessary to perform it with minimum safety (equivalent to carrying out a total of about 50 patients).
The fluoroscopic guide with two image intensifiers simplifies screw insertion and makes it faster because it shows the three-dimensional trajectory of the needle entering the pedicle in real time, of all modes this technique has not significantly improved accuracy when placing percutaneous screws and requires increased use of ionizing radiation.
Any invasion of the canal has been described lumbar less than 4 mm can be tolerated without causing neurological symptoms due to the existence of a safety zone of approximately that measure mainly formed by epidural fat and subarachnoid space, there are still countless reports of misplaced transpedicular screws associated with nerve root, medullary lesions, vascular, visceral, biomechanical changes in the instrumentation and decrease in merger rates [15].
The main disadvantage of placing pedicle screws with 2D fluoroscopy, is the great exposure of the patient and radiation surgical staff, we cannulate mirror pedicles of the same vertebra simultaneously, which decreases the number of control image acquisition.
The learning curve for pedicle screws placement requires time and patience since the surgeon must perform surgical maneuvers without direct vision and with minimal touch input provided through Jamshidi needle.
We believe that the comparison mirroring is probably the best way to assess training between 2 surgeons with a similar grade of training, this is because when operating at the same patient, the anatomy of the pedicles is practically the same and therefore face the same difficulty for Screw placement in vertebrae without deformities on the coronal plane. Compare results with a accuracy percentage taken as “gold standard” starting from a metaanalysis does, in our opinion, more reliable monitoring of the training and timing in which they reach the degree of sufficiency to be able to perform the surgical act with a minimum security.
The possibility of a wrong transpedicular screw placed generate a complication that depends on the anatomical characteristics of the patient, the segment compromised, vertebral and especially of the magnitude of its wrong trajectory. We consider that screws with a wall breach pedicular equal to or greater than 2 mm is more likely generate intra or postoperative adverse events (Figure 3, Table 1).
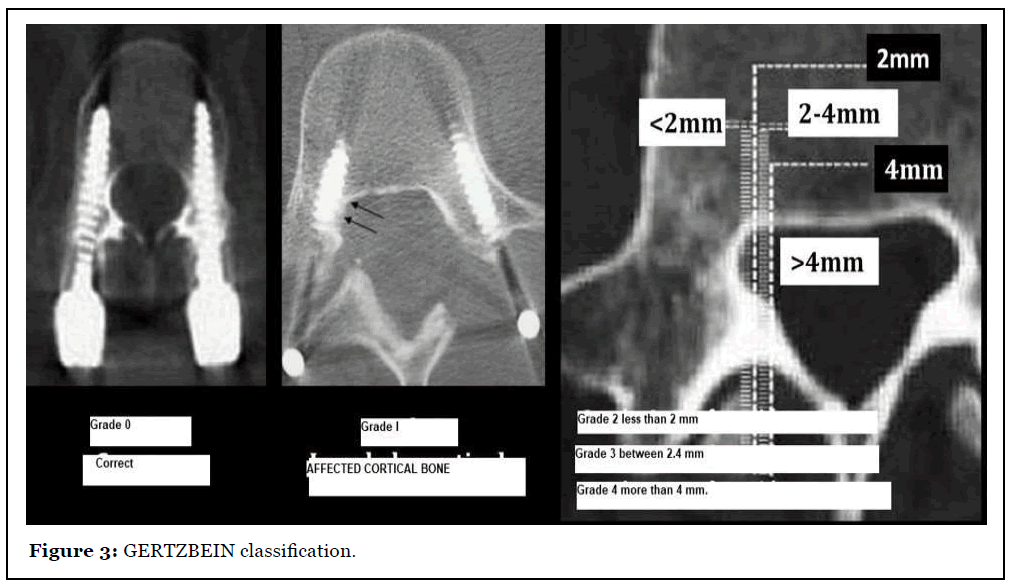
| Grade | Drilling distance |
|---|---|
| 0 | Screw completely housed inside the pedicle |
| 1 | Screw invades but does not pierce the cortex |
| 2 | Perforation <2 mm |
| 3 | Perforation 2-4 mm |
| 4 | Drilling >4 mm |
Table 1: GERTZBEIN classification.
