Abstract
Introduction: Cytopathological examination is the main method for the screening of cervical cancer, its occurrence can be prevented or minimized through screening, with good coverage, quality of collection and analysis and women’s adherence to the examination.
Objective: To describe the quality of cytopathological exams performed at a family health unit in Salvador - Bahia during the years 2015 and 2016. Method: A cross-sectional study, of an exploratory descriptive character, was conducted, using a database from a previous study carried out in a health unit in Salvador / BA and approved by the Ethical Committee from State University of Feira de Santana.
Results: Preventive gynecological exams of 1,350 women were analyzed, but 330 (24.4%) of them could not be evaluated due to the absence of the report in the health unit and the presence of acellular or hypocellular material that prevented the analysis. From 1020 exams, 45 (3.3%) presented an unsatisfactory sample, without conditions for analysis, while 589 (43.19%) showed only squamous cells. From 392 (29.0%) reports with an adequate study sample, 150 (%) were women with a mean age of 38.49 years. These were located and composed the final sample of the present investigation.
Final Considerations: We suggest the need for investments in continuing education for professionals involved in performing cytopathological exams, in order to ensure the right of women to comprehensive and quality health care.
Keywords
Cervical neoplasms, Cervical cancer screening, Gynecological preventive
Introduction
Cytopathological examination (CE) is the main method for early identification of cervical cancer (CC) and its precursor lesions. Also known as Papanicolau, according to [1], it is recognized as a fast, low cost, and effective for detection, although its vulnerability for collection bias, plate preparation and its interpretation.
Regarding sampling for this assay, its elegibility evaluation has been considered a quality indicator, and the sample that has a representative amount of well distributed, fixed and colored cells, allowing a diagnostic conclusion, is considered adequate for analysis. The samples may contain squamous, glandular and metaplastic cells [2]. On the other hand, samples with an unsatisfactory reading due to technical aspects or cellular sampling leads to an unfeasible diagnosis [2].
Most of cervical cancer cases could be prevented by the adherence to cytopathological examination, with a good coverage screening, quality sample collection and correct analysis [3]. According to the World Health Organization (WHO), with at least 80% of the population screened, with confirmed diagnosis and adequate therapy, there could be a reduction from 60 to 90% of cervical cancer cases. Some developed countries show a reduction of CC incidence of 80% in locations where cytopathological examination was performed with quality and the coverage was reached, and diagnosis was confirmed and adequate therapy was delivered [4].
In order to reduce CC morbidity and mortality in Brazil, the Ministry of Health (MoH) recommends annual examination for sexually active women who are 25 to 64 years old; women younger than 25 years old should avoid this examination. The examination can be performed every three years for women presenting two consecutive normal results, with an interval of one year between them. The first two examinations must be performed annually, and, if both of results are negative, the next must be taken every three years [2,4].
Some factors influence on the detection of lesions, such as insufficient material collection; inadequate smears and plate preparation; technical deficit in cytopathology laboratories; women’s low adherence on being examined [5]. Therefore, the sample analysis can be compromised due to an unsatisfactory collection, invalidating the CE as a screening measure for CC [6]. A false-negative result compromises the patient’s prognosis since the nonvisualization of suggestive lesions of CC may increase its morbimortality [7].
Therefore, the conduction of research regarding the quality of CC screening may offer information that evidence the quality of CE performed, as well as the attainment of parameters to guide strategies to personnel qualification regarding sample collection in CE. The aim of the present study is to describe the quality of cytopathological examinations performed at a Family Health Unity (FHU) in Salvador - Bahia, between 2015 and 2016.
Material and Methods
We performed a cross sectional, descriptive and exploratory study, using a database from a previous study. The present study was approved by an Ethical Research Committee (n. º 2.548.705).
The research context was based on a FHU from Salvador County, state of Bahia. Data from patient hospital records and registry from CE collection were analyzed between December 2017 and June 2018, in order to identify potential participants. Initially, a total of 1,350 women who underwent cytopathological examinations were identified. Their medical records were accessed and verified if there was an adequate sample of material for such examination, and computed those that had unsatisfactory samples or presence of squamous cells in them. Afterwards, the availability of the reports of these exams was evaluated, and/or a request for a second copy was made. Finally, the quality of their records was analyzed in terms of detailing the description of the results.
