Abstract
Background and aims: Use of platelet-rich plasma (PRP) is well established in treatment of orthopedic patients. This pilot study aims to determine the efficacy of using instillation of PRP paired with hydrodistention of the bladder to treat patients with interstitial cystitis (IC).
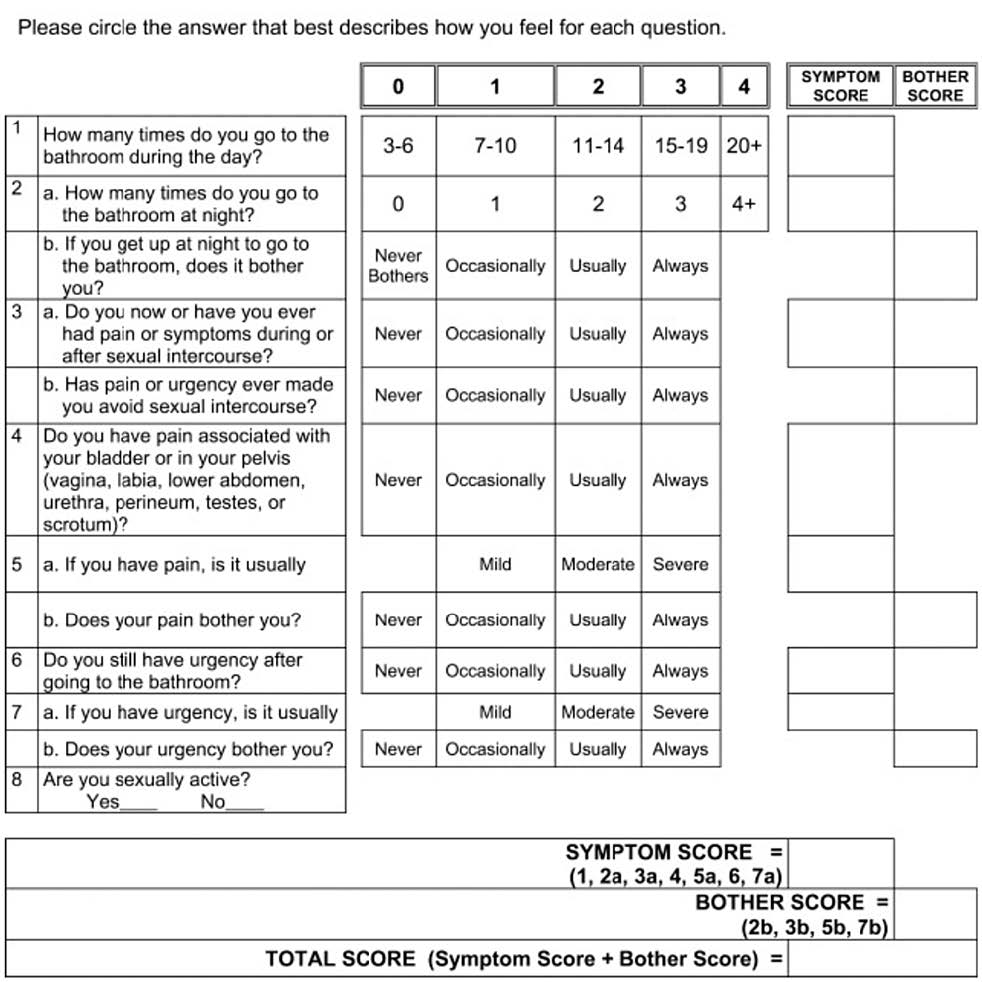
Methods: Patients with a diagnosis of interstitial cystitis were recruited to this study. Patients completed Pelvic Pain and Urgency/Frequency (PUF) patient symptom scale, which quantified a symptom and bother score. Patients were treated with hydrodistention with instillation of PRP. Patients completed the PUF questionnaire weekly for six weeks following treatment.
