Abstract
Aim: To investigate the efficacy of uterocervical angle, posterior cervical angle, Bishop score and cervical length in predicting the success of labor induction in nulliparous patients during labor.
Methods: Our study was prospectively conducted on patients admitted to Etlik Hospital between November 2022 and June 2023 who opted for induction of labor. The mothers were between 18 and 40 years old, nulliparous and carrying a single live fetus with vertex between 37 and 41 weeks of gestation. 140 patients who met the criteria were examined by transvaginal sonography and digital cervical examination. The length of the cervix, the uterocervical angle and the posterior cervical angle, i.e. the angle between the uterus and the cervix, were measured by sonography and the Bishop score was determined by vaginal examination. The patients were divided into two groups, one successful and one unsuccessful vaginal delivery within 24 hours, and the outcome parameters were compared separately between the two groups. The target parameters were also compared by comparing patients separately by methods of cervical ripening with or without.
Results: Of the 140 pregnant women who participated in our study, 14 patients were excluded from the study due to a category III non-stress test (NST) and active vaginal bleeding. 61 patients delivered vaginally and 65 were delivered by cesarean section because vaginal delivery attempts were unsuccessful. There was no difference in demographic characteristics between the two groups, but weight and BMI were significantly higher in the group with unsuccessful deliveries.
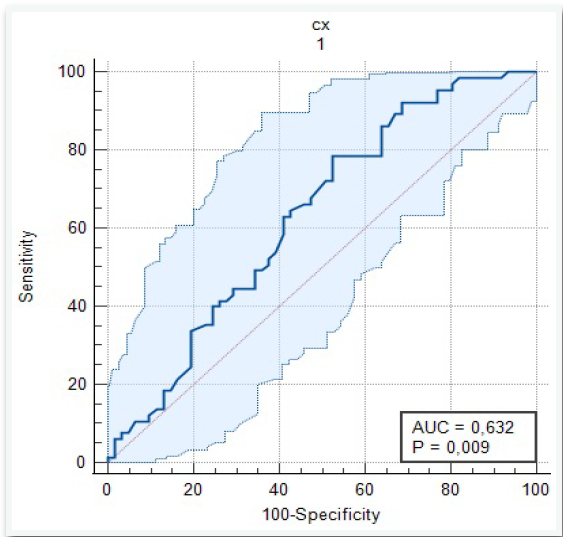
The length of the cervix was also significantly shorter in the group with successful induction (p=0.008). The cut-off value of the results of the ROC analysis curve for cervical length was 18.8 mm (AUC=0.632). While uterocervical angle (UCA) and Bishop scores were similar in both groups, vaginal delivery success was higher in patients in whom dilation and effacement were more advanced prior to induction (p=0.005). Although the posterior cervical angle (PCA) was quite high in the successful group, it was not statistically significant and predicted vaginal delivery only in the group of patients who received oxytocin and did not use cervical ripeners, it predicted vaginal delivery (p=0.022).
Conclusion: In conclusion, UCA and Bishop score measurements did not predict induction of labor at the time of delivery in the nulliparous pregnant women examined in this study. However, cervical length, posterior cervical angle, cervical dilation, and cervical effacement were found to be successful predictors of labor induction. We hypothesize that PCA and cervical length measurement are the most effective methods for predicting vaginal delivery in the group in which direct induction was induced due to various obstetric conditions and the induction was successful.
