Abstract
Introduction: This study examined the role of the medial patellofemoral ligament (MPFL) and medial patellotibial ligament (MPTL) in patellar stability at various flexion angles.
Methods: Nine cadaveric knees were used. The MPFL and MPTL were isolated and marked. The knees were potted and rigidly fixed to a materials testing system (Instron, Norwood, MA). A wire was threaded through two concentric holes in the patella allowing it to translate laterally. The knees were secured in different angles of flexion (0o, 10o, 20o, 30o, 40o, 50o, and 60o). At each angle the knees were tested with both structures intact, one or the other transected, the MPFL reconstructed alone, both structures reconstructed and the MPTL reconstructed alone. A repeated measures ANOVA was conducted to examine the difference between force and strain using SPSS statistical software.
Results: The force needed to displace the patella 1 cm was significantly less at all flexion angles when the MPTL and MPFL were transected compared with intact, MPFL reconstruction, MPTL reconstruction and both reconstructed (p<0.05). With an increase in flexion the stiffness increased as well. Stiffness was significantly higher at 30°, 40°, 50° and 60° (p<0.001) for the MPFL reconstruction compared to the intact knee. When both the MPFL and the MPTL reconstructions together were compared to the intact state, the reconstructions at 40°, 50° and 60° of flexion had a significantly high stiffness p=0.025, p=0.022 and p=0.007 respectively.
Discussion: The MPFL remains the primary medial stabilizer of the patella. Our initial thoughts were that the MPTL could provide a possible alternative in reconstruction techniques for patellar instability. After our study was completed, we determined that the native MPTL provides little functional importance to preventing lateral displacement of the patella. Our reconstruction results did provide some increased benefit of reconstructing the MPTL and MPFL. This is most likely due to replacing the native ligament with a profoundly more robust ligament under tension.
Keywords
Medial patellofemoral ligament (MPFL), Medial patellotibial ligament (MPTL), Biomechanics, Reconstruction
Introduction
The medial patellofemoral ligament (MPFL) is a thickened band of tissue that originates from the adductor tubercle and inserts on the proximal medial patella. It is expected that the MPFL, under patellar lateral subluxation, will fail at approximately 12-18 mm of displacement [1] due to the failing of collagen based structures at 20% to 30% elongation [1].
The geometry of the trochlear groove, the vastus medialis, the MPFL and medial patellotibial ligament (MPTL) provide stability for the patellofemoral joint [2,3]. Studies examining patellar instability have been conducted suggesting that the MPFL provides the majority of the restraint to lateral translation of the patella [4-6]. Several studies describe the patella traveling twice as far after the MPFL was transected [4-6]. Upon severing the MPFL, it has been reported that the force needed to displace the patella decreases between 14% and 22% [7]. One study found that the MPFL provided 53% of the restraint for the patella [8]. This was found by sequentially cutting the soft tissue structures of the knee.
The medial patellotibial ligament (MPTL) is a stabilizing structure for the patella that reportedly contributes 30% of restraint for the patella at 30° of flexion [5]. The MPTL is located in a more superficial layer than the MPFL [9]. Therefore, the ligament is thinner and provides less restraint. There is a paucity of evidence about the MPTL and its contribution to medial restraint of the patella. It is unknown whether there is a specific flexion angle of the knee where the MPTL contributes more to patella stability. Hautamaa et al. found that when the MPFL and MPTL were reconstructed balance of the patella was returned to near normal range [5].
The purpose of this study was to determine the amount of medial restraint of the patella provided by the MPTL and MPFL at various flexion angles and to report the flexion angle where each structure has the greatest effect on patellar stability. We also examined the effect of reconstructing the MPFL, MPTL or both on patellar stability.
Materials and Methods
Nine cadaveric knees were used for this study (Biological Resource Center of Illinois, Rosemont, IL). The study was reported via Human Research Determination Form to the institutional review board (IRB) of the Wayne State University (IRB# 2020035) and it was documented that no IRB approval was required (de-identified specimen does not constitute human subjects research). The study was reported via Human Research Determination Form to the institutional review board (IRB) of the Wayne State University and it was documented that no IRB approval was required (de-identified specimen does not constitute human subjects research). The freshfrozen specimens were thawed at room temperature the night prior to dissection. Radiographs were taken of the specimens prior to dissection to observe the trochelar groove geometry [10]. The skin and subcutaneous tissues were removed leaving intact all other tissue. The lead author identified the MPFL and the MPTL. All specimens underwent biomechanical testing in the intact state, after sectioning of the MPFL and MPTL, with the MPFL reconstructed, with the MPTL reconstructed and with both reconstructed.
