Abstract
A 24-year-old professional soccer player sustained a rare distal biceps femoris avulsion injury during a training session, characterized by a near-complete tear at the musculotendinous junction approximately 5 cm proximal to the fibular head, without tendon detachment or significant retraction. Given the unusual nature of this injury and the absence of tendon retraction or involvement of lateral stabilizing structures, a conservative, nonoperative treatment approach was adopted. The patient underwent a carefully structured, four-phase rehabilitation protocol spanning 12 weeks, focusing sequentially on pain control and protection, gradual introduction of eccentric strengthening, neuromuscular re-education, and finally sport-specific functional training. Serial imaging, including MRI at six weeks, confirmed progressive tendon healing and resolution of intramuscular edema, validating safe progression through rehabilitation phases.
Despite the general inclination towards surgical intervention in distal biceps femoris avulsion injuries, especially in elite athletes, this case highlights successful full functional recovery and return to competitive play without surgery. The rehabilitation program emphasized tailored progression based on clinical milestones, strength assessments, and imaging findings. Key elements included initial isometric strengthening, controlled eccentric loading, and prevention strategies targeting flexibility, core stability, and load management to mitigate recurrence risk. Moreover, the patient's history of a prior contralateral hamstring injury led to genetic evaluation, which was unremarkable, underscoring the importance of individualized assessment.
This case contributes valuable evidence supporting the viability of nonoperative management in select distal biceps femoris avulsion injuries, particularly when surgical indications such as greater than 2 cm tendon retraction or multi-ligamentous instability are absent. The detailed four-phase rehabilitation protocol outlined here offers a practical framework for clinicians managing similar presentations, balancing tissue healing with progressive functional demands. Ultimately, individualized treatment decisions incorporating clinical, imaging, and patient-specific factors are paramount to optimizing outcomes in this rare but challenging injury.
Keywords
Muscle and joint injuries, Occupational medicine, Trauma and rehabilitation
Introduction
The hamstrings are one of the most commonly injured groups of muscles in athletes, from the recreational to the professional level [1]. Ranging from ruptures to more chronic low-grade tears, these injuries can not only cause prolonged absence from the athlete’s sport but also come at a high risk of recurrence [1]. Of the hamstring muscles, the biceps femoris is the most commonly injured and accounts for 57–87% of all hamstring injuries [2–4], likely due to the fact that it produces more powerful eccentric contraction as compared to the semimembranosus or semitendinosus [5], producing up to 75% of flexion strength at the knee [6].
While the most commonly affected portion of the muscle is the proximal or distal musculotendinous junction, avulsion injuries are rare, with distal avulsion injuries in particular accounting for 2% of all hamstring injuries [4,7,8]. The biceps femoris consists of a long head, arising from the superomedial portion of the ischial tuberosity, and a short head that arises from the lateral lip of the linea aspera of the posterior femur. Both heads insert onto the fibular head along with the lateral collateral ligament and popliteofibular ligament as part of the posterolateral corner (PLC) [4].
Injuries to the proximal hamstrings are more commonly reported and hence our current knowledge of its management is more accurate, as indicated by the strong body of evidence suggesting that its management should consist of surgical intervention over non-operative treatment [9]. However, avulsions of the distal biceps are much rarer, and hence guidelines on management are not as concrete [4,8]. Few cases have been reported of isolated biceps femoris avulsion fractures [8] and to our knowledge, this is the first reported case of such injury in a professional soccer player that was ultimately managed with conservative therapy.
The purpose of this case report is to grow our currently very limited knowledge of the management of distal biceps femoris avulsion fractures so that it may guide future health professionals in the management of this rare injury.
Case Presentation
A 24-year-old male professional soccer player presented to our sports medicine clinic with acute left posterior knee pain. The injury occurred during team practice while attempting to trap a soccer ball in stride, at which point the patient experienced a sudden "pop" in the posterolateral aspect of the left knee. He was unable to complete the session and noted increasing discomfort with weight-bearing. He denied any sensation of instability or prior trauma to the knee. The player was immediately evaluated, with an MRI performed the same day. On physical examination, he was noted to have a palpable defect at the expected attachment site of the biceps femoris tendon with associated tenderness. There was edema, but no appreciable bruising likely due to the patient’s darker skin tone. Inspection of the posterior knee revealed mild swelling localized to the posterolateral region. The initial phase of rehabilitation, focusing on edema and pain control, was initiated the day following the injury. The patient ambulated with an antalgic gait and a shortened stance phase on the affected side. Palpation elicited tenderness over the distal biceps femoris tendon, and a palpable defect was noted without a clear tendon outline. Strength testing demonstrated 4/5 weakness with resisted knee flexion, while ligamentous testing of the lateral collateral ligament and other posterolateral structures was normal. There were no neurological deficits.
