Abstract
Since its discovery in December 2019 severe acute respiratory syndrome coronavirus-2 (SARS-COV2), coronavirus disease-19 (COVID-19) pandemic has opened up a pandora’s box and put the entire health-care industry globally under trial by fire. Neurological manifestations of it started becoming apparent in first few months and as of now we are still facing never-ending gamut of central nervous system (CNS) disorders related to SARS-COV-2 infection. Spinal cord involvement in COVID-19 although very well documented, overall remains uncommon. Here we present an interesting case of spinal cord hemorrhage in a patient with COVID-19 positive status, the first of its kind to our knowledge in this ever so expanding spectrum of nervous system manifestations of SARS-COV2.
Keywords
COVID19, CNS manifestations, Spinal cord, Spinal cord hemorrhage
Introduction
The pandemic of COVID-19 which has the global spread was first recognized in December 2019 in Wuhan, China is the 5th pandemic since 1918 Spanish flu pandemic [1]. SARS-CoV-2 then spread to all the parts of the world causing paralysis of the healthcare infrastructure world-wide and having devastating effects on the global economy. COVID-19 has proven to be a systemic illness with wide range of multi-organ involvement rather than an illness involving respiratory system in isolation [2]. Neurological manifestations of COVID-19 are likely related to both, direct neuro-invasive properties of the virus and indirect consequences of effects of multi-system impairment [3,4]. While significant progress has been made in knowing all the varied neurological presentations of COVID-19 syndrome, new entities keep getting added to the already substantial list.
Neurological manifestations of COVID-19 are broadly divided into those related to central nervous system and those related to peripheral nervous system. Spinal cord involvement in COVID-19 is well documented and as per a systemic review, wide range of spinal cord disorders can happen during the course of COVID-19 illness such as acute transverse myelitis, acute necrotizing myelitis, acute disseminated encephalomyelitis, spinal cord ischemia, spinal epidural abscess, etc [5].
We report an interesting case of primary spinal cord hemorrhage in a patient with COVID-19 infection.
Case Report
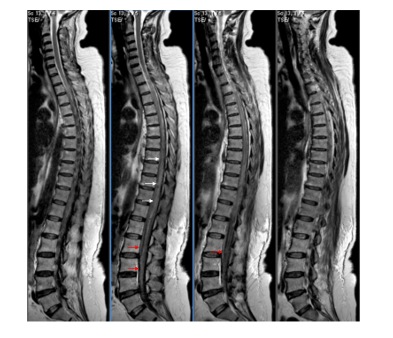
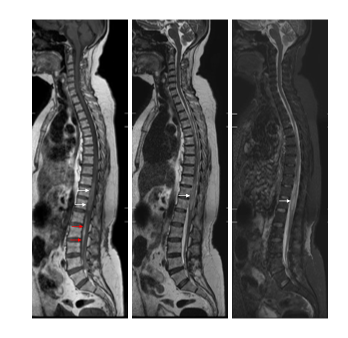
A 73 years old diabetic lady was admitted at a hospital in Raipur, India with complaints of fever, cough, and malaise for 3 days. During initial evaluation, her COVID-19 positive status was confirmed and was treated with tablet azithromycin, multivitamins, and supportive care. On day-3 of hospitalization, she developed acute onset paraparesis with urinary retention. She was evaluated with MRI of the spine and it revealed spinal cord hemorrhage with intradural extension from D9 to D12 level (Figure 1) and raised the possibility of a Dural AV-fistula. She was shifted to Mumbai for further evaluation and management. On initial assessment, she had hypotonia, paraplegia, and areflexia in her lower limbs. Sensory examination revealed sensory level at D9-D10. On basis of first MRI suggesting possibility of spinal Dural AV-fistula, digital subtraction angiography (DSA) was performed, which however did not reveal any vascular abnormality. A joint case discussion was then held with a team of neurologist, neurosurgeon, and radiologist which mutually concluded to repeat the MRI of spine. Follow up MRI revealed evidence of persistent intramedullary hemorrhage from D9 to D12 levels with no flow voids and resolving cord oedema (Figure 2). Details of primary hospitalization and treatment sheets were reviewed to find out possible culprits for primary spinal cord hemorrhage which revealed mildly deranged prothrombin time (PT/INR 1.5), elevated D-Dimer levels (3600 ng/ml), normal platelet counts, bleeding time, clotting time and activated partial thromboplastin time. Medication history revealed that patient received 3 days of subcutaneous low molecular weight heparin (LMWH) in therapeutic doses (1 mg/kg twice a day) during her primary hospitalization for COVID-19 infection [6]. She was managed conservatively at our institute with aggressive limb physiotherapy and out of bed mobilization. She was followed up and there was only marginal improvement in her clinical condition and she still requires significant support for her activities of daily living.
Figure 1. 1st MRI. T2W sagittal images reveal intramedullary hemorrhage from D9 to D12 level (white arrows) with extension into the intradural extramedullary space (red arrows).