Subsequently, the women who presented adequate samples for the present investigation were located by community health agents and invited to participate in this research. Those who accepted signed the Informed Consent Form and were interviewed using a semistructured questionnaire. Such procedures allowed all women registered at the USF to be selected for the study, presenting results of CE with squamous and glandular cells, with or without precursor lesion for CC, and with inconclusive results. According to the eligibility criteria, initially 29% of women would be eligible to participate in the study. However, at the end of the aforementioned sample selection steps, only 150 were included in the final phase of the study, which represented 11% of potential participants.
Descriptive analysis comprised simple and relative frequencies regarding categorical variables, and central tendency measures for continuous variables. Statistical analyses were performed on Statistical Package for the Social Sciences (SPSS) version 17.0 and STATA version 10.0 software.
Results
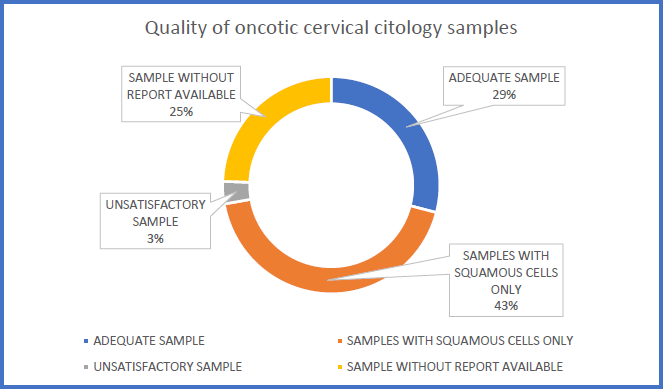
Between December 2017 and June 2018, 1,350 cytopathological examinations were performed in San Martin 1 FHU. Nonetheless, only 392 reports presented adequate samples, whilst 3.3% had unsatisfactory sample and 43.19% showed only squamous cells. We point out that 24.44% (25%) of examinations could not be evaluated because its reports were not available in the health unit, even with a second copy being requested, or did not show a detailed registry (Figure 1).
Figure 1. Quality of oncotic cervical citology samples. Salvador, BA, Brazil (n=1,350).
Participants were in average 38.49 ± 13.68 (%) years old (median of 37 years old), and the majority self-reported as Black and/or Brown (138/92.0%). Most part of women in the sample did not have a Professional occupation at the time of the interview (89/59.3%) (Table 1).
| Characteristics | n | % |
|---|---|---|
| Age | ||
| Mean | 38.49 ± 13.68 | |
| Median (min-max) | 37 (18 - 81) | |
| Race/skin color | ||
| White/Yellow/Indigenous | 12 | 8.0 |
| Black/Brown | 138 | 92.0 |
| Education level | ||
| = 8 years | 95 | 63.3 |
| < 8 years | 55 | 36.7 |
| Occupation | ||
| Employed | 61 | 40.7 |
| Unemployed | 89 | 59.3 |
| Smoker | ||
| No | 142 | 94.7 |
| Yes | 8 | 5.3 |
| Alcohol consumption | ||
| No | 71 | 47.3 |
| Yes | 79 | 52.7 |
| Physical activity | ||
| = 2 days/week | 31 | 20.7 |
| 0 to 1 day/week | 119 | 79.3 |
Regarding lifestyle, there was a prevalence of women consuming alcoholic beverages (79/52.7%), non-smokers (142/94.7%) and with low consumption of ilicit drugs (n=5/3.3%). We also observed that the majority of women had a low frequency of physical activity (119/79.3%) (Table 1).