The accuracy of screw placement can be optimized if navigation or guide techniques use intraoperative robotics which decrease significantly the patient’s radiant exposure and treating personnel in the operating room [16]. The disadvantage is the time necessary for the acquisition and virtual image processing and its high cost, so they are not available in most hospital centers.
Conclusion
Valid techniques: The surgeon’s experience is essential in the Results.
Free Hand
In favor: No radiation
Against: > Malposition index
Fluoroscopy
In favor: < Malposition regarding free hand technique
Against:> Radiation index.
Navigation
In favor: The lowest index of malposition and radiation.
Against: Price of navigation system and longer surgical time
It was evident that it needs to be placed approximately between 80-100 pedicle screws to achieve results in terms of intrapedicular accuracy comparable to what reported by surgeons experienced in this techniques (Standards and MIS and navigation systems).
In our opinion, it would be necessary to always start with the conventional standard technique, performing about 50-75 patients for anatomical knowledge. Subsequently perform the MIS technique (50 patients) and finally perform the technique aided by navigation (30 patients).
Anatomical knowledge is essential in this procedure to be able to perform the surgery with the highest percentage of normal positioned screws.
References
2. Hansen-Algenstaedt N, Chiu CK, Chan CY, Lee CK, Schaefer C, Kwan MK. Accuracy and safety of fluoroscopic guided percutaneous pedicle screws in thoracic and lumbosacral spine. Spine. 2015 Sep 1;40(17):E954-63.
3. Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clinical orthopaedics and Related research. 1986 Feb(203):18-33.
4. Roy-Camille R. Osteosynthesis of thoracolumbar spine fractures with metal plates screwed through the vertebral bodies. Reconstruction Surgery and Traumatology. 1976;15:2-16.
5. Amundsen G, Edwards C, Garfin S. Spondylolisthesis. In: Rothman RH, Simeone FA (eds). The Spine. Philadelphia: W B Saunders, 1992; 913-970.
6. Stauffer RN, Coventry MB. Posterolateral lumbarspine fusion: analysis of Mayo Clinic series. The Journal of Bone and Joint Surgery. 1972 Sep 1;54(6):1195-204.
7. Esses SI, Botsford DJ, Huler RJ, Rauschning W. Surgical anatomy of the sacrum. A guide for rational screw fixation. Spine. 1991 Jun;16(6 Suppl):S283-8.
8. Mirkovic S, Abitbol JJ, Steinman J, Edwards CC, Schaffler M, Massie J, Garfin SR. Anatomic consideration for sacral screw placement. Spine. 1991 Jun;16(6 Suppl):S289-94.
9. Roy-Camille R, Saillant GÉ, Mazel CH. Internal fixation of the lumbar spine with pedicle screw plating. Clinical Orthopaedics and Related Research. 1986 Feb(203):7-17.
10. Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990 Jan;15(1):11-4.
11. George DC, Krag MH, Johnson CC, Van MH, Haugh LD, Grobler LJ. Hole preparation techniques for transpedicle screws. Effect on pull-out strength from human cadaveric vertebrae. Spine. 1991 Feb;16(2):181-4.
12. Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a microsoft excel spreadsheet: stepby- step guide focusing on descriptive data analysis. BMC Research Notes. 2012 Dec;5(1):52.
13. Gonzalvo A, Fitt G, Liew S, de la Harpe D, Turner P, Ton L, Rogers MA, Wilde PH. The learning curve of pedicle screw placement: how many screws are enough?. Spine. 2009 Oct 1;34(21):E761-5.
14. Wood MJ, McMillen J. The surgical learning curve and accuracy of minimally invasive lumbar pedicle screw placement using CT based computer-assisted navigation plus continuous electromyography monitoring–a retrospective review of 627 screws in 150 patients. International journal of spine surgery. 2014 Jan 1;8.
15. Ahmad FU, Wang MY. Use of anteroposterior view fluoroscopy for targeting percutaneous pedicle screws in cases of spinal deformity with axial rotation. Journal of Neurosurgery: Spine. 2014 Nov 1;21(5):826-32.
16. Nowitzke AM. Assessment of the learning curve for lumbar microendoscopic discectomy. Neurosurgery. 2005 Apr 1;56(4):755-62.