Biomechanical testing
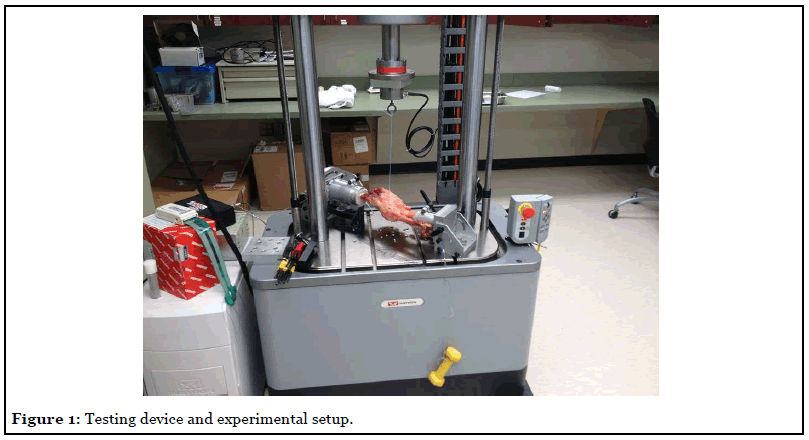
The knees were potted in aluminum cylinders using Bondo (3M, St. Paul, MN). The potted specimens were rigidly attached to the base of an electromechanical materials testing machine (ElectroPuls E10000, Instron, Norwood, MA) lateral side up. A wire was threaded through two concentric holes in the patella and attached to the actuating arm of the materials testing machine and the patella was pulled in the lateral direction (Figure 1). This test set up has been used previously [7] (Figure 1).
The knees were secured in different angles of flexion (0o, 10o, 20o, 30o, 40o, 50o, and 60o) in neutral rotation. This position was verified with a goniometer. A two-pound weight was clamped to the patellar tendon and suspended to simulate a small quadriceps-force [1,4-6,11]. This helped to centralize the patella during the study, thereby minimizing the medial patellar subluxation effects of gravity [7].
Strain of the MPFL and MPTL was measured using a 3.0 mm stroke micro-miniature DVRT linear displacement transducer (Lord Microstrain, Williston, VT). This was placed at the origin/insertion sites of MPFL and MPTL.
To determine the difference in force required to displace the patella 6 cm, a static load was applied at 100 mm/ min as previously described [7]. Force and displacement were recorded by the materials testing machine. Stiffness was calculated by taking the slope of the line in the linear portion of the force/displacement curve.
MPFL reconstruction
The superficial and deep fascia were incised superior to the patella between the quadriceps tendon and vastus medialis. The vastus medialis was elevated off the intermuscular septum and the adductor magnus tendon was identified. The intermuscular septum was severed to visually identify the adductor magnus tendon. The adductor magnus tendon was harvested and all of the muscle tissue was removed. The insertion sites were identified to determine the correct placement of the bone tunnel for the reconstruction.
Isometric graft placement was performed using a tensiometer [12]. A 1.5 cm incision was made lateral to the patella and a transverse 2.5 mm drill hole made at the junction of the superior and middle one-third sections near the anatomical insertion of the MPFL. A No. 2 Vicryl suture connected to the isometer was passed through the transverse patellar hole and around a Kirschner wire positioned at the origin of the MPFL on the medial epicondyle. The excursion of the suture through a range of knee flexion was measured on the tensiometer. The isometric location was established by adjusting the position of the Kirschner wire about the medial epicondyle until suture excursion was minimized.
The adductor magnus graft diameter was sized. After determining graft size, the appropriate diameter cannulated drill was used to make a drill hole over the Kirschner wire at the adductor tubercle. A whip-stitch was placed at the end of the graft to pass it through the bone tunnel. A drill hole matching the graft diameter was placed in the patella at the same hole where the tensiometer was used. The appropriate sized drill was advanced 10 mm—which represents the amount of graft in the patellar tunnel.