Results of reproductive conditions show that the majority of women had the first sexual contact up to 18 years old (102/70,0%), and most of them also referred to relate themselves with up to 4 partners (102/68.0%), and almost all of them had one fixed partner (149/99.3%) (Table 2).
| Characteristics | n | % |
|---|---|---|
| Amenorrhea | ||
| No | 78 | 52.0 |
| Yes | 72 | 48.0 |
| First sexual contact | ||
| > 18 years old | 45 | 30.0 |
| = 18 years old | 105 | 70.0 |
| Number of sexual partners | ||
| = 4 partners | 102 | 68.0 |
| > 4 partners | 48 | 32.0 |
| Fixed sexual partner | ||
| Yes | 149 | 99.3 |
| No | 1 | 0.7 |
| Misscarriage | ||
| None | 101 | 67.3 |
| 1 or more | 49 | 32.7 |
| Time interval between preventive examinations | ||
| Less than 1 year | 20 | 13.3 |
| 1 year or more | 130 | 86.7 |
| Use of hormonal contraceptives | ||
| Yes | 84 | 56.0 |
| No | 66 | 44.0 |
| Adequate use of hormonal contraceptive | ||
| Yes | 135 | 90.0 |
| No | 15 | 10.0 |
| Yes | 52 | 34.7 |
| No | 98 | 65.3 |
| Regular condom use | ||
| Yes | 11 | 7.3 |
| No | 139 | 92.7 |
| Adequate condom use | ||
| Yes | 9 | 6.0 |
| No | 141 | 94.0 |
| Family record of CC | ||
| Yes | 137 | 91.3 |
| No | 13 | 8.7 |
The majority of women reported more than one year of interval between the last two gynecological preventive examinations (130/86.7%) and most of them reported using of hormonal contrapectives (86/56.0%) adequately (135/90.0%); similarly, most of women reported they did not use other type of contraceptives (98/65.3%). There were few reports regarding regular (11/7.3%) and adequate use of condoms (141/94.0%) (Table 2).
We observed from cytopathological examination records that only a few women showed precursor lesions of CC (17/11.2%), where the majority of lesions were Atypical Squamous Cells of Undetermined Significance (ASCUS) (7/4,7%), and the least observed were atypical glandular cells of undetermined significance (1/0.7%). There was also a low frequency of ASCUS in possibly non neoplasic cells, cannot exclude a high grade intraepithelial lesion (HSIL) (2/1.3%), of low grade intraepithelial lesion, including human papillomavirus infections, mild dysplasia and intraepithelial cervical neoplasia I (low grade intraepithelial lesion) (5/3,3%), and high grade intraepithelial lesions (intraepithelial cervical neoplasia II and III, in situ carcinoma) (2/1,3%) (Table 3).
| Characteristics | n | % |
|---|---|---|
| Presence of lesion | ||
| No | 133 | 88.7 |
| Yes | 1 | 11.2 |
| Cellular changes | ||
| ASCUS | 7 | 4.7 |
| ASC-H | 2 | 1.3 |
| AGC | 1 | 0.7 |
| LSIL | 5 | 3.3 |
| HSIL | 2 | 1.3 |
| Not applicable | 133 | 88.7 |
| Atrophy with inflammation | ||
| No | 138 | 92.8 |
| Yes | 2 | 8.0 |
| Vulvar lesion | ||
| No | 144 | 96.0 |
| Yes | 6 | 4.0 |
| Vaginal lesion | ||
| No | 149 | 99.3 |
| Yes | 1 | 0.7 |
| Leukorrhea | ||
| No | 67 | 44.7 |
| Yes | 83 | 55.3 |
| Microbiota | ||
| Physiological | 104 | 69.3 |
| Pathological | 46 | 30.7 |
| Metaplasia | ||
| No | 148 | 98.7 |
| Yes | 2 | 1.3 |
| Benign alterations | ||
| Normal | 149 | 99.3 |
| Altered | 1 | 0.7 |
| Onset of malignancy | ||
| Positive | 23 | 15.1 |
| Negative | 127 | 83.6 |
We also observed the presence of leukorrhea in the most part of examination reports (83/55.3%); pathological microbiota was less frequent than physiological (46/30.7%). Metaplasias were rare (2/1.3%), as well as benign alterations (1/0.7%); however, positivity for malignancy was more frequent (23/15.1%) than the two categories cited above (Table 3).