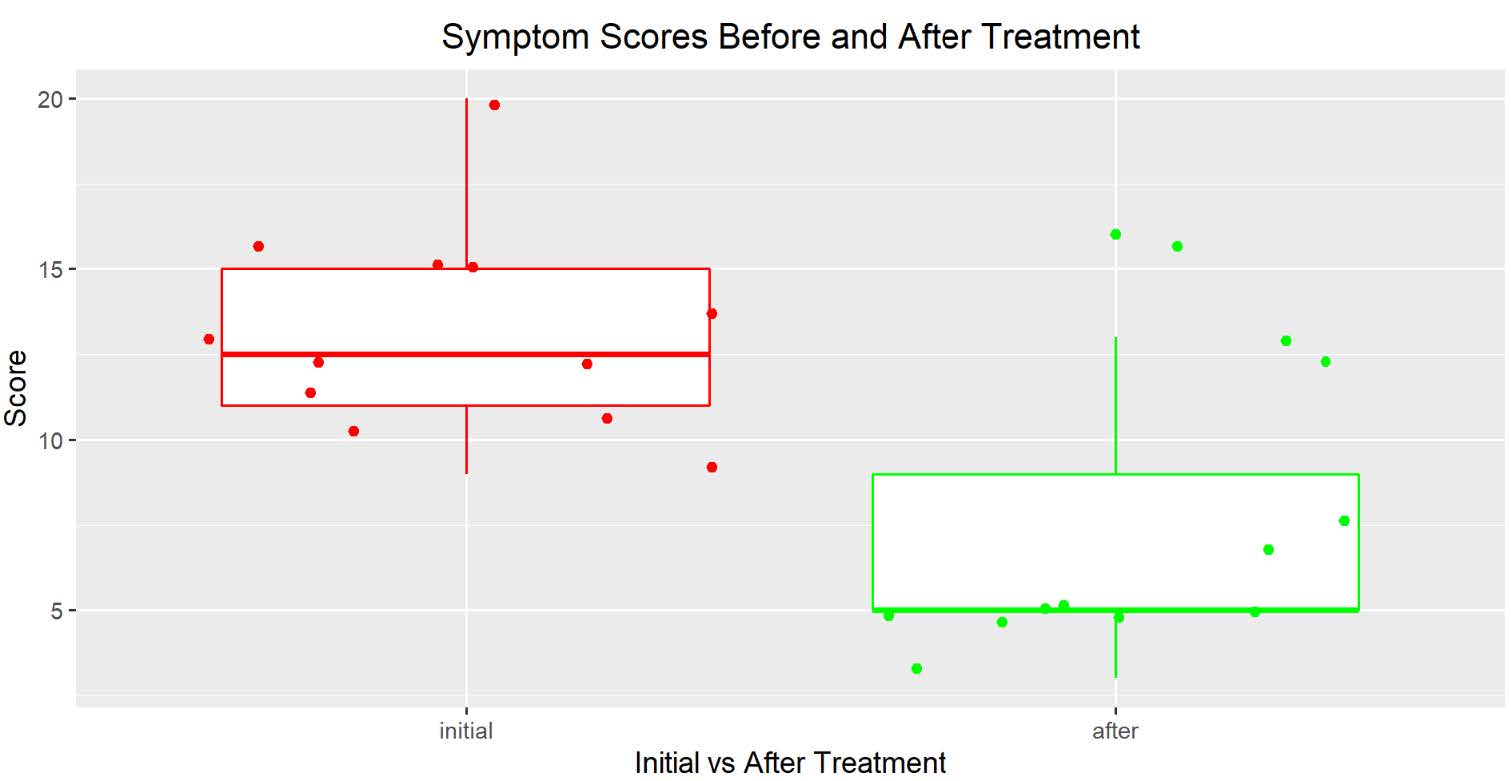
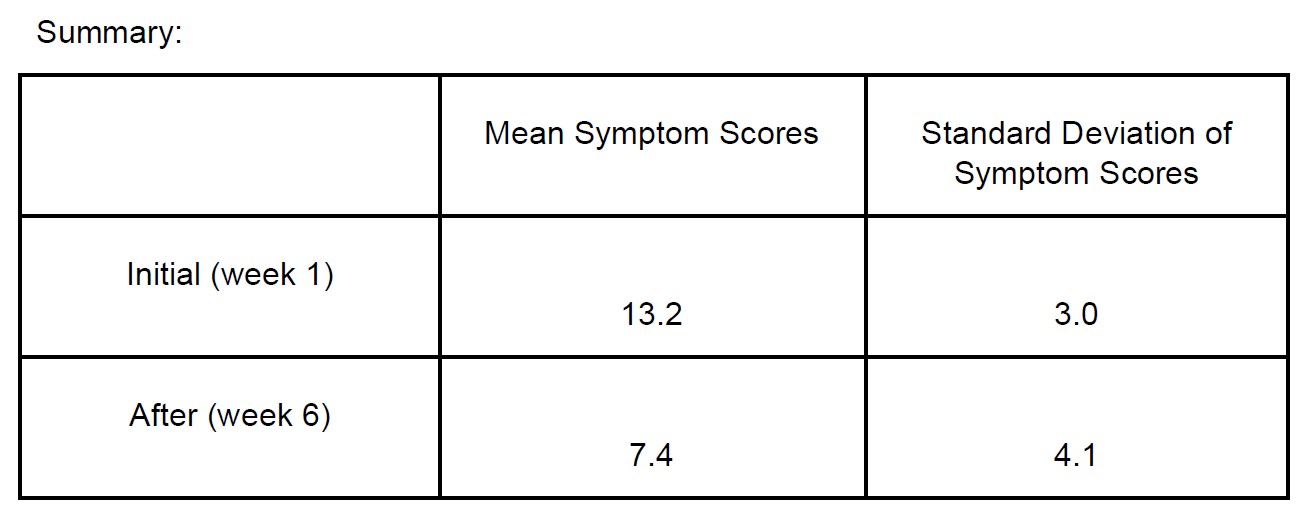
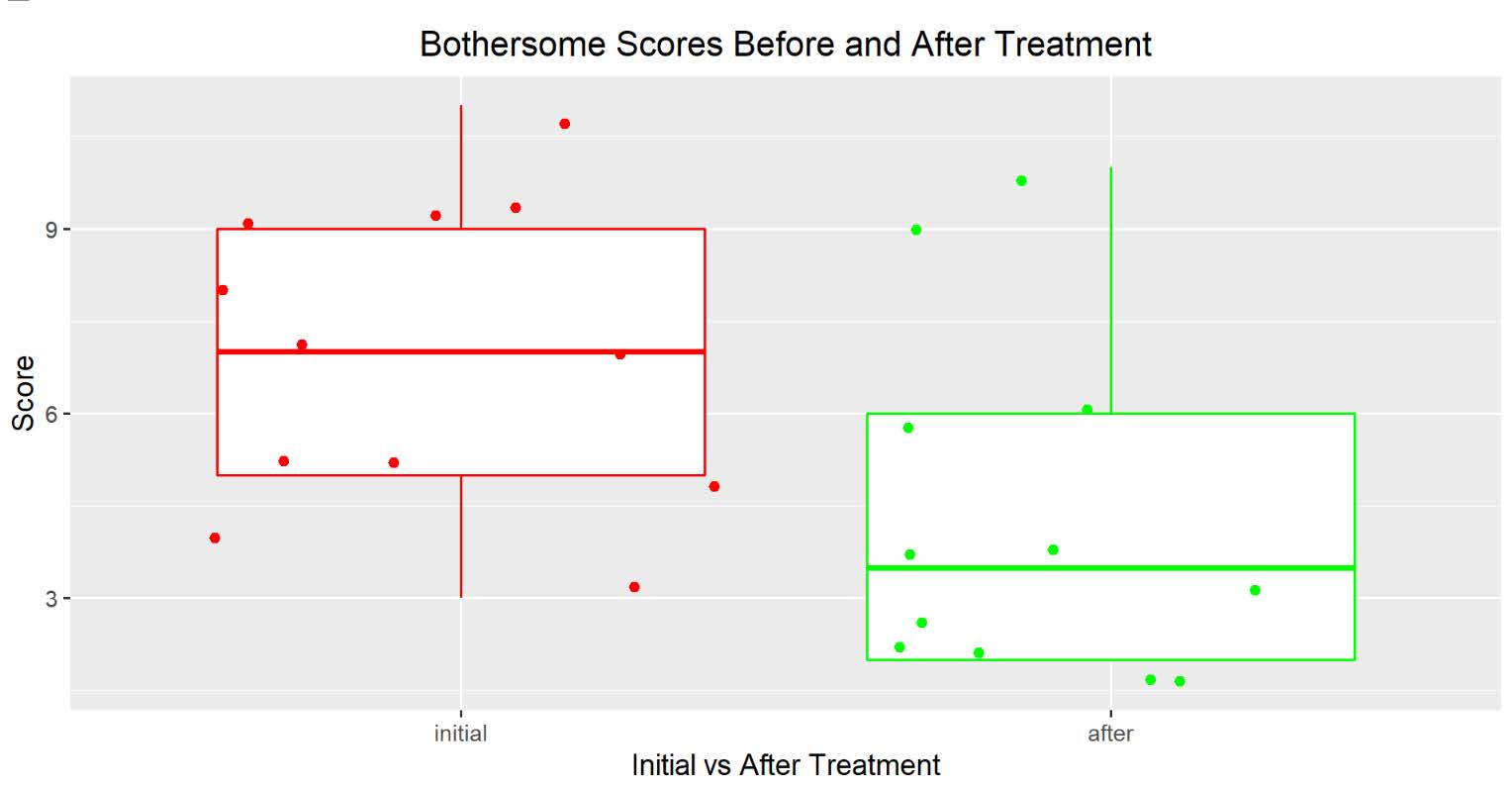
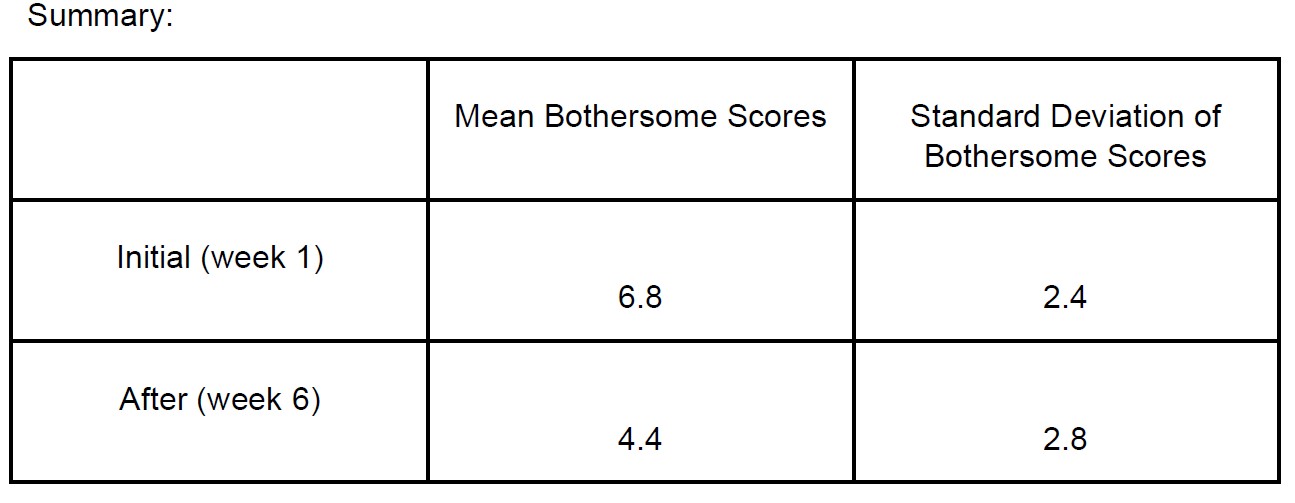
Results: 12 patients underwent hydrodistention with instillation of PRP. The patients were all women, ranging in age from 23 to 71. The mean symptom score went from 13.167 to 7.417 and the mean bother score decreased from 6.833 to 4.41, showing a statistically significant reduction in symptom and bother scores.