A 4.5 mm PEEK Bio-Corkscrew (Arthrex, Naples, Florida) was placed in the patellar tunnel. The graft length was determined from the bone tunnel to the medial edge of the patella. The graft was trimmed to the appropriate length. Graft fixation was performed at 30° of flexion using a sliding knot construct and knot pusher.
MPTL reconstruction
The width of the patellar tendon was measured using a standard ruler. The knee was flexed placing the patella tendon in tension; the medial 8-mm of the patella tendon was marked from the tibial tubercle to the patella. A sharp scalpel was used to incise the portion of the tendon to be used as graft. Using an oscillating saw an 8 mm by 30 mm tibial bone plug was harvested. The precise location of the graft fixation was determined by dynamic assessment with flexion and extension of the knee. Fixation point would show patellar stability near extension without causing excessive tension when the knee was flexed. Previous studies described the MPTL as originating inferiorly and medially on the patella passing distally with an oblique trajectory inserting 1.5 cm distal to the joint line [13,14].
The appropriate fixation point was marked with a beath pin. Using the Arthrex bio-tenodesis set (Arthrex, Naples, Florida), an 8-mm drill bit was used to create the bone tunnel. The tunnel was drilled to a depth of 30 mm. The bone graft was fashioned to accommodate the drilled tunnel. Bone-plug tunnels were used to place sutures across the plug allowing us to introduce the plug using the bio-tenodesis driver. The graft was place in the tunnel and fixed with a 9.0-mm bio-tenodesis screw.
Statistical analysis
Data were reported as mean ± standard error. Repeated Measures of ANOVA (PostHoc LSD) was also used to determine whether there was a significant difference in the force needed to displace the patella intact, with MPFL and MPTL resected, MPFL reconstructed, MPTL reconstructed and both the MPFL and MPTL reconstructed. Significant P value was set at being smaller than 0.05.
Results
Of the knee specimens used for testing, the average age was 52.9 ± 5.75 years, four were female and seven were male. Radiographs taken prior to mechanical testing revealed that all of the knees in the study had normal trochlear groove geometry.
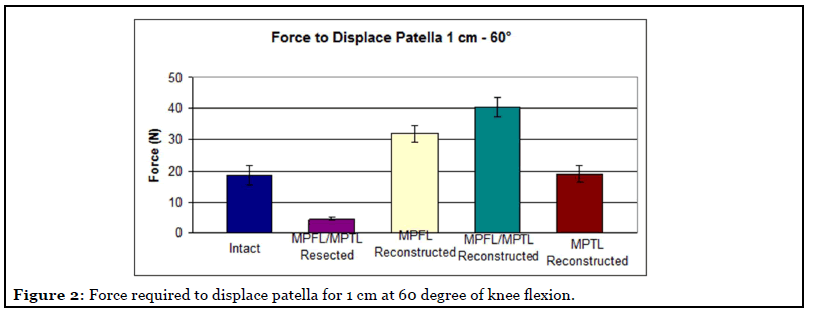
The force needed to displace the patella 1 cm was significantly less at all flexion angles when the MPTL and MPFL were transected compared with intact, MPFL reconstruction, MPTL reconstruction and both reconstructed (p<0.05). At 0° the force required to displace the patella 1 cm increased significantly between intact (16.6 ± 9.01N) and the MPFL reconstructed knee (20.1 ± 4.10 N) (p=0.047). The same result was found at 40° where the force to displace the patella of the intact knee was (21.96 ± 8.44N) and the force for the MPFL reconstructed was (28.3+/-7.56N) (p=0.037). At 50° the maximum force for the intact knee was 19.5 N and the MPFL reconstructed was 34.1 N (p=0.016). Both the MPFL and MPTL reconstructions together at 50° (34.12+/-8.88 N) and 60° (40.31+/-9.31 N) of flexion (Figure 2) had an increase in the force to displace the patella. There was no significant difference in force to displace the patella between the intact knee and the MPTL reconstructed knee.