Discussion
Regarding the initial number of examinations evaluated (n=1,350), only 29% had an adequate collection for diagnosis. Thus, more than 1,000 (71%) women did not have the opportunity to be screened regarding CC or its precursor lesions. That is because the sample was insufficient, unsatisfactory or only had squamous cells, therefore, without conditions for an adequate diagnosis.
Moreover, the examination alterations frequency was 11.2%; therefore, there is a possibility that more than 112 women had these alterations at the time of sample collection, but were not diagnosed, or did not receive a control measure or treatment for such alterations, and did not have the right to know their real gynecological health status.
On the other hand, the Brazilian MoH recommends a minimum frequency of unsatisfactory samples of 5% as criteria for quality of collection and sample preservation in the screening examination for CC [2]. We observed in the present study that the frequency of unsatisfactory samples was according to the Brazilian MoH recommendation, although values close to zero better indicate an adequate screening [8].
In contrast, Santos [9] showed the elevated frequency of unsatisfactory samples on vaginal cytopathological examinations in Brazilian states. The state of Maranhão had the best evidence for showing a frequency of 5.6%, while Rio Grande do Norte had a frequency of 2.0%. Centralwestern, Southeast and Southern regions had states with a frequency close to the Brazilian MoH recommendation. In contrast, in a study performed at Doresópolis, Minas Gerais, all plates (100%) were considered adequate for cytopathological examination [10]. Therefore, since sample adequacy is an important indicator of quality in cytopathological examinations [2], it is a positive aspect regarding CC screening in the family health unit evaluated in the present study.
This examination is important for the prevention of CC and has a low cost, therefore, the personnel qualification is essential and imperative [7]. This is probably because the big amount of unsatisfactory samples may be related to personnel accuracy during the cytopathological examination.
Adequate cytopathological examination is mandatory for ensuring women’s health, which is a major social right protected by the current legal framework [11]. Social, political and economic policies focused on the reduction of risk for diseases and harms is a State’s responsability. The Unified Health System (Sistema Único de Saúde – SUS) forecasts that access to health must happen in a universal and equitable manner, looking forward to health promotion, protection and recovery [12]. The above mentioned collection involves manual work, and, therefore, investments on health professionals qualification is required.
Underpinning with the present study, results from a women’s health research, conducted at Aracaju, Sergipe, showed that only 46.2% (154) of samples were adequate for the analysis. The same study showed that cytopathological examination, cervical oncotic cytology test, is considered the best procedure to detect the first lesions, which indicates its systematic undertaking in women who are 25 to 64 years old. Finally, the authors point that social, economic, and behavioral factors are associated to examination adherence, therefore, competing for a reduction in survival indicators, when disease is diagnosed in an advanced stage [13].
In contrast, in order to avoid the low frequency of adequate samples, showing squamous and glandular cells, the collection must be representative of the squamocolumnar junction. The presence of endocervical and metaplastic cells in cytopathological smears has been considered as an indicator of collection quality, because it is the main source of pre-neoplastic lesions [14]. Thus, the squamocolumnar junction is the part with the highest occurrence of preneoplastic lesions, and endocervical and metaplastic cells must be present in samples for cytopathological examination; this works as an indicator for the lack of guidance and training of personnel involved in the collection procedures. Namely, it is possible to consider that the aim of screening for CC from examinations has been unsuccessful, besides the wrong use of public financial resources and its impact in women’s health that failed to obtain information regarding their gynecological condition and possible treatments.
Furthermore, in case of an unsatisfactory result, the patient must redo the examination after a period of six to twelve months, since this timeframe may enable early CC diagnosis, and consequently the improvement of therapeutical response, in spite of the burden of the examination recurrence [15]. This happens as one more disadvantage for the patients, considering that they will have to return to the health unit for a new sample collection for the smears, with possible expenses with displacement, work absence and discomfort at the collection moment. However, this return to the health unit does not happen quite often, and, therefore, these women lose the opportunity of an early diagnosis of possible harms, such as CC. The age range of 25 to 64 years, that predominated in the present study was also found in Aracaju, Sergipe [16]. These findings respond to the Brazilian MoH, and in this age range, precursor CC lesions are frequent [2]. However, it is important to establish a minimal age for this age range.