Conclusions: Hydrodistention with instillation of PRP is an effective treatment of interstitial cystitis.
Keywords
Interstitial cystitis, Platelet-rich plasma, Hydrodistention, Chronic pelvic pain, Urinary incontinence, Painful bladder syndrome, Nocturia
Introduction
Interstitial cystitis (IC) is a bladder disorder with unknown etiology [1]. The most commonly accepted theory is that a defect in the glycosaminoglycan layer of the bladder urothelium allows solutes in the urine to penetrate through the urothelium into the bladder interstitium which causes an inflammatory reaction [1]. This theory is supported by a study which shows increased absorption of lactulose into the bloodstream of patients who have interstitial cystitis compared to controls [2]. A previously published study showed that platelet-rich plasma (PRP) was an effective therapy for interstitial cystitis when injected in multiple areas of the bladder transurethrally with cystoscopic guidance [3]. In accordance with the University of Virginia Ethical Principles for the Protection of Human Subjects of Biomedical Behavioral Research we adhered to the three principles underlying the ethical conduct of research: respect for persons, beneficence, and justice. Consent was obtained from all participants.
Materials & Methods
12 patients with a diagnosis of interstitial cystitis for over one year were recruited to this study. The patients signed informed consents which discussed the risks of the procedure, including the unknown risk of a new procedure and the novel nature of the procedure that was not FDA-approved. Patients were also made aware of similar studies performed in the field of orthopedics. The patients were recruited from a private practice. All patients were women, ranging in age from 23 to 71. All patients had cystoscopy performed which confirmed no foreign bodies or signs of malignancy or abnormalities not associated with interstitial cystitis—such as glomerulations, squamous metaplasia of the trigone, and urethral erythema. The patients had previous unsuccessful treatments with usual interstitial cystitis care, including avoidance of bladder irritants, treatment of comorbid conditions, including anxiety, depression, fibromyalgia, and endometriosis, and use of medications, including amitriptyline, pentosan polysulfate sodium, phenazopyridine, and methenamine. During preoperative appointment patients filled out a Pelvic Pain and Urgency/Frequency (PUF) patient symptom scale (Figure 1) [4].
Figure 1. PUF Questionnaire.
All patients in the study underwent hydrodistention of the bladder with intravesical instillation of PRP with anesthesia. 50 ml of peripheral blood was drawn prior to the procedure and separated using centrifugation to obtain the platelet-rich plasma. Under general anesthesia the bladder was distended to a maximum cystometric capacity, which ranged from 200 ml to 750 ml, using a pressure of 80 cm of water. The bladder was distended for three minutes and then drained with the cystoscopic sheath. Then 20 ml of platelet-rich plasma was instilled into the bladder using the cystoscopic sheath and was flushed with 10 ml of saline. The sheath was then removed. The patient was instructed to not void for two hours. The patient was recommended to continue with usual IC care, including avoiding dietary bladder irritants. All patients filled out Pelvic Pain and Urgency/Frequency patient symptom questionnaires weekly for six weeks after the procedure. A historical control was compared from a previous usual care treatment of hydrodistention in a one to three ratio.