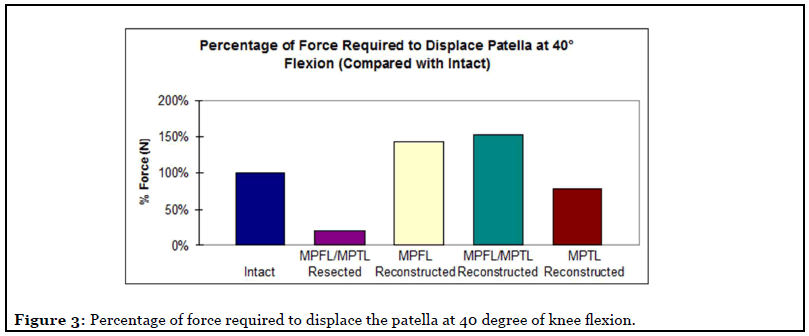
With an increase in flexion the stiffness increased as well. Stiffness was significantly higher at 30°, 40° 50° and 60° (p<0.001) for the MPFL reconstruction compared to the intact knee. When both the MPFL and the MPTL reconstructions together were compared to the intact state the reconstructions at 40°, 50° and 60° of flexion had a significantly high stiffness p=0.025, p=0.022 and p=0.007 respectively (Figure 3).
Discussion
This study demonstrated that the MPFL remains the primary medial stabilizer of the patella. Our initial thoughts were that the MPTL could provide a possible alternative in reconstruction techniques for patellar instability. After our study was completed, we found out that the native MPTL provides little functional importance to preventing lateral displacement of the patella. The secondary stabilizers all work in concert in preventing lateral patellar displacement—not one isolated ligament has proven to be superior or equal to the MPFL. Our reconstruction provided some increased benefit of reconstructing the MPTL and MPFL. This is most likely due to replacing the native ligament with a profoundly more robust ligament under tension.
Our study showed that the transected MPFL knee was the most unstable condition evidenced by that the force needed to displace the patella 1 cm was significantly less at all flexion angles when the MPTL and MPFL were transected compared with intact, MPFL reconstruction, MPTL reconstruction and both reconstructed. A twopound weight was clamped to the patellar tendon and suspended to simulate a small quadriceps-force as the normal physiologic status in an experimental setting. The force on the patellar tendon in our experiment would act to increase the joint reactive force and to dynamically stabilize the patella in the femoral trochlea. This may reduce the effect of release of the MPFL, but could better simulate normal patellofemoral mechanics.
There has been a multitude of biomechanical studies examining the medial patellofemoral ligament and its effect on medial restraint of the patella [7,8]. The MPFL has been widely accepted as the primary medial restraint to lateral patellar translation because of these studies. A study performed by Conlan et al. determined that the MPFL contributed 53% of soft-tissue restraint to lateral patellar translation [8]. Another study performed by Bedi et al. showed the force required to displace the patella 1 cm laterally was reduced by 14%-22% after cutting the MPFL [7]. Unlike a previous study that found the MPFL to be present in only 31% of dissected knees, we identified and isolated the MPFL in 100% of the knees in this current study [10].
With the multiple studies examining the role of the MPFL there are few cadaveric studies that observe the interaction of the other medial patellar stabilizers— medial retinaculum, the medial patellotibial ligament (MPTL), the medial patellomeniscal ligament (MPML), and the vastus medialis obliquus (VMO). The role of these secondary stabilizers has been studied in only a few studies. The results of those cadaveric studies are inconclusive regarding the role of the secondary medial patellar stabilizers [11]. In our study we specifically observed the MPTL and the MPFL. As expected, our study determined the force needed to displace the patella 1 cm was significantly less at all flexion angles when the MPTL and MPFL were sectioned (p<0.05).
Conlan et al. described the MPTL as functionally unimportant, but there was minor contribution to medial restraint from the MPML [8]. Alternatively, Hautamaa et al. examined the MPTL/MPML as a complex and found that these ligaments play a secondary role in restraining lateral patellar displacement [5]. They examined these ligaments as a complex because of the close approximation of these structures near the patella making accurate separation difficult. In our dissection the MPML and MPTL were in close proximity and it is easy to see why separation of these two ligaments would be difficult to reproduce. In addition to being difficult to separate routinely, we also concluded that repair of the MPML would not be realistic given the intracapsular association with the medial meniscus. Because of these assumptions we focused our attention on dissection and reconstruction of the MPTL.
A number of techniques for reconstruction of the MPFL have been described. Despite the graft choice, most MPFL reconstruction techniques are similar. In our institution, we commonly use an adductor magnus tendon autograft. A previous case series published subjective good results in 14 patients after this procedure [15]. In our study, we achieved increased strength against lateral translation in comparison the native MPFL—a result consistent with MPFL reconstructions in the literature [5,7,13]. This is desirable occurrence for surgeons who believe that the MPFL reconstruction can stretch after surgery. However, there may be a point at which reactive forces can be too large and increase medial instability [7].