According to the Brazilian MoH, women with no sexual activity record should not be screened for CC. However, it also points that screening may prevent the majority of cervical neoplasia, through the abnormal alterations identified in cervical cells (pre-neoplasia) [2], although these affirmations are contrary to the indication of screening onset at 25 years old. Thus, we understand that these arguments are controversial, favoring the suggestion of anticipating the age of onset of screening examinations.
According to Sasieni et al. [17], the incidence of CC in young women is low, and there is evidence of screening in women younger than 25 years old being less efficient than in older women. Similarly, in women younger than 25 years old LSIL are predominant, which regress spontaneously in most cases, and that annual examination does not increase significantly the protective effect of screening. Moreover, the Brazilian MoH emphasize that examinations out of target age range and recommended periodicity could overload health services, and compromise access for those that have a precise indication. Namely, indiscriminate screening risk for women up to 24 years old would outweigh its possible advantages [2,18].
Vetrano et al. observed that international data showed a percentage of 12 to 45% of sexually active adolescents that had been screened for CC [19]. Hence, the majority of these women should have had indication for systematic CC screening, but not because they were young. In this regard, it is possible that many of these women may have precursor lesions, or other women needing treatment, but are not included in the current policies.
In addition, women that are not screened in the last two appointments show a four-time higher risk of CC compared to those screened at the adequate period. Those that were not screened in an early appointment, but lately, also showed an elevated risk. Besides, being screened only with regular results has been associated to a CC from squamous cells risk reduction of 89%, compared to those that were not screened, but only 60% of reduction to adenocarcinoma [20].
Therefore, with the early onset of sexual activities, pregnancy and sexually transmitted infections, we understand that this is a highly vulnerable group regarding the future development of CC. A study performed in Sao Paulo showed that on average, the onset of sexual activities happens at 14 years old, in contrast to the Brazilian MoH recommendations [21]. Thus, there is a need for a policy revision regarding women’s health, in order to reduce the minimum age recommended for the onset of systematic CC screening, including younger women, for instance those younger than 20 years old.
Accordingly with the present results, the majority of women interviewed in a study in Rio Branco, Acre, were also Brown (89.1%) and had more than two sexual partners lifelong (70%) [22]. However, considering the social and historical context of Salvador County, the high number of Black/Brown women may not represent the interference of race/color on a higher risk for CC lesions in this sample.
In contrast to the findings from the present study, Borges et al. (2012) observed a higher adherence to the preventive examination in those women who practiced in physical activity (82.2%). A higher prevalence of nonsmokers in the present sample (94.7%) was also described in Porto Alegre, Rio Grande do Sul (75%). This low frequency is satisfactory, considering that smoking is a risk factor for CC development [14].
We observed a low proportion of vulvar and vaginal lesions in the present sample. Recurrent vulvovaginal infections are very frequent and has social and psychological consequences [24]. According to Curty et al. [25], in Fortaleza, Ceará, the reasons to cytopathological examinations are related to vulvovaginitis, which represents 70% of complaints in gynecological consultations [26]. However, in the present study, patients looked for examination preventively; that evidences the success of health education initiatives focused on the present health unit recipients, in spite of inquiries regarding the quality of CC screening, considering weaknesses on sample collections that may contribute to a reliable diagnosis.
Moreover, we also observed in this study a high proportion of women without precursor CC lesions (88.7%), similarly to results observed by Silva in 2014 (86.8%). Typically, we observed a high number of women presenting regular results for the samples analyzed. That may indicate that those women that seek for extra health assistance may have their gynecological and reproductive health highly ensured.
Among possible cellular alterations, HSIL are truly precursor CC lesions, given its potential effect on disease progression. Therefore, its detection is considered as main focus of secondary prevention of CC [15]. The present findings show that only 1.3% of examinations showed HSIL. However, if all examinations performed in the present study (n=1350) could have had a diagnosis, this proportion would represent a hypothetical number of 18 women with HSIL instead of two. Therefore, 16 women may have developed CC, whether or not they sought for early screening.