Results
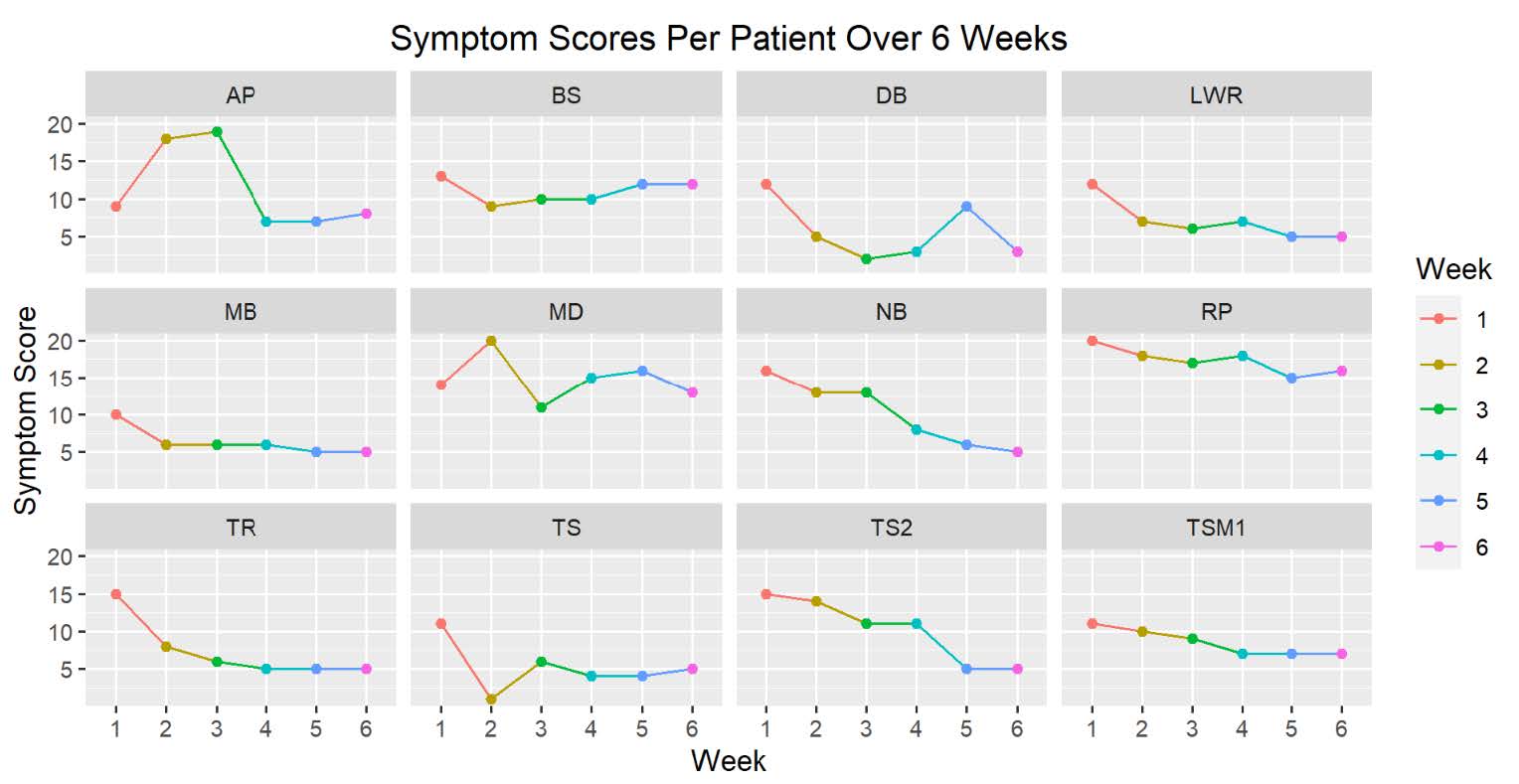
A total of 12 women between the ages of 23 and 71 completed the PUF questionnaires weekly for 6 weeks. The responses were analyzed and showed a statistically significant improvement in the symptom and bother scores from their preoperative responses to the six-week post-procedure responses. Symptom scores before and six weeks after treatment were statistically significant with the average symptom score of 12 before treatment and average symptom score of 5 after treatment, showing with paired t-tests a P-value of 0.001101 (Figure 2).
Figure 2. Symptom scores before and after treatment.