Keywords
Nulliparous, Labor induction, Posterior cervical angle, Uterocervical angle, Cervical length
Abbreviations
AUC: Area Under the Curve; CI: Confidence Interval
Introduction
Labor induction is the stimulation of uterine contractions before the spontaneous onset of labor. The goal is to achieve vaginal delivery within 24 hours. Nowadays, labor induction has become one of the most frequently performed procedures due to maternal and fetal conditions. However, it brings with it increased cesarean rates, operative vaginal deliveries, uterine hyperstimulation and variable fetal heart rate tracings. The presence of such complications makes the assessment of labor induction success important before proceeding with the induction. A Bishop score of 6 or less, obesity, nulliparity, increased birth weight, and early gestational age are associated with failed induction [1]. The Bishop score is the most commonly used cervical assessment system in clinical practice in the United States [2]. Despite its limitations, it appears to be as predictive of successful induction as fetal fibronectin or sonographic measurement of cervical length [3,4]. However, it does not inform us about changes in the internal os when the external os is closed. Additionally, it is a subjective assessment influenced by the clinician's experience. Transvaginal sonographic measurement of cervical length has been evaluated as an alternative to the Bishop score [5]. However, data from a meta-analysis of 31 studies demonstrated generally low sensitivity and specificity and limited predictivity for predicting successful induction [4]. Cervical length and the angles between the uterus and cervix, known as the posterior cervical angle and the uterocervical angle, are sonographic parameters defined for assessing the cervix. Also, popularly elastographic measurements of cervix can be seminal [6].
In our clinic, we plan labor induction at appropriate gestational weeks in light of the recommendations of professional organizations. For this reason, various subjective and ultrasonographic parameters used to predict the success of induction, particularly for evaluating the cervix, hold significant importance for us as well. Recently, the growing popularity of ultrasonographic evaluations such as the Uterocervical angle and the Posterior cervical angle has also directed our clinic to examine these parameters.
In this study, we aimed to evaluate the functions of UCA, PCA, cervical length parameters, and Bishop scoring in predicting the success of labor induction through transvaginal ultrasonography performed before the initiation of induction in patients admitted to our hospital’s delivery rooms, who were at or beyond 37 weeks of gestation and planned for vaginal delivery. Additionally, we assessed vaginal delivery within 24 hours of induction to compare the effectiveness of these parameters and determine their individual superiority.
Method
This prospective observational study was conducted at the Department of Obstetrics and Gynecology, Ankara Etlik Hospitals, between November 2022 and June 2023, on 140 term pregnancies admitted for maternal or fetal reasons, planned for labor induction.
Detailed medical histories and informed consent for the study were obtained from eligible pregnant women scheduled for labor induction upon admission. Patients included in our study were thoroughly evaluated both systemically and obstetrically before the induction was started. First, a detailed medical history was taken and recorded in the follow-up form.
The study included primigravid women aged 18-40 years with a singleton live vertex-presenting pregnancy, a Bishop score of 7 or less, and who had not yet entered the active phase of labor (cervical dilation <4 cm, effacement <60%). Patients with a history of uterine surgery, multiparous pregnancies, multiple pregnancies, malpresenting fetuses, macrosomic fetuses (pregnancies with an estimated fetal weight of 4500 grams or more), patients undergoing emergency C-section during active labor, patients with uncontrolled maternal hypertension and diabetes mellitus, pregnancies with a history of cervical surgery (LEEP, conization) and pregnancies with detected congenital fetal anomalies were excluded from the study.
To ensure standardization of the study, measurements and examinations were performed by a single physician using the same ultrasound device (Voluson S10 BT18 5788346). First, fetal biometric measurements were taken using the transabdominal probe of the ultrasound. Then, the transvaginal probe was used to measure cervical length, uterocervical angle, and posterior cervical angle, which were recorded. Vaginal examination was performed to assess cervical dilation, effacement, and Bishop score. With the patient in the lithotomy position and empty bladder, care was taken to avoid applying pressure to the cervix with the transvaginal probe. The cervix was aligned in the midline, and the endocervical canal was visualized throughout its length. During cervical measurement, care was taken to ensure that the internal os, external os, and entire endocervical canal were visible in the same image. The distance between the external os and internal os was recorded as the cervical length. With the endocervical canal, external os, and internal os linearly displayed on the screen, the angle between the endocervical canal, anterior uterine segment, and posterior uterine segment was measured using the ultrasound's “angle measurement” feature. For the measurement of the uterocervical angle, the first line of the angle was defined along the endocervical canal used for measuring cervical length, and the second line was drawn from the internal os along the anterior uterine segment for a minimum of two centimeters. The angle between these two lines was recorded as the uterocervical angle in the form (Figure 1). When measuring the posterior cervical angle, the line extending along the endocervical canal and the line with a minimum length of two centimeters drawn between the cervix and the posterior uterine segment were taken as basis and the angle between the two was recorded as the posterior cervical angle (Figure 2).