Finally, we point for the possible interference of the present sample size on the findings. This raises the need for studies with more robust samples. However, regardless of the sample size, we recognize the waste of public financial resources on ineffective examinations, low effectiveness on CC screening by primary health care, and the need for higher investments on personnel qualification and the revision of current clinical protocols for diagnosis, in order to have a better CC combat. A successful experience was showed by Jakpbcynski et al. [27] with personnel qualification. They obtained a better sample, representation of required epithelium and examination results.
Final Considerations
The high proportion of unsatisfactory samples described in the present results raises the need for investments on systematic qualification of personnel involved in cytopathological examinations. That is relevant considering the identification of women that reported having many partners, therefore, being in higher risk for general gynecological alterations, including cervical cancer. In contrast, it requires additional costs and discomfort on recurrence of examinations, and may impact on the adherence for the systematic disease screening.
The proportion of unsatisfactory samples in cytopathological examinations is an indicator. It is related to the quality of collection, and also shows the proportion of samples that are considered inadequate or insufficient for diagnosis, therefore, requiring another examination. Moreover, it allows the evaluation and formulation of qualification of human resources, in order to enhance financial resources and avoid loss in women’s adherence to the examination.
On the other hand, the high frequency of young and sexually active women, that have more than one partner, and with a relatively low use of condoms, is associated with a higher risk for gynecological diseases. Therefore, the current minimal age for cervical cancer screening may be excluding these women. We understand the need for the implementation of protocols, in order to include these women in the screened group, and to standardize the collection and laboratory techniques, and to enhance and to streamline the diagnosis of precursor lesions for this type of cancer. Thus, this is possible if the State accomplish its duty of ensuring women the realization of their fundamental right for health, focusing on prevention and early detection of diseases and possible harms.
Thus, more studies regarding this topic are needed, especially those that explore the adequacy of collection and analysis of cytopathological examination, as an important tool on cervical cancer control, besides the effective prevention of its risk factors, in order to reduce the social and economic impact of this problem.
References
2. Instituto Nacional de Câncer José Alencar Gomes da Silva. Coordenação de Prevenção e Vigilância. Divisão de Detecção Precoce e Apoio à Organização de Rede. Diretrizes brasileiras para o rastreamento do câncer do colo do útero. 2. ed. rev. atual. – Rio de Janeiro: INCA, 2016.
3. Gontijo RC, Derchain SF, Roteli-Martins C, Sarian LO, Bragança JF, Zeferino LC, Silva SM. Avaliação de métodos alternativos à citologia no rastreamento de lesões cervicais: detecção de DNA-HPV e inspeção visual. Revista Brasileira de Ginecologia e Obstetrícia. 2004;26:269-75.
4. Ministério da Saúde. Política Nacional de Atenção Integral à Saúde da Mulher: princípios e diretrizes. 1 ed., 2 reimpr. Brasília: Editora do Ministério da Saúde, 2011.
5. Lapin GA, Derchain SF, Tambascia J. Comparação entre a colpocitologia oncológica de encaminhamento e a da gravidade das lesões cervicais intra-epiteliais. Revista de Saúde Pública. 2000;34:120-5.
6. Amaral RG, Manrique EJ, Guimarães JV, Sousa PJ, Mignoli JR, Xavier AD, Oliveira A. Influência da adequabilidade da amostra sobre a detecção das lesões precursoras do câncer cervical. Revista brasileira de ginecologia e obstetrícia. 2008;30:556-60.
7. Leitão NM, Pinheiro AK, Anjos SD, Vasconcelos CT, Nobre RN. Avaliação dos laudos citopatológicos de mulheres atendidas em um serviço de enfermagem ginecológica. Revista Mineira de Enfermagem. 2008;12(4):508-15.
8. Instituto Nacional de Câncer José Alencar Gomes da Silva. Monitoramento das ações de controle dos cânceres do colo do útero e de mama. Informativo Detecção Precoce, v. 3, n. 3, p. 1-12, ago/dez, 2012.
9. Santos KM. Distribuição espacial da mortalidade por câncer de colo de útero no Brasil, 1996 a 2009: ecocuidado de enfermagem (Master’s thesis).
10. Silva PV, Araújo A, Araújo MRN. Análise da cobertura do exame citopatológico do colo do útero no município de Doresópolis-MG. Revista de Enfermagem do Centro Oeste Mineiro. 2011;1(2):154-163.
