Keywords
Food cravings; Eating disorders; Anorexia nervosa; Bulimia nervosa; Binge eating disorder
Food cravings
Food cravings;Eating disorders; Anorexia nervosa; Bulimia nervosa; Binge eating disorder
Food Cravings (FC) is the term commonly used to describe sensations related to an intense desire for specific consumption [1], and there are features that we separate into internal and external aspects related to FC [2]. The internal ones would be dietary restraint, food reward, impulsivity/inflexibility, emotions/thoughts/feelings about food, hunger/satiety/appetite and symptoms of anxiety/ depression. External aspects would be positive/negative events, food environment, advertising, cultural beliefs about food, specific places (i.e. kitchen) and the food itself. FC entails the food choice process (between two options the most desired tends to be chosen), thus being related to habits and memories. FC is also associated with events of emotional memory – when a desire for food occurs, but it is actually the search for the sensation a memory provides [3].
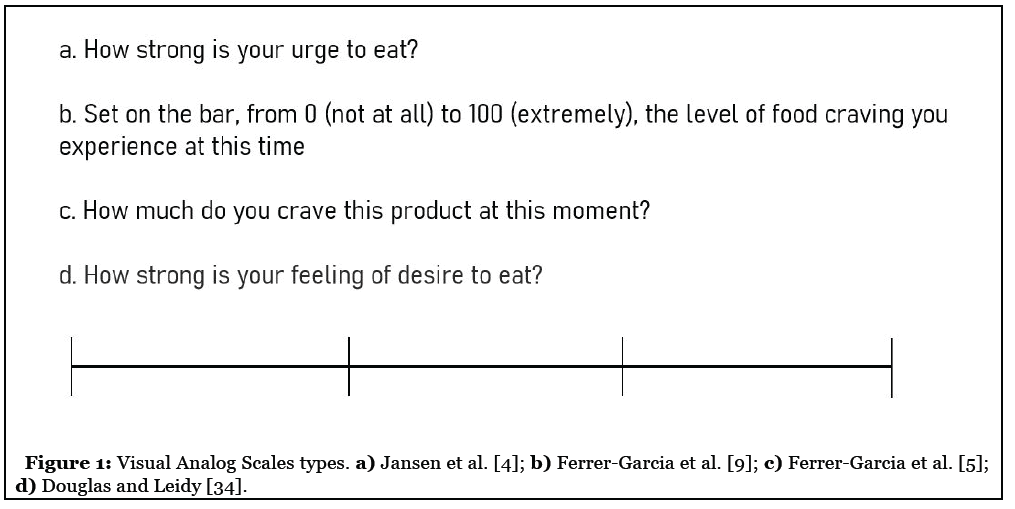
Our review of FC in EDs entitled “The body asks and the mind judges: Food Cravings in Eating Disorders” aimed to gather how FC was assessed in Anorexia Nervosa (AN), Bulimia Nervosa (BN) and Binge Eating Disorder (BED). Thirty-seven studies available that used eight different methodologies, such as Visual Analog Scales [4-10] (Figure 1) and different questionnaires [11-14] were under discussion [2]. The smallest part of the studies (n= 3) which investigated AN [5,15,16] as well as the role of dietary beliefs and inflexibility seems to differentiate AN in opposition to BN and BED. Such distinction is due to the fact that they have lower levels of FC in relation to BN, and also report higher levels of FC lowfat foods [5]. Future studies may investigate the role of neuropsychological characteristics and neural changes in this group.
Ten studies investigated neural aspects in BN and BED [14,17-25]. Possibly due to the culturally influenced view that FC is only related to binge eating, most studies have investigated individuals with BN and BED. However, a more neutral view of FC in the future may provide readings that will verify whether the evolution in AN is related to an increase in FC. The use of Repetitive transcranial stimulation (rTMS) seems to be a potential therapeutic intervention [26], and 1 session could reduce ratings of want to eat, urge to eat and sense of hunger for caloric foods (FC) according to Sutoh and colleagues [27]. rTMS aims to modulate cortical excitability and reduction of FC is measured by VAS. One single session of rTMS reduces FC in BN outpatients [27,28], and also reduction of salivary cortisol [21] that could be related to arises of FC to reduced negative sensations (emotional eating). Functional magnetic resonance imaging (fMRI) also could be applied for the study of neuronal related structures and alterations in EDs. For BN individuals, processing visual food stimuli and comparing oneself to other slim women increase anxiety, but not FC. When comparing their body against slim women, BN uses the insula more (i.e. reflect more on themselves) and the fusiform gyrus less (i.e. look less at the other’s actual shape) [23].
Also, we have seen a large increase in EDs in the population, and the progress of nutrition science coupled with the growth of nutritionism in popular discourses have been influencing the “search for health” by rigid means, sometimes called lifestyle [29]. In 2019, we found that 25% of university students had practiced a low-carb diet [30]. Within the group that carried out the diet, 35% associated with Intermittent Fasting (a practice spread by the simplification of the science of nutrition combined with lifestyle). Those who self-report low-carb practice had higher weight and levels of binge eating according to the Binge Eating Scale and higher FC levels (trait and state).