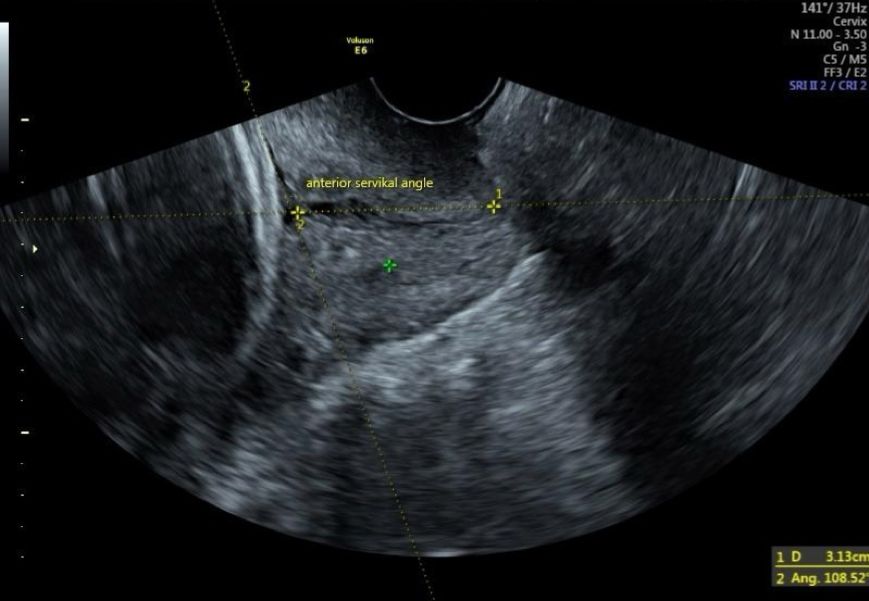
Figure 1. Uterocervical angle (UCA).

Figure 2. Posterior cervical angle (PCA).
After the measurements, the patient's age, indication for hospitalization, height, weight and body mass index, history of abortion if any, gestational week according to the last menstrual date or gestational week determined by logging according to the 1st trimester ultrasound were noted on the follow-up form.
According to the Bishop values determined after cervical evaluation of the patients, one of the cervical ripening methods (foley catheter, propess or misoprostol 25 mcg intravaginal) was frequently applied to patients with Bishop 5 and below. Induction of labor with direct oxytocin was started in patients with Bishop 5 and above. In patients whose foley balloon did not drop spontaneously, the foley was kept for a maximum of 24 hours and then withdrawn. According to the vaginal examination of the patient, oxytocin infusion was started. In patients who received Dinoprostone vaginal ovule (0.3 mg/hour prostaglandin E2 slow-release preparation for 24 hours, Propess) as the other medical cervical ripening method, the ovule was placed in the posterior fornix and the time of placement was noted on the follow-up form. If adequate contraction was not achieved, it was kept for a maximum of 24 hours and then withdrawn and continued with oxytocin infusion. Misoprostol 25 mcg majistral medicine capsules were administered vaginally every 4 hours according to the patient's cervical condition and contractions.
Oxytocin dose was given according to the alternative low dose protocol [7] by placing 1 ampoule (5000 mU oxytocin) in 500 ml, starting with 12 drops per minute, 0.5 mU in 1 drop and increasing every 15-30 minutes.
Fetal heart rate tracings were monitored throughout the labor induction process and cesarean section was planned for patients with any fetal stress or suspicion of detachment due to active vaginal bleeding and these patients were excluded from the study. In patients who failed to reach the active phase within 24 hours, by excluding the cervical ripening time, induction was considered unsuccessful and cesarean delivery was performed. In addition, patients who had cesarean section due to fetal distress and prepartum hemorrhage were excluded from the study.