There have been no reported cadaveric studies evaluating MPTL reconstruction. In our literature search we found a surgical technique using the medial one-third of the patellar tendon with a distally attached bone block [6]. This technique proved to be reproducible and more than sufficient collagen for reconstruction of the MPTL. Although the isolated MPTL reconstruction did not provide the same medial restraint as the reconstructed MPFL, the reconstructed MPTL did provide some medial restraint according to our data.
A strength of our study was performing radiologic imaging of every specimen in this study. This was done prior to reconstruction to rule out any osseous dysplasia that would contribute to inherent patellar instability. Another strength was the use of DVRTs to determine strain of the native ligaments.
Limitations
Clinical application could be limited by the fact that most dislocations occur during the second decade of life, and in this study our patients were significantly older [16,17]. Clinical application is also limited by a relatively small sample size. Further investigation of the MPML might be required to prove useful as another alternative (or additive) procedure for patellar instability.
Conclusions
The MPFL remains the primary medial stabilizer of the patella with the secondary stabilizers working in concert in preventing lateral patellar displacement. Our reconstruction provided some increased benefit of reconstructing the MPTL and MPFL.
Acknowledgment
The authors acknowledge Lin Gross, Rachel Toccalino, and E.J. Rozek of the Detroit Medical Center for their assistance in all aspects of this study.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics Statement
The study was reported via Human Research Determination Form to the institutional review board (IRB) of the Wayne State University (IRB# 2020035) and it was documented that no IRB approval was required (de-identified specimen does not constitute human subjects research). The study was reported via Human Research Determination Form to the institutional review board (IRB) of the Wayne State University and it was documented that no IRB approval was required (deidentified specimen does not constitute human subjects research).
References
2. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surgery, Sports Traumatology, Arthroscopy. 2012 Feb;20(2):331-6.
3. Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. The American journal of sports medicine. 2006 Aug;34(8):1254-61.
4. Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surgery, Sports Traumatology, Arthroscopy. 2006 Jan 1;14(1):7-12.
5. Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clinical Orthopaedics and Related Research (1976-2007). 1998 Apr 1;349:174-82.
6. Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surgery, Sports Traumatology, Arthroscopy. 2005 Oct 1;13(7):510-5.
7. Bedi H, Marzo J. The biomechanics of medial patellofemoral ligament repair followed by lateral retinacular release. The American Journal of Sports Medicine. 2010 Jul;38(7):1462-7.
8. Conlan T, Garth Jr WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. JBJS. 1993 May 1;75(5):682-93.
9. Ebied AM, El-Kholy W. Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surgery, Sports Traumatology, Arthroscopy. 2012 May 1;20(5):926-32.
10. Reider B, Marshall JL, Koslin B, Ring B, Girgis FG. The anterior aspect of the knee joint. The The Journal of bone and joint surgery American volume. 1981 Mar 1;63(3):351-6.
11. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. The American journal of sports medicine. 1998 Jan;26(1):59- 65.
12. Steensen RN, Dopirak RM, Mcdonald III WG. The Anatomy and Isometry of Themedial Patellofemoral Ligament: Implications for Reconstruction. The American Journal of Sports Medicine. 2004 Sep;32(6):1509-13.
13. Slocum DB, Larson RL, James SL. Late reconstruction of ligamentous injuries of the medial compartment of the knee. Clinical Orthopaedics and Related Research (1976- 2007). 1974 May 1;100:23-55.
14. Terry GC. The anatomy of the extensor mechanism. Clinics in Sports medicine. 1989 Apr;8(2):163.
15. Avikainen VJ, Nikku RK, Seppánen-Lehmonen TK. Adductor magnus tenodesis for patellar dislocation: technique and preliminary results. Clinical Orthopaedics and Related Research®. 1993 Dec 1;297:12-6.
16. Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. The American journal of sports medicine. 1986 Mar;14(2):117-20.
17. Vainionpaa SE, Laasonen ER, Silvennoinen TI, Vasenius JA, Rokkanen PE. Acute dislocation of the patella. A prospective review of operative treatment. The Journal of bone and joint surgery. British volume. 1990 May;72(3):366-9.