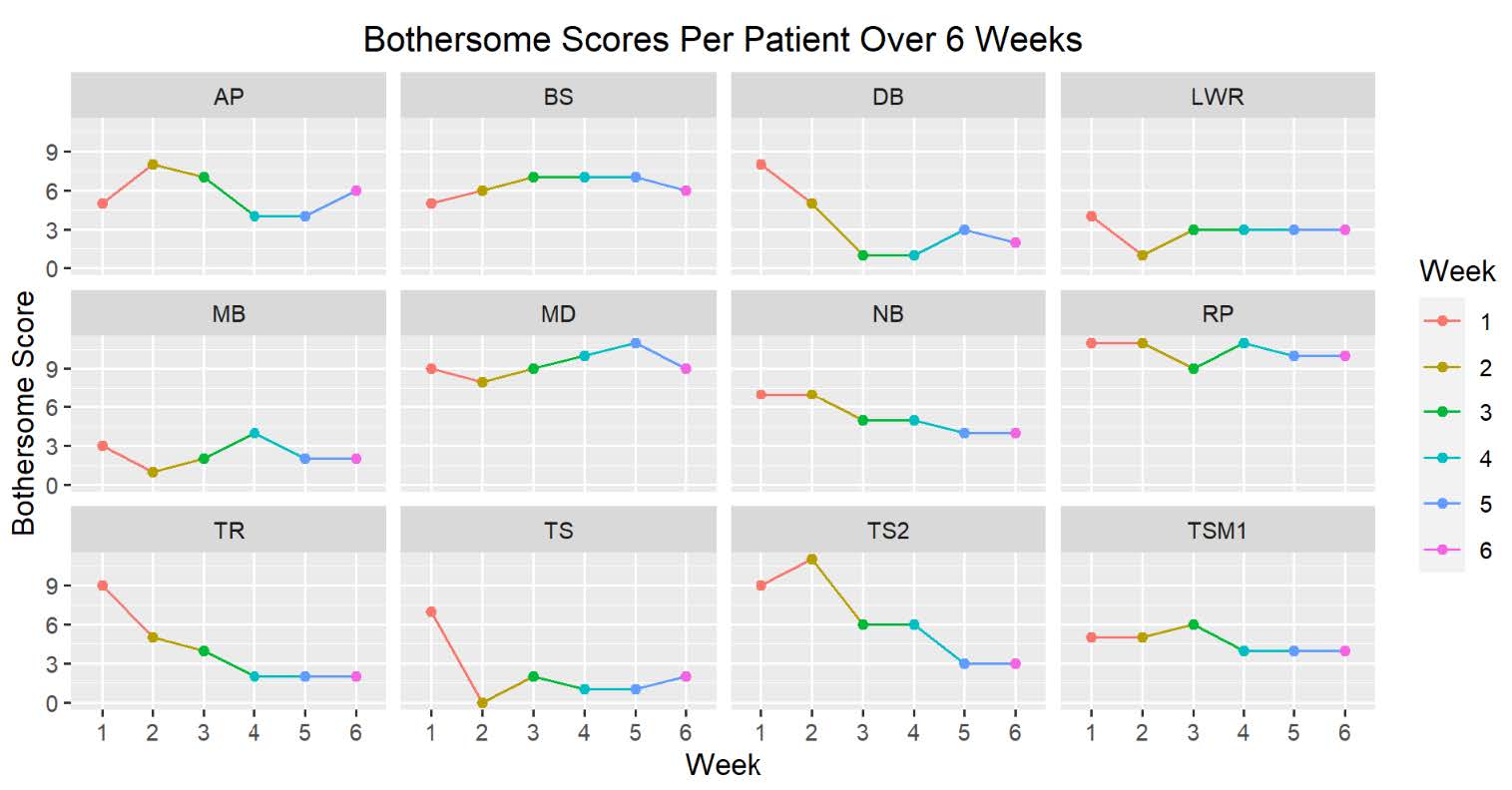
There was also convincing statistical evidence to conclude that the treatment is effective in reducing patients’ bothersome score after six weeks, with a P-value of 0.007 (Figure 3).
Figure 3. Bothersome scores before and after treatment.
Figures 4 and 5 demonstrates the change in symptom and bother scores over the six-week study period. Individual patients experienced improvement in symptom and bother scores. Of note the patient labeled MD was not able to comply with the posttreatment course of avoiding alcohol.
Figure 4. Symptom scores per patient over 6 weeks.