Statistical analysis
After the data collection phase, all statistical analyses were analyzed using the RStudio integrated development environment for statistical computing (Affero General Public License v3; released in 2011. RStudio for Linux, version v2021.09.4+403.pro3 Ghost Orchid; September 19, 2022; Posit, PBC). Variables were analyzed using visual (histograms, probability plots) and analytical methods (Kolmogrov-Simirnov/Shapiro-Wilk's test) to determine whether they were normally distributed. Levene's test was used to assess the homogeneity of variance. Descriptive analyses were presented using mean and standard deviation for normally distributed variables. Independent sample t test was used to compare these parameters between groups. For non-normally distributed numerical data, descriptive analyses are presented using means and quartiles (Q1-Q3). Mann-Whitney U tests were used to compare these parameters between groups. Descriptive analyses for categorical variables were presented using frequencies and percentages. Associations between categorical variables were analyzed using the Chi-square test or Fisher's exact test (in cases where the assumptions of the Chi-square test were not valid due to low expected cell counts). A general 5% type-I error level was used to infer statistical significance. A P-value less than 0.05 was considered a statistically significant result.
The study was conducted with the approval of the Ethics Committee of Ankara Etlik Zübeyde Hanlm Women's Health Training and Research Hospital, with the decision number 2022/113 dated 24/08/2022. Clinical Trials number: NCT06558500.
Results
A total of 140 pregnant women were included in the study, but 14 of them were excluded from the study because of category III NST and active vaginal bleeding during active labor and emergency CS delivery. In total, 126 nulliparous pregnant women who met the inclusion criteria were evaluated. There were 61 patients in the group who delivered vaginally with successful induction of labor (Group-1) and 65 patients in the group who failed induction (Group-2).
Demographic and basic obstetric characteristics of the study groups are detailed in Table 1. They were statistically similar between the successful and unsuccessful groups. However, body mass index and weight of the patient were significantly higher in the unsuccessful labor induction group.
|
Parameters |
Successful group Vaginal delivery (Group -1) |
Failed group CS birth (Group -2) |
P value |
|
Age (years) |
24 (21-28) |
25 (23-28) |
0.091 |
|
Height (cm) |
162.6 ± 7.17 |
162.7 ± 6.58 |
0.906 |
|
Weight (kg) |
73 (65-83.5) |
80 (72-92) |
0.005 |
|
BMI |
27 (25-31) |
30 (27-34) |
0.004 |
|
Gravida |
1 (1-1) |
1 (1-1) |
0.341 |
|
Gestational week |
39 (38-40) |
40 (38-41) |
0.088 |
|
Birth weight |
3090 (2660-3410) |
3370 (3050-3675) |
0.001 |
|
Gender |
Female 39 (63.9) Male 22 (36.1) |
Female 31 (47.7) Male 34 (52.3) |
0.098 |
|
Data are expressed as mean ± SD, median and quartiles (Q1-Q3), or number (percentage) where appropriate. A p value of <0.05 indicates a significant difference. Statistically significant p-values are in bold. |
|||
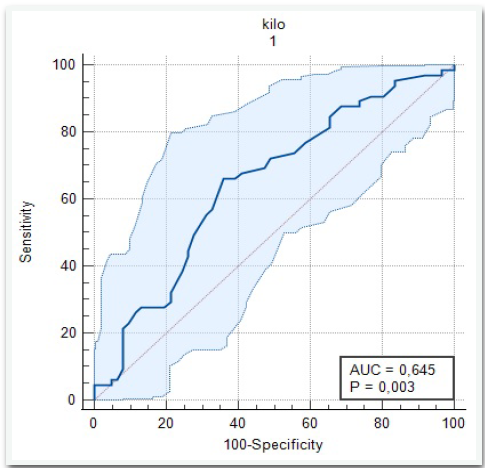
In the ROC analysis, the cut-off value for weight was 77 kg. In the regression analysis, the risk of unsuccessful vaginal delivery attempt increased 1.4-fold for every 10 kg increase (AUC=0.645, OR=1.038, sensitivity 66%, specificity 64%) (Figure 4).