Figure 2. 2nd MRI. T1W, T2W, and STIR sagittal images reveal resolving intramedullary hemorrhage (white arrows) its intradural extramedullary component (red arrows). The cord edema has reduced.
Discussion
Despite abundant accumulation of information concerning neurological manifestations of COVID-19 in last 3 years, involvement of spinal cord during COVID illness overall remains infrequent. Wide range of spinal cord manifestations can happen during the course of COVID-19 illness such as acute transverse myelitis (ATM), acute necrotizing myelitis, acute encephalomyelitis, spinal cord infarction, spinal subdural abscess etc [5,7,8]. Spinal cord involvement during COVID-19 illness can be either a para-infectious or post-infectious complication of the illness.
Both thrombotic and bleeding complications during COVID-19 infection are very well known and add significantly to the morbidity and mortality of the patients [9,10]. Various risk factors predisposing to the same have been identified and as per one study, raised D-Dimer level at the time of hospitalization was associated with increased risk of bleeding, thrombotic complications, critical illness and death [11]. Major sites for bleeding include intracerebral hemorrhage, bleeding into soft tissues, muscles and retroperitoneal spaces, adrenal hemorrhage etc [12,13].
Although hemorrhagic strokes are well recognized during the course of COVID-19 illness, primary spinal cord hemorrhage is not yet documented in individual case reports or case-series globally. A large case series of intracerebral hemorrhage (ICH) amongst COVID-19 patients found that patients with ICH were slightly older, had more traditional vascular risk factors and received systemic anticoagulation more than those without ICH [11].
Use of systemic anti-coagulation in therapeutic doses during the phase of acute COVID-19 illness does indeed predispose patients to the risk of bleeding complications. Our patient developed acute onset paraplegia on day-3 of hospitalization for her COVID19 infection and her medical charts revealed delivery of therapeutic doses of subcutaneous low molecular weight heparin for 3 days. Her labs revealed elevated D-Dimer level (3600 ng/ml) and deranged prothrombin time (PT/INR 1.5). Rest of the hematological, biochemical, and coagulation parameters of the patient were within normal range.
As spinal cord hemorrhage during the course of COVID-19 infection is not documented in the literature so far and initial MRI suggested possibility of a Dural A-V fistula, extensive workup with DSA was performed to rule out vascular malformations. This intriguing case of primary spinal cord hemorrhage is likely related to the coagulopathy, either due to primary COVID-19 infection or its treatment related complications.
We would like to bring to attention a probable new addition to the never-ending spectrum of COVID-19 related spinal cord manifestations. Although bleeding complications during COVID-19 illness are well-known, this intriguing case of spinal cord hemorrhage is one of the first of such spinal cord involvement to our knowledge. As such unusual complications may have catastrophic prognosticating implications on patient’s overall quality of life, we would like to emphasize the judicious use of anti-coagulation therapy in only absolutely indicated cases to prevent occurrence of such cases in future.
References
2. Roberts CM, Levi M, McKee M, Schilling R, Lim WS, Grocott MP. COVID-19: a complex multisystem disorder. British Journal of Anaesthesia. 2020 Sep 1;125(3):238-42.
3. Whittaker A, Anson M, Harky A. Neurological manifestations of COVID-19: a systematic review and current update. Acta Neurologica Scandinavica. 2020 Jul;142(1):14-22.
4. Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory coronaviruses. Journal of virology. 2000 Oct 1;74(19):8913-21.
5. Garg RK, Paliwal VK, Gupta A. Spinal cord involvement in COVID-19: a review. The Journal of Spinal Cord Medicine. 2021 Mar 12:1-5.
6. Canoglu K, Saylan B. Therapeutic dosing of low-molecular-weight heparin may decrease mortality in patients with severe COVID-19 infection. Annals of Saudi medicine. 2020 Nov;40(6):462-8.
7. Mondal R, Deb S, Shome G, Ganguly U, Lahiri D, Benito-Leon J. COVID-19 and emerging spinal cord complications: a systematic review. Multiple sclerosis and related disorders. 2021 Jun 1;51:102917.
8. Chow CC, Magnussen J, Ip J, Su Y. Acute transverse myelitis in COVID-19 infection. BMJ Case Reports CP. 2020 Aug 1;13(8):e236720.
9. Castro RA, Frishman WH. Thrombotic complications of COVID-19 infection: a review. Cardiology in review. 2021 Jan 1;29(1):43-7.
10. Avila J, Long B, Holladay D, Gottlieb M. Thrombotic complications of COVID-19. The American Journal of Emergency Medicine. 2021 Jan 1;39:213-8.
11. Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JC, Fogerty AE, Waheed A, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020 Jul 23;136(4):489-500.
12. Pavlov V, Beylerli O, Gareev I, Torres Solis LF, Solis Herrera A, Aliev G. COVID-19-related intracerebral hemorrhage. Frontiers in Aging Neuroscience. 2020 Oct 22;12:600172.
13. Boira I, Esteban V, Vañes S, Castelló C, Celis C, Chiner E, et al. Major bleeding complications in COVID-19 patients. Cureus. 2021 Aug 1;13(8).