11. BRASIL. Constituição (1988). Constituição da República Federativa do Brasil. Brasília, DF: Senado Federal: Centro Gráfico, 1988.
12. Lei nº 8.080, de 19 de setembro de 1990. Lei Orgânica da Saúde. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Brasília, set. 1990.
13. dos Santos Silva MA, Teixeira ÉM, Ferrari RA, Cestari ME, Cardelli AA. Fatores relacionados a não adesão à realização do exame de Papanicolau. Rev Rene. 2015;16(4):532-9.
14. Ughini SF. Importance of the quality of preventive test collection for the diagnosis of endocervical and endometrial glandular neoplasms. RBAC. 2016;48(1):39-45.
15. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Controle dos cânceres do colo do útero e da mama / Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Atenção Básica. – 2. ed. – Brasília: Editora do Ministério da Saúde, 2013.
16. Ferreira JE, Alves MC, Martins MD, de Santa MD, Gonçalves MC. Perfil da população atendida em um consultório de atendimento integral à saúde da mulher. Caderno de Graduação-Ciências Biológicas e da Saúde- UNIT-SERGIPE. 2015 Oct 26;3(1):127-40.
17. Sasieni P, Castanon A, Cuzick J. Effectiveness of cervical screening with age: population based case-control study of prospectively recorded data. Bmj. 2009 Jul 29;339.
18. Instituto Nacional de Câncer José Alencar Gomes da Silva. Monitoramento das ações de controle dos cânceres do colo do útero e de mama. Informativo Detecção Precoce, v. 5, n. 1, p. 1-8, jan/abr, 2014.
19. Vetrano G, Lombardi G, Di Leone G, Parisi A, Scardamaglia P, Pate G, et al. Neoplasia intraepitelial cervical: fatores de risco para persistência e recorrência em adolescentes. Eur J Gynaecol Oncol. 2007;28(3):189- 92.
20. Wang J, Elfström KM, Andrae B, Nordqvist Kleppe S, Ploner A, Lei J, Dillner J, Sundström K, Sparén P. Cervical cancer case–control audit: Results from routine evaluation of a nationwide cervical screening program. International journal of cancer. 2020 Mar 1;146(5):1230-40.
21. Cirino FM, Nichiata LY, Borges AL. Conhecimento, atitude e práticas na prevenção do câncer de colo uterino e HPV em adolescentes. Escola Anna Nery. 2010;14:126-34.
22. do Prado PR, Koifman RJ, Santana AL, da Silva IF. Characterization of the profile of women with ASCUS/ AGC, LSIL and HSIL cytological results according to sociodemographic, epidemiological and reproductive factors in Rio Branco-AC, Brazil. Brazilian Journal of Cancerology. 2012 Sep 28;58(3):471-9.
23. Borges MF, Dotto LM, Koifman RJ, Cunha MD, Muniz PT. Prevalência do exame preventivo de câncer do colo do útero em Rio Branco, Acre, Brasil, e fatores associados à não-realização do exame. Cadernos de Saúde Pública. 2012;28:1156-66.
24. Kalia N, Singh J, Kaur M. Microbiota in vaginal health and pathogenesis of recurrent vulvovaginal infections: a critical review. Annals of clinical microbiology and antimicrobials. 2020 Dec;19(1):1-9.
25. Curty G, et al. O papel do microbioma cervicovaginal na gênese e como biomarcador de neoplasia intraepitelial cervical pré-maligna e câncer cervical invasivo. Jornal internacional de ciências moleculares. 2019;21(1):222.
26. Soost HJ, Lange HJ, Lehmacher W, Ruffing-Kullmann B. The validation of cervical cytology. Sensitivity, specificity and predictive values. Acta cytologica. 1991 Jan 1;35(1):8-14.
27. Jakobczynski J, Frighetto M, Perazzoli M, Dambrós BP, Dallazem B, Kirschnick A. Capacitação dos profissionais de saúde e seu impacto no rastreamento de lesões precursoras do câncer de colo uterino. RBAC. 2018;50(1):80-5.