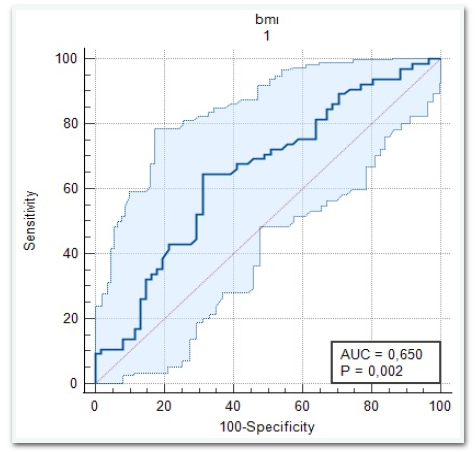
Similarly, the cut-off value determined in the ROC analysis for BMI was 29.3, and the risk of unsuccessful vaginal delivery attempt increased 1.128 times for every 1 unit increase in patients with BMI above this value (AUC=0.650, OR=1.128, sensitivity 65%, specificity 69%) (Figure 3).
Figure 3. ROC analysis of BMI.
Figure 4. ROC analysis of weight.
Unsuccessful vaginal delivery attempts increased in fetuses weighing 3260 g and above. A hundred gram increase in birth weight increased the risk of unsuccessful vaginal delivery attempt by 1.176 times (OR=1.176, p<0.001). No relationship to the gender of the baby could be determined.
According to Table 2, cervical dilatation was significantly greater in the vaginally delivered group in which induction was successful (p=0.030). The percentage of effacement was also higher (p=0.005). Cervical length was 20.8 ± 9.53 in Group-1 and 25 ± 8.17 mm in Group-2. And it was statistically significant (p=0.008).
|
Parameters |
Successful group Vaginal delivery (Group -1) |
Failed group CS birth (Group -2) |
P value |
|
Dilatation (cm) |
1.5 (0.5-2.5) |
1 (0-2) |
0.030 |
|
Effacement (%) |
30 (0-40) |
30 (0-30) |
0.005 |
|
Cervical length (mm) |
20.8 ± 9.53 |
25 ± 8.17 |
0.008 |
|
Bishop score |
4 (3-6) |
3 (2-5) |
0.146 |
|
Uterocervical angle (degrees) |
98.9 ± 29.92 |
105.8 ± 27.42 |
0.177 |
|
Posterior cervical angle (degrees) |
121.8 (103.1-138.5) |
108.9 (81.8-133.4) |
0.071 |
|
Data are expressed as mean ± SD, median and quartiles (Q1-Q3), or number (percentage) where appropriate. A p value of <0.05 indicates a significant difference. Statistically significant p-values are in bold. |
|||
In the analysis, the cut-off value for cervical length (Figure 5) was found to be 18.8 mm and below this value is associated with successful vaginal delivery (AUC=0. 632, Sensitivity= 78%, specificity= 48%). The cut-off for effacement was 30% (AUC=0.638, Sensitivity= 77%, specificity= 48%) (Table 3).
|
Variable |
AUC |
CI 95% |
p value |
Cut-off value |
Sensitivity (%) |
Specificity (%) |
|
Cervical length (mm) |
0.632 |
0.541-0.716 |
0.008 |
>18.8 |
78 |
48 |
|
Dilatation (cm) |
0.609 |
0.518-0.695 |
0.026 |
≤ 1 |
62 |
57 |
|
Effacement (%) |
0.638 |
0.548-0.722 |
0.003 |
≤ 30 |
77 |
48 |
|
Abbreviations: AUC: Area Under the Curve; CI: Confidence Interval |
||||||
Figure 5. ROC analysis of cervical length.
When the indications for hospitalization were analyzed, premature rupture of membranes was the first indication with 45 patients, followed by post-term pregnancies with 42 patients. The number of patients in groups who were presented with only rupture of membranes and post-term pregnancy were statistically sufficient to compare UCA and PCA values. Although the PCA value was found to be higher in patients who were presented with premature rupture of membranes and delivered vaginally compared to the other group, but it was not statistically significant. Similarly, in patients presenting with post-term, PCA value was significantly higher in the vaginal delivery group, but not statistically significant also. In both groups, UCA value and Bishop score did not predict successful vaginal delivery.