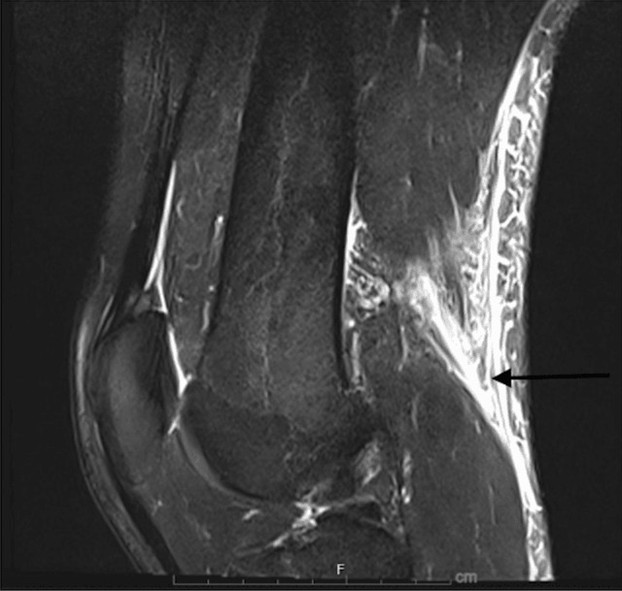
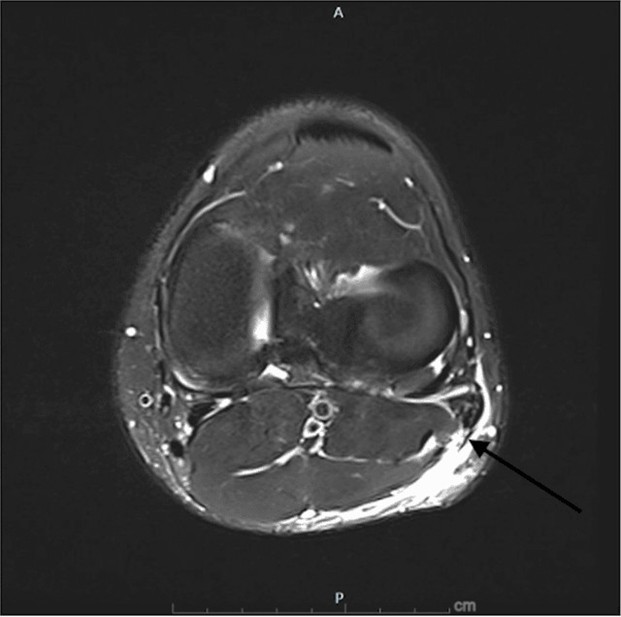
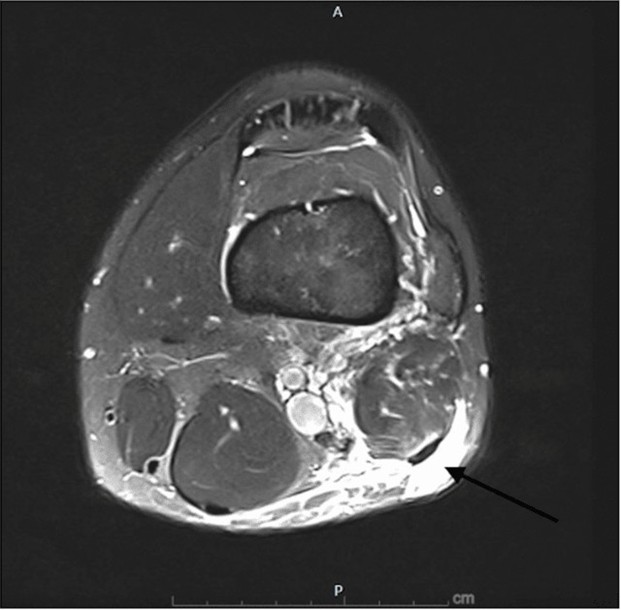
Given the clinical findings, an MRI of the left knee was obtained the same day, shown in Figures 1-3. Imaging revealed a near-complete tear of the distal biceps femoris tendon at the musculotendinous junction, approximately 5 cm proximal to its fibular insertion. Importantly, the tendon remained in continuity with the fibular head, with no frank avulsion. The lateral collateral ligament and posterolateral corner structures appeared intact [7].