Eating Disorders (EDs) represent the best examples of a troubled relationship with food, where a series of behaviors and beliefs that have been influenced by the cultural factor, thus, it is common to believe that FC are wrong or responsible for the failure of treatments. Questioning studies that defend Food Addiction seems important: how will a compulsive individual see “tempting” food in a more neutral way, managing to include it in the appropriate context, quantity and frequency, if the relationship established with food is called addiction?
Understanding that the triggers are more significant than the desire itself, as the latter should not be subject to moralization, demands new approaches for the treatment of EDs, considering that a good relationship with food has been related to the unconditional permission to eat [31]. Intuitive Eating was developed by Evelyn Tribole and Elyse Resch in 1995, and since then a series of publications and reviews have been showing their role in the treatment of EDs [32,33].
The importance of multi-professional treatment and the possibility of pharmacological intervention aimed at FC can be associated with a nutritional approach that studies and recognizes the importance of FC. Besides, the attempt to stop eating food is often what sustains the loss of control. Taking this into account, during treatments that use the concept of Intuitive Eating, such as the one conducted in the Eating Disorders Program (AMBULIM/ PROTAD) in Brazil, nutritionists use the premise that the prohibition relationship (cognitive restraint and distorted beliefs) are associated with the emergence and maintenance of ED’s symptoms. Moreover, during treatment, the nutrition team works on unconditional permission to eat, combined with body perception (signs of hunger and satiety), awareness of FC and emotional triggers. Thus, the act of eating occurs for physical rather than emotional reasons, but FC can still be fulfilled. Psychological aspects and third-generation approaches are also useful for the association with FC, their study, and better understanding, both in aspects of research, as well as in clinical practice.
References
2. de Oliveira J, Cordás TA. The body asks and the mind judges: Food cravings in eating disorders. L’encephale. 2020 Mar 6.
3. Lee YH, Kim M, Lee M, Shin D, Ha DS, Park JS, et al. Food Craving, Seeking, and Consumption Behaviors: Conceptual Phases and Assessment Methods Used in Animal and Human Studies. Journal of Obesity & Metabolic Syndrome. 2019 Sep;28(3):148.
4. Jansen A, Broekmate J, Heymans M. Cue-exposure vs self-control in the treatment of binge eating: a pilot study. Behaviour Research and Therapy. 1992 May 1;30(3):235-41.
5. Veenstra EM, de Jong PJ. Reduced automatic motivational orientation towards food in restricting anorexia nervosa. Journal of Abnormal Psychology. 2011 Aug;120(3):708.
6. Rosenberg N, Bloch M, Avi IB, Rouach V, Schreiber S, Stern N, et al. Cortisol response and desire to binge following psychological stress: Comparison between obese subjects with and without binge eating disorder. Psychiatry Research. 2013 Jul 30;208(2):156-61.
7. Farci AM, Piras S, Murgia M, Chessa A, Restivo A, Gessa GL, et al. Disulfiram for binge eating disorder: an open trail. Eating behaviors. 2015 Jan 1;16:84-7.
8. Dakanalis A, Fernandez-Aranda F, Fusté-Escolano A, Ribas-Sabaté J, Riva G, Saldaña C, et al. External eating as a predictor of cue-reactivity to food-related virtual environments. Annual Review of Cybertherapy and Telemedicine 2015: Virtual Reality in Healthcare: Medical Simulation and Experiential Interface. 2016 Jan 28;219:117.
9. Ferrer-Garcia M, Pla-Sanjuanelo J, Dakanalis A, Vilalta-Abella F, Riva G, Fernandez-Aranda F, et al. Eating behavior style predicts craving and anxiety experienced in food-related virtual environments by patients with eating disorders and healthy controls. Appetite. 2017 Oct 1;117:284-93.
10. Pla-Sanjuanelo J, Ferrer-García M, Vilalta-Abella F, Riva G, Dakanalis A, Ribas-Sabaté J, et al. Testing virtual reality-based cue-exposure software: Which cue-elicited responses best discriminate between patients with eating disorders and healthy controls?. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2017 Jul 27:1-9.
11. White MA, Grilo CM. Bupropion for overweight women with binge eating disorder: Randomized doubleblind placebo-controlled trial. The Journal of Clinical Psychiatry. 2013 Apr;74(4):400.
12. Moreno-Domínguez S, Rodríguez-Ruiz S, Fernández-Santaella MC, Ortega-Roldán B, Cepeda-Benito A. Impact of fasting on food craving, mood and consumption in bulimia nervosa and healthy women participants. European Eating Disorders Review. 2012 Nov;20(6):461-7.
13. Spada MM, Caselli G, Fernie BA, Nikcevic AV,Ruggiero GM, Boccaletti F, et al. Metacognitions about desire thinking predict the severity of binge eating in a sample of Italian women. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2016 Jun 1;21(2):297-304.
14. Wolz I, Sauvaget A, Granero R, Mestre-Bach G, Baño M, Martín-Romera V, et al. Subjective craving and eventrelated brain response to olfactory and visual chocolate cues in binge-eating and healthy individuals. Scientific Reports. 2017 Feb 3;7(1):1-0.