The number of patients in which direct induction was started due to various obstetric conditions and induction success was achieved (n=32) was sufficient for the statistical analysis, the PCA value was 126 degrees and statistically significantly higher in the group with successful vaginal delivery (p=0.037) (Table 4).
|
|
Vaginal delivery n:32 |
CS n:27 |
TOTAL n:59 |
|
|
UCA |
98 ± 31.8 |
113 ± 23.8 |
105 ± 29.1 |
0.053 |
|
PCA |
126 (109-140) |
114 (77-131) |
118 (101-134) |
0.037 |
|
Data are expressed as mean ± SD, median and quartiles (Q1-Q3), or number (percentage) where appropriate. A p value of <0.05 indicates a significant difference. Statistically significant p-values are in bold. |
||||
Oxytocin alone was the most common method with 59 patients (46.8%) in total. In the successful group, induction with oxytocin alone was again the most common method (52.5%). In the unsuccessful group, foley catheter was the most common cervical ripening method and 49.2% of the total catheterized patients had unsuccessful vaginal delivery attempts.
Of the 126 patients included in the study, 65 delivered with CS and induction was not successful. Among these indications, the diagnosis of CPD is the first with 28 patients (43.1%). This was followed by 23 patients (35.4%) with a diagnosis of non-progressing labor and 14 patients (21.5%) with a diagnosis of failed induction.
In the post hoc analysis conducted, the primary aim is to evaluate whether it is possible to predict delivery outcomes with posterior cervical angle (PCA) or uterocervical angle (UCA) in patients undergoing labor induction with oxytocin. The study, with an S pooled of 25.8 and an alpha error of 0.05, included group sizes of 32 and 27. The calculated power of the study is 77%.
Discussion
The cervix is an organ of balance consisting of collagen fibers in the extracellular matrix and takes on a different structure before pregnancy, at the beginning of pregnancy and in preparation for childbirth as a result of changes in these fibers. The traditionally used Bishop score is a standardized method used in pre-induction assessment to predict induction of labor. It is subjective, with inter-observer variability. Studies over the past 30 years to find a better predictor of labor induction have shown that ultrasonographic assessment of the cervix is a better method. Recent studies suggest that the relationship of the uterus to the cervix also influences the birth process. And the hypothesis is this: If the angle between the uterus and the cervix increases, the major vector of fetal pressure on the endocervical canal will be greater and thus the fetal thrust will increase, which, combined with the maternal thrust, will make the concomitant labor induction methods more effective, accelerate fetal descent and increase the probability of vaginal delivery within 24 hours. The first study in the literature evaluating the angle between the uterus and cervix was a seven-parameter comparative study by Paterson et al. in which patients were evaluated by TVUSG.
According to this study, the posterior cervical angle was more significant than the Bishop score in predicting vaginal delivery. The combination of a posterior cervical angle greater than 70 degrees and a Bishop score greater than 5 provided the best accuracy in predicting successful induction of labor (sensitivity = 88%, specificity = 100%) [8]. In an 80-patient cervical length and Transperineal ultrasound study, cervical length was also shown to be an essential predictor for labour induction [6]. In a study in which 200 nulliparous patients were evaluated pre-induction, posterior cervical angle, cervical length and Bishop scores were compared; while both Bishop score and posterior cervical angle did not predict labor induction, cervical length was highly successful in predicting labor induction success (P < 0.001) [9]. Dasari et al. in which TVUSG parameters were evaluated against the Bishop score, >110° posterior cervical angle and <2 cm cervical length are the best predictors for the success of labor induction [10]. In a study conducted by Keepanasseril et al. with nulliparous pregnant women, sensitivity was calculated as 65% and specificity as 72% when the posterior cervix angle was taken as 100 Z [11]. Al-Adwy et al. evaluated 49 successful induction and 21 unsuccessful induction groups and compared PCA, cervical length and Bishop score and found that a PCA of more than 99.5° was the most predictive parameter for successful induction. In this study, the recommended limits for prediction of successful labor induction were PCA more than 99.5°, cervical length less than 34 mm and Bishop score more than five [12]. In a prospective study conducted by Göktürk et al. on 178 pregnant women at term, they concluded that multiparity status, cervical length, posterior cervical angle and Bishop score were predictive of successful labor induction. Cervical length was statistically significantly shorter in the successful group (23.1 ± 7.42 mm vs. 31.3 ± 6.83 mm, p<0.001). The Bishop score was statistically significantly higher (3 (1-4) vs. 1 (1-4), respectively, p < 0.001). Posterior cervical angle was also significantly higher (100.1 ± 17.2, 92.7 ± 21.4, p=0.007, respectively) [13].