Figure 1. MRI (sagittal view) of initial injury. The black arrow is pointing to musculotendinous disruption with some retraction of the distal biceps femoris tendon with overlying edema.
Figure 2. MRI (axial view) of initial injury. The arrow is pointing to edema within the tendon sheath, signifying a high-grade/complete tear of the distal biceps femoris tendon.
Figure 3. MRI (axial view) of initial injury. Edema within the distal biceps femoris.
After consultation with the team’s orthopedic surgeon, a nonoperative treatment plan was initiated due to the absence of tendon retraction and the integrity of surrounding stabilizing structures. The decision to pursue conservative care was also influenced by the patient’s preference and favorable prognostic indicators, including high baseline fitness and early presentation. The rehabilitation process began the next day for the patient and focused on three phases that required 12 weeks to complete.
During the initial three weeks (Phase 1), the rehabilitation focused on symptom control, edema reduction, and prevention of muscle atrophy. Isometric exercises were implemented, and range of motion was cautiously preserved. Passive modalities and protective strategies were emphasized to avoid overstressing the healing tissue. No eccentric or stretching movements were allowed at this stage [10].
Six weeks after the injury, a repeat MRI showed tendon fiber abutment and decreased intramuscular edema. The imaging files from this follow-up MRI were not made available to our team, and only the radiology report was accessible; therefore, we did not include images for comparison in this manuscript. With improved pain control and normalized gait, Phase 2 introduced gentle eccentric training and treadmill walking. Progression was based on achieving pain-free ambulation and controlled resistance exercises [10].
In weeks 7-9 (Phase 3), the athlete began high-intensity treadmill running, lateral band walks, Nordic hamstring exercises, and neuromuscular re-education of the trunk and pelvis. By week 10, he had achieved >80% strength compared to the contralateral limb and was advanced to Phase 4, which included sport-specific drills and maximal eccentric loading [10].
By week 12, the athlete returned to full team participation without symptoms. Notably, this was his second distal biceps femoris injury-the first occurred on the contralateral side during the previous season. Due to the unusual recurrence, he was referred for genetic evaluation to rule out connective tissue disorders, which was unremarkable. His long, lean body habitus was considered a possible contributing factor.
To support healing and ensure a safe return to sport, a structured four-phase rehabilitation protocol was implemented, with specific attention to symptoms and edema control in the early phase. Passive modalities such as cryotherapy (15–20 minutes, three times daily), intermittent compression, and transcutaneous electrical nerve stimulation (TENS) were used during the first two weeks to manage pain and swelling. Elevation and the use of compression sleeves were also applied consistently during off-loading.
In addition to describing the phased progression within the main text, the intervention plan is summarized in Table 1, which provides detailed guidance for clinical replication.
|
Phase |
Weeks |
Goals |
Intervention Strategies |
Passive Modalities |
|
Phase 1 Acute Phase |
Weeks 0–3 |
- Pain and edema control - Protect healing tissue - Maintain ROM |
- Partial weight-bearing - Isometric quadriceps and hamstring activation - Gentle passive range of motion (PROM) - No stretching or eccentric loading |
- Cryotherapy - TENS - Compression sleeves - Elevation |
|
Phase 2 Subacute |
Weeks 4–6 |
- Restore gait and ROM - Begin eccentric loading |
- Treadmill walking - Gentle eccentric hamstring curls - Hip/glute strengthening |
- Moist heat pre-exercise |
|
Phase 3 Strengthening |
Weeks 7–9 |
- Regain strength and neuromuscular control |
- Nordic hamstring exercises - Lateral band walks - Trunk/pelvis control work |
- None routinely used |
|
Phase 4 Return to Sport |
Weeks 10–12 |
- Sport-specific reconditioning |
- Maximal eccentric loading - Plyometric drills - Sport-specific training |
- None routinely used |
Discussion
The prevalence of avulsion injuries has increased due to the continued rise of athletes participating in dynamic sports, such as soccer, track and field, and football [11]. Avulsion injuries usually occur when either a ligament or soft tissue attachment to a bone is separated from the main bone attachment and is allowed to surpass the maximum stress amount that is typically seen [11]. These injuries are seen in both children and adults, but more commonly in adults with inadequate growth zones during bone development [11]. The most common injury site for an avulsion injury is the hamstring, which is composed of three muscles known as the biceps femoris, semitendinosus, and semimembranosus [11]. Treating avulsion injuries is typically indicative of instability in the injured area, and treatment should be assessed based on a patient’s individual needs [11].