15. Gendall KA, Sullivan PF, Joyce PR, Bulik CM. Food cravings in women with a history of anorexia nervosa. International Journal of Eating Disorders. 1997 Dec;22(4):403-9.
16. Moreno S, Warren CS, Rodríguez S, Fernández MC, Cepeda-Benito A. Food cravings discriminate between anorexia and bulimia nervosa. Implications for “success” versus “failure” in dietary restriction. Appetite. 2009 Jun 1;52(3):588-94.
17. Burgess EE, Sylvester MD, Morse KE, Amthor FR, Mrug S, Lokken KL, et al. Effects of transcranial direct current stimulation (tDCS) on binge-eating disorder. International Journal of Eating Disorders. 2016 Oct;49(10):930-6.
18. Gay A, Jaussent I, Sigaud T, Billard S, Attal J, Seneque M, et al. A Lack of Clinical Effect of High-frequency r TMS to Dorsolateral Prefrontal Cortex on Bulimic Symptoms: A Randomised, Double-blind Trial. European Eating Disorders Review. 2016 Nov;24(6):474-81.
19. Wonderlich JA, Breithaupt LE, Crosby RD, Thompson JC, Engel SG, Fischer S. The relation between craving and binge eating: Integrating neuroimaging and ecological momentary assessment. Appetite. 2017 Oct 1;117:294-302.
20. Van den Eynde F, Claudino AM, Mogg A, Horrell L, Stahl D, et al. Repetitive transcranial magnetic stimulation reduces cue-induced food craving in bulimic disorders. Biological Psychiatry. 2010 Apr 15;67(8):793-5.
21. Claudino AM, Van den Eynde F, Stahl D, Dew T, Andiappan M, Kalthoff J, et al. Repetitive transcranial magnetic stimulation reduces cortisol concentrations in bulimic disorders. Psychological Medicine. 2011 Jun;41(6):1329-36.
22. Van den Eynde F, Broadbent H, Guillaume S, Claudino A, Campbell IC, Schmidt U. Handedness, repetitive transcranial magnetic stimulation and bulimic disorders. European Psychiatry. 2012 May 1;27(4):290-3.
23. Van den Eynde F, Giampietro V, Simmons A, Uher R, Andrew CM, Harvey PO, et al. Brain responses to body image stimuli but not food are altered in women with bulimia nervosa. BMC Psychiatry. 2013 Dec;13(1):302.
24. Sutoh C, Koga Y, Kimura H, Kanahara N, Numata N, et al. Repetitive Transcranial Magnetic Stimulation Changes Cerebral Oxygenation on the Left Dorsolateral Prefrontal Cortex in Bulimia Nervosa: A Near-Infrared Spectroscopy Pilot Study. European Eating Disorders Review. 2016 Jan;24(1):83-8.
25. Simon JJ, Skunde M, Walther S, Bendszus M, Herzog W, Friederich HC. Neural signature of food reward processing in bulimic-type eating disorders. Social Cognitive and Affective Neuroscience. 2016 Sep 1;11(9):1393-401.
26. Grall-Bronnec M, Sauvaget A. The use of repetitive transcranial magnetic stimulation for modulating craving and addictive behaviours: a critical literature review of efficacy, technical and methodological considerations. Neuroscience & Biobehavioral Reviews. 2014 Nov 1;47:592-613.
27. Sutoh C, Koga Y, Kimura H, Kanahara N, Numata N, Hirano Y, et al. Repetitive Transcranial Magnetic Stimulation Changes Cerebral Oxygenation on the Left Dorsolateral Prefrontal Cortex in Bulimia Nervosa: A Near-Infrared Spectroscopy Pilot Study. European Eating Disorders Review. 2016 Jan;24(1):83-8.
28. Van den Eynde F, Koskina A, Syrad H, Guillaume S, Broadbent H, Campbell IC, et al. State and trait food craving in people with bulimic eating disorders. Eating Behaviors. 2012 Dec 1;13(4):414-7.
29. Mayes CR, Thompson DB. What should we eat? Biopolitics, ethics, and nutritional scientism. Journal of Bioethical Inquiry. 2015 Dec 1;12(4):587-99.
30. de Oliveira J, Figueredo L, Cordás TA. Prevalência de comportamentos de risco para transtornos alimentares e uso de dieta “low-carb” em estudantes universitários. Jornal Brasileiro de Psiquiatria. 2019 Dec;68(4):183-90.
31. Keirns NG, Hawkins MA. The relationship between intuitive eating and body image is moderated by measured body mass index. Eating Behaviors. 2019 Apr 1;33:91-6.
32. Tribole E, Resch E. Intuitive eating. Macmillan; 2012 Aug 7.
33. Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutrition Research Reviews. 2017 Dec;30(2):272-83.
34. Douglas SM, Leidy HJ. Novel Methodological Considerations Regarding the Use of Visual Analog Scale (VAS) Appetite Questionnaires in Tightly Controlled Feeding Trials. Current Developments in Nutrition. 2019 Jun;3(6):nzz061.