Eun Ju Kim et al. in a retrospective study conducted in 2021 with 90 pregnant women, cervical length was significantly shorter in the vaginal delivery group and PCA was significantly wider in the vaginal delivery group. PCA greater than 96.5 degrees was found to be an independent factor associated with successful vaginal delivery [14]. Many factors may increase or decrease the success of labor induction, when the literature is reviewed. Favorable factors include multiparity, body mass index BMI<30, suitable cervix and birth weight<3500 grams [16,17]. Kominiarek et al. found that the duration of labor to reach active phase and full cervical opening in both nulliparous and multiparous women was negatively affected by high BMI [15].
The results of our study are quite similar to the studies on posterior cervical angle and cervical length measurements in the literature. And in this respect, our study also supports literature. Another strength of the study was the exclusion of pregnant women with fetal anomalies and USG estimated fetal weight of 4500 grams or more. However, the heterogeneity of our diagnoses; some indications are of maternal origin, some indications were due to obstetric reasons. We do not know how the fact that half of the sample had a history of amnion retention affected our study.
Interestingly, the potential applications of angle measurements, such as the uterocervical or anterior cervical angle, extend beyond obstetric settings into gynecological research. For example, in a study investigating the etiopathogenesis of primary dysmenorrhea, transabdominal sonographic evaluation of 200 virginal patients revealed that the anterior cervical angle was significantly higher in the control group compared to the dysmenorrhea group [16]. This finding underscores the potential diagnostic value of cervical angle measurements in understanding and managing gynecological conditions. While our study focused on labor induction outcomes, such evidence highlights the broader applicability of angle measurements, suggesting that these parameters could serve as useful markers in both diagnostic and therapeutic contexts across obstetrics and gynecology. Future studies are warranted to explore these relationships further and validate their clinical significance.
Strengths
One notable strength of our study is the selection of a homogenous patient group, consisting exclusively of nulliparous patients at full-term pregnancy. Additionally, the use of transvaginal ultrasonography provided highly accurate and reliable measurements of these parameters, enhancing the credibility of our findings. Our study also stands out by comparing multiple diagnostic markers, including UCA, PCA, cervical length, and Bishop scoring, offering a comprehensive assessment of their predictive value in labor induction outcomes.
Another strength of our study is that all measurements and evaluations were conducted by a single physician, which significantly reduces interobserver variability and enhances the reliability and consistency of the data. This approach ensures that the methodology remains uniform throughout the study, minimizing potential biases that could arise from differences in measurement techniques. Such standardization is particularly valuable in studies involving sonographic parameters like the uterocervical angle (UCA) and posterior cervical angle (PCA), as these measurements can be operator-dependent.
Limitations
First, the sample size, although statistically sufficient for the primary objectives, may not be representative of broader populations, limiting the generalizability of the findings. Additionally, the influence of confounding factors such as BMI, maternal age, and parity, which may affect the uterocervical angle (UCA) and posterior cervical angle (PCA), was minimized but not entirely eliminated. Furthermore, while we excluded preterm and multiparous patients to limit heterogeneity, this exclusion narrows the scope of the study and may limit its applicability to other patient groups. Future prospective studies with larger and more diverse populations, as well as standardized measurement protocols, are needed to validate these findings and address these limitations.