Figure 5. Bothersome scores per patient over 6 weeks.
Discussion
The treatment of 12 patients with longstanding interstitial cystitis with hydrodistention with instillation of platelet-rich plasma shows statistically significant evidence of efficacy in relieving symptoms of IC over a six week course. The previously published case study by the author suggested people who have anxiety or high stress are in a constant “fight or flight” mode which prevents adequate perfusion of the bladder and decreases growth factors [5]. This deferred maintenance could be the etiology of the defect in the glycosaminoglycan layer of the urothelium in patients with IC. This therapy is supported by articles in the medical literature which shows the role of serotonin in the function of the gastrointestinal and genitourinary organ systems. High levels of stress decreases serotonin in the central nervous system and in the peripheral nervous system [6]. With increased stress, blood flow is diverted away from organs such as the bladder. Women who have anxiety or high stress and low levels of serotonin perceive the pain as more intense [6]. Intravesical instillation of platelet-rich plasma provides growth factors to the urothelium and encourages healing and repair of the defects in the umbrella cells of the urothelium and the glycosaminoglycan layer. Once the layer is repaired and barrier integrity is restored, the inflammation decreases and the pain decreases. The procedure is done by first performing hydrodistention, which many times leads to terminal hematuria from the defective urothelium. The bladder is then drained, and the platelet-rich plasma is instilled in the bladder. After the procedure is performed, the patients are instructed to avoid bladder irritants strictly for two weeks to encourage complete healing of the urothelium.
In previous studies hydrodistention showed that stretching of the bladder increased urinary heparin-binding epidermal growth factor and reduced antiproliferative factor in patients with interstitial cystitis [7]. Normal bladder stretch of detrusor smooth muscle cells is known to stimulate heparin-binding epidermal growth factor. However, an antiproliferative factor in patients with IC inhibits urothelial proliferation. Patients with IC also have decreased levels of heparin-binding epidermal growth factor [8].
Unfortunately, this procedure is not permanent. It has been shown to be effective in some patients for up to one year. This initial study requires further study and, eventually, a randomized control study comparing a control group to a treatment group receiving hydrodistention with PRP.
Conclusions
This pilot study concludes that hydrodistention with intravesical instillation of PRP is an effective treatment for female patients with longstanding interstitial cystitis symptoms. Randomized controlled study is needed to confirm these initial findings.
Conflict of Interest
The author has no conflicts of interest.
Funding
There has been no funding for this investigation.
Acknowledgements
The author would like to thank Prince Afriyie, Ph.D. for conducting statistical analysis.
References
2. Erickson DR, Herb N, Ordille S, Harmon N, Bhavanandan VP. A new direct test of bladder permeability. The Journal of Urology. 2000 Aug 1;164(2):419-22.
3. Jiang YH, Kuo YC, Jhang JF, Lee CL, Hsu YH, Ho HC, et al. Repeated intravesical injections of platelet-rich plasma improve symptoms and alter urinary functional proteins in patients with refractory interstitial cystitis. Scientific Reports. 2020 Sep 16;10(1): 15218.
4. Parsons CL, Dell J, Stanford EJ, Bullen M, Kahn BS, Waxell T, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002 Oct 1;60(4):573-8.
5. Hardy TJ. Interstitial Cystitis Can Be Improved with Intravesical Instillation of Platelet-Rich Plasma. Cureus. 2022 Mar 1;14(3):e22747.
6. Carhart-Harris RL, Nutt DJ. Serotonin and brain function: a tale of two receptors. Journal of Psychopharmacology. 2017 Sep;31(9):1091-120.
7. CHAI TC, ZHANG CO, SHOENFELT JL, JOHNSON HW, WARREN JW, KEAY S. Bladder stretch alters urinary heparin-binding epidermal growth factor and antiproliferative factor in patients with interstitial cystitis. The Journal of Urology. 2000 May;163(5):1440-4.
8. Kim J, Freeman MR. Antiproliferative factor signaling and interstitial cystitis/painful bladder syndrome. International Neurourology Journal. 2011 Dec;15(4):184-91.