Distal avulsion injuries are associated with injuries that involve multiple ligaments at the posterolateral corner (PLC) of the knee being damaged [8]. When a person is diagnosed with a distal avulsion injury, multiple ligaments are suspected to be damaged due to the amount of stress experienced during the injury [8]. These injuries are sometimes overlooked or misdiagnosed due to their anatomical location. Differential diagnoses include reactive bone lesions, tendonitis, muscle strains or tendon tears, simple dislocations, and apophysitis [11].
Individuals who experience a biceps femoris avulsion fracture can be treated either nonoperatively or operatively. To confirm diagnosis, orthopedic provocation tests must be performed: Puranen-Orava Test, Bent-knee stretch test, modified bent-knee stretch test. If tests present positive, the next course of action involves immobilization for pain relief and an MRI to assess injury severity. Surgical repair is typically indicated when there is avulsion of two tendons or retraction greater than 2 cm [7]. Conservative management includes rest, ice, anti-inflammatories, and progressive strengthening over 4-6 weeks [11]. Platelet-rich plasma (PRP) injections may be used to accelerate healing and reduce scar tissue formation [7].
According to Ernlund et al., injuries can be graded using a 0-4 system with letter suffixes indicating location: a = myofascial, b = musculotendinous, c = intra-tendinous (Table 2) [12]. A Grade 4C injury-defined as a complete intra-tendinous tear with >2 cm of retraction-warrants surgery, while lesser grades may be managed conservatively [7]. Knapik et al. reported that among 22 professional athletes who underwent surgical repair for distal biceps femoris avulsion, return to sport occurred at an average of 3.8 ± 2 months [7].
|
GRADE |
DESCRIPTION |
MRI IMAGING (Day 2)* |
|
0a |
Focal area of muscle pain usually following exercise |
MRI normal |
|
0b |
Generalized muscle pain following unaccustomed exercise |
MRI normal or patchy high signal change throughout one or more muscles. |
|
GRADE |
DESCRIPTION |
MRI IMAGING |
|
1a |
Small Myofascial tear |
High signal change evident at the fascial border with less than 10% extension into muscle belly Cranio-caudal distance of <5 cm. |
|
1b |
Small Muscle Tendon junction tear |
High signal change of less than 10% cross sectional area of muscle at the MTJ High signal change of cranio-caudal length <5 cm (may note fiber disruption of <1 cm) |
|
GRADE |
DESCRIPTION |
MRI IMAGING |
|
2a |
Moderate Myofaseial tear |
High signal change evident at fascial border with extension into the muscle High signal change cross sectional area of between 10% and 50% at maximal site High signal change of cranio-caudal length >5 cm and <15 cm Architectural fiber disruption usually noted over less than 5 cm |
|
2b |
Moderate Muscle Tendon Junction Tear |
High signal change evident at the MTJ High signal change cross sectional area of between 10% and 50% at maximal site High signal change of cranio-caudal length >5 cm and <15 cm Architectural fiber disruption usually noted over less than 5 cm |
|
2c |
Moderate sired Intra-Tendinous Tear |
High signal change extends into the tendon with longitudinal length of tendon involvement <5 cm Cross sectional area of tendon involvement <50% of tendon cross sectional area No loss of tension or discontinuity within the tendon. |
|
GRADE |
DESCRIPTION |
MRI IMAGING |
|
3a |
Extensive Myofascial tear |
High signal change evident at fascial border with extension into the muscle High signal change cross sectional area of greater than 50% at maximal site High signal change of cranio-caudal length of greater than 15 cm Architectural fiber disruption usually noted over more than 5 cm |
|
3b |
Extensive Muscle Tendon junction tear |
High signal change cross sectional area of greater than 50% at maximal site High signal change of cranio-caudal length of greater than 15 cm Architectural fibre disruption usually noted over more than 5 cm |
|
3c |
Extensive Intra-Tendinous Tear |
High signal change extends into the tendon Longitudinal length of tendon involvement >5 cm Cross sectional area of tendon involvement >50% of tendon cross sectional area There may be loss of tendon tension although no discontinuity is evident |
|
GRADE |
DESCRIPTION |
MRI IMAGING |
|
4 |
Full thickness tear of muscle |
Complete discontinuity of the muscle with retraction |
|
4c |
Full thickness tear of tendon |
Complete discontinuity of the tendon with retraction |
In this case, a non-surgical approach was used due to the patient not meeting surgical criteria, being classified as a grade 3 injury. Conservative treatment involved a 4-phase rehabilitation protocol with eccentric training and PRP to support tissue healing [7,10]. Initial goals included symptom control and prevention of atrophy. Once pain-free ambulation was achieved, the focus shifted to regaining strength and neuromuscular control using exercises such as Nordic hamstring curls and lateral band walks [10]. The final phase emphasized functional drills and eccentric loading in a lengthened state.