Conclusion
The results of cervical length and posterior cervical angle measurements obtained from many studies in the literature are similar to our study, which supports the existing literature and raises awareness of objective ultrasonographic measurements. The fact that the Bishop score was not predictive in our study should perhaps lead us to more objective sonographic evaluations.
In conclusion, considering that the patient is already in the lithotomy position and cervical length will be frequently evaluated by TVUSG, which is easily available in many institutions, a posterior cervical angle parameter to be added to this will help us to predict successful induction of labor together with cervical length. It is of course important to continue to conduct studies with larger samples to evaluate all these.
Declarations
Acknowledgments
None.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The study did not receive funding.
Data statement
Data are openly available in a public repository that issues datasets with DOIs.
References
2. Bishop EH, Pelvic Scoring For Elective Induction. Obstet Gynecol. 1964;24:266.
3. Crane JM. Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol. 2006 Sep;49(3):573-84.
4. Verhoeven CJ, Opmeer BC, Oei SG, Latour V, van der Post JA, Mol BW. Transvaginal sonographic assessment of cervical length and wedging for predicting outcome of labor induction at term: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2013 Nov;42(5):500-8.
5. Feltovich H. Cervical Evaluation: From Ancient Medicine to Precision Medicine. Obstet Gynecol. 2017 Jul;130(1):51-63.
6. Li X, Li L, Li Y, Fang S, Zhao C, Zhang Y, et al. USEFULNESS OF TRANSPERINEAL VIRTUAL TOUCH QUANTIFICATION IN THE CERVIX FOR PREDICTING OUTCOME OF LABOR INDUCTION. Ultrasound Med Biol. 2020 Sep;46(9):2207-14.
7. ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol. 2009 Aug;114(2 Pt 1):386-97.
8. Paterson-Brown S, Fisk NM, Edmonds DK, Rodeck CH. Preinduction cervical assessment by Bishop's score and transvaginal ultrasound. Eur J Obstet Gynecol Reprod Biol. 1991 Jun 5;40(1):17-23.
9. Bastani P, Hamdi K, Abasalizadeh F, Pourmousa P, Ghatrehsamani F. Transvaginal ultrasonography compared with Bishop score for predicting cesarean section after induction of labor. Int J Womens Health. 2011;3:277-80.
10. Dasari P, Thiyagalingam S. Prediction of success of induction of labour: Bishop’s score versus transvaginal sonographic parameters. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2021 Mar 1;10(3):1251-9.
11. Keepanasseril A, Suri V, Bagga R, Aggarwal N. Pre-induction sonographic assessment of the cervix in the prediction of successful induction of labour in nulliparous women. Aust N Z J Obstet Gynaecol. 2007 Oct;47(5):389-93.
12. Al-Adwy AM, Sobh SM, Belal DS, Omran EF, Hassan A, Saad AH, et al. Diagnostic accuracy of posterior cervical angle and cervical length in the prediction of successful induction of labor. Int J Gynaecol Obstet. 2018 Apr;141(1):102-7.
13. Gokturk U, Cavkaytar S, Danısman N. Can measurement of cervical length, fetal head position and posterior cervical angle be an alternative method to Bishop score in the prediction of successful labor induction? J Matern Fetal Neonatal Med. 2015 Jul;28(11):1360-5.
14. Kim EJ, Heo JM, Kim HY, Ahn KH, Cho GJ, Hong SC, et al. The Value of Posterior Cervical Angle as a Predictor of Vaginal Delivery: A Preliminary Study. Diagnostics (Basel). 2021 Oct 25;11(11):1977.
15. Kominiarek MA, Zhang J, Vanveldhuisen P, Troendle J, Beaver J, Hibbard JU. Contemporary labor patterns: the impact of maternal body mass index. Am J Obstet Gynecol. 2011 Sep;205(3):244.e1-8.
16. Sahin ME, Sahin E, Madendag Y, Madendag IC, Tayyar AT, Özdemir F, et al. The Effect of Anterior Uterocervical Angle on Primary Dysmenorrhea and Disease Severity. Pain Res Manag. 2018 Sep 17;2018:9819402.