Abstract
Introduction: Intestinal intussusception in adults is quite rare, accounting for 1-5% of cases of intestinal semi-occlusion. The most frequent symptoms are nausea, vomiting and abdominal distension, as in any obstructive condition seen in the emergency room. Most cases of intestinal intussusception do not have a preoperative etiological diagnosis, due to difficulty in interpreting the radiological image.
Case presentation: Case report of a 62-year-old male patient who was admitted to the emergency room at Hospital da Cidade in Salvador- Bahia- Brazil with semi-occlusion secondary to intestinal intussusception. During a multidisciplinary discussion with the radiology team, specialized in the digestive system, a preoperative diagnosis of lipoma was possible. Patient underwent primary resection without the need for oncological standardization.
Conclusion: In this case report, it was possible, with specialized discussion, to pre-operatively diagnose lipoma as a cause of intestinal intussusception.
Keywords
Intestinal intussusception, Adults, Case report, Surgical treatment, Lipoma
Introduction
Intestinal intussusception occurs due to the invagination of the proximal segment of the intestine into the adjacent lumen of the distal segment. It is relatively common in childhood, being rare in adults with an incidence between 1-5% of cases [1,2] of which lipomas represent 25% of cases.
Clinical Case
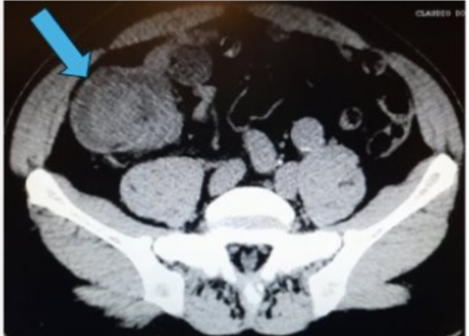
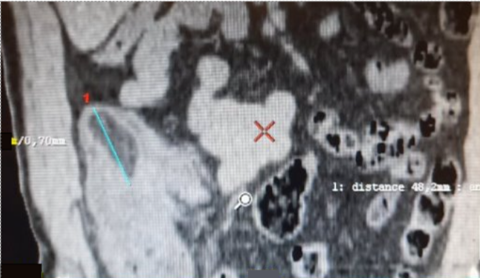
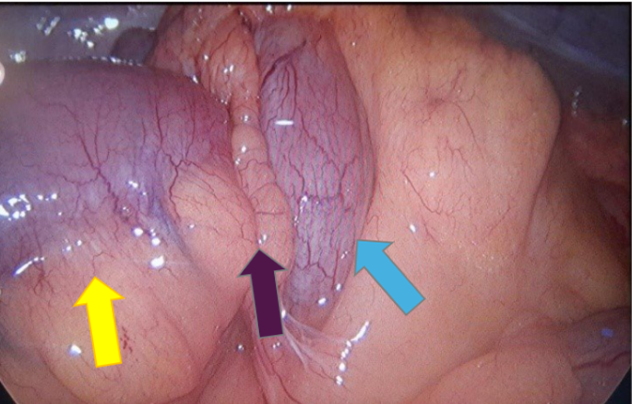
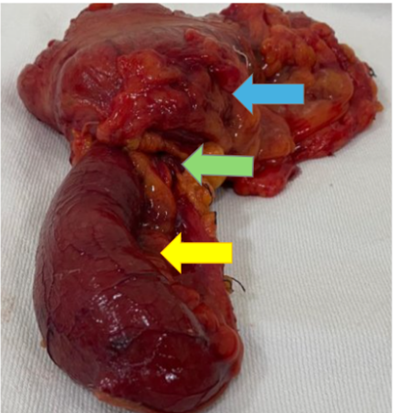
Male patient, 62 years old, overweight, hypertensive and regularly using antihypertensive medication, admitted to the digestive system surgery service at Hospital da Cidade-Salvador- Bahia- Brazil, with clinical symptoms of abdominal pain in the hypogastrium, radiating to the right iliac fossa. Report of abrupt onset, with strong intensity and no improvement after analgesia. Pacient reports passing gas and feces. On physical examination, the abdomen was globular due to a fatty panniculus, without abdominal distension, tympanic, painless on superficial and deep palpation. Surgical history: conventional appendectomy, 10 years ago. Computed tomography of the total abdomen showed a point of mechanical obstruction at the level of the distal ileum and cecum, with classic radiological signs of intestinal intussusception: pseudokidney sign (Figure 1) and target sign (Figure 2). In a multidisciplinary discussion with the radiolo team specialized in the digestive system, radiological characteristics of benign lipomatous neoplasia were highlighted: Lesion measuring 4.8 x 3.0 cm, associated with well-defined margins, rounded and with a fat density similar to that of mescolon, without prominent peri-colonic lymph node (Figure 3). The patient's clinical condition worsened due to abdominal distension and post-food vomiting, undergoing surgical treatment with resection of the distal ileum and cecum and primary anastomosis. No need for wide colectomy or retroperitoneal lymphadenectomy. The patient was discharged from hospital on the 5th postoperative day without abdominal pain, with a bland oral diet and normal intestinal rhythm. Pathological anatomy showed a benign lipomatous lesion measuring (4.5 x1.5 cm) in the ileum.
Figure 1. Telescoping between the distal ileum and cecum. Radiological sign of the pseudokidney (green arrow).
Figure 2. Ileo-colonic intussusception.Target sign (blue arrow).
Figure 3. Coronal section showing a lesion with well-defined margins, rounded and with a fat density similar to the mesocolon, measuring 4.8 cm (blue line).
Figure 4. Intraoperative photo showing intussuscepted segment (yellow arrow: distal ileum; blue arrow: cecum; purple arrow: site of intussusception).
Figure 5. Photo of the surgical specimen: (yellow arrow: distal ileum; blue arrow: cecum; green arrow: site of intussusception).
Discussion
Intestinal intussusception was first mentioned by Paul Barbbet, who described it as a telescope-shaped invagination of the proximal portion with the distal portion of the intestine. Since its description, several cases have emerged and in 1789, John Hunter coined the term after describing 3 of his patients [3]. Although the exact underlying mechanism for intussusception is not known, it is believed that any irritant factor in the mucosa or injury to the intestinal wall alters the normal peristalsis, thus culminating in intussusception [4].
Symptoms
The clinical presentation of intestinal intussusception in adults is quite variable [5], with its progression generally being chronic or subacute [6]. Abdominal pain appears as the main symptom in the literature, followed by nausea, vomiting, abdominal distension, constipation and gastrointestinal bleeding [7]. However, in up to 35% of cases, the diagnosis is made intraoperatively [1]. In a retrospective study, Honjo et al. [3] reported 44 cases of intussusception in adults, where abdominal pain