Progress was monitored with flexibility assessments such as the H-test and passive hamstring stretch with contralateral hip flexion. Full recovery was achieved in 12 weeks with no residual symptoms. Patient education on injury prevention-through stretching, strengthening, adequate rest, and activity modification- was emphasized to reduce recurrence risk. Although genetic testing was performed to evaluate an underlying connective tissue disorder, the specific test name and detailed results were not available to our team. This represents a limitation of our case evaluation, as such information could have provided additional context for the recurrence risk and potential predisposition to bilateral hamstring injuries.
Conclusions
We report the case of successful nonoperative management of a distal biceps femoris avulsion fracture in this professional soccer player, which highlights the potential efficacy of conservative treatment for this rare injury. Although surgical intervention is often recommended for proximal hamstring injuries and severe distal avulsions, our case demonstrates that a structured, phase-based rehabilitation protocol can lead to a complete return to sport without the need for surgery in cases where the tear is incomplete. It is important to note that the management approach must be catered to each patient as an individual, since they may present with varying degrees of injury and inherent rates of healing. We realize that the approach we adopted for a professional athlete, such as our patient, may look very different than a weekend warrior working a full-time job. Nonetheless, we present a 4-phase approach with careful progression through pain-free movement, isometric and concentric exercises, followed by the introduction of eccentric strengthening, allowing for effective healing and restoration of function. The timeline and progression through these 4 phases can be modified as appropriate, as long as the patient meets the criteria for progression to the next stage. Additionally, the use of imaging to guide the rehabilitation process was instrumental in ensuring appropriate tendon recovery before advancing to more demanding activities.
References
2. Thompson JW, Plastow R, Kayani B, Moriarty P, Asokan A, Haddad FS. Surgical Repair of Distal Biceps Femoris Avulsion Injuries in Professional Athletes. Orthop J Sports Med. 2021 Mar 26;9(3):2325967121999643.
3. Brunet ME, Kester MA, Cook SD, Leinhardt TM, Haddad RJ Jr. Biomechanical evaluation of superficial transfer of the biceps femoris tendon. Am J Sports Med. 1987 Mar-Apr;15(2):103–10.
4. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007 Feb;35(2):197–206.
5. Dolman B, Verrall G, Reid I. Physical principles demonstrate that the biceps femoris muscle relative to the other hamstring muscles exerts the most force: implications for hamstring muscle strain injuries. Muscles Ligaments Tendons J. 2014 Nov 17;4(3):371–7.
6. Ali K, Leland JM. Hamstring strains and tears in the athlete. Clin Sports Med. 2012 Apr;31(2):263–72.
7. Knapik DM, Metcalf KB, Voos JE. Isolated Tearing and Avulsion of the Distal Biceps Femoris Tendon During Sporting Activities: A Systematic Review. Orthop J Sports Med. 2018 Jul 3;6(7):2325967118781828.
8. Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003 Oct;32(10):582–9.
9. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007 Jun;15(6):350–5.
10. Schmitt B, Tim T, McHugh M. Hamstring injury rehabilitation and prevention of reinjury using lengthened state eccentric training: a new concept. Int J Sports Phys Ther. 2012 Jun;7(3):333–41.
11. De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am J Roentgenol. 2000 Feb;174(2):393–9.
12. Ernlund L, de Almeida Vieira L. Hamstring injuries: diagnosis and treatment options. Rev Bras Ortop (Engl Ed). 2017;52(4):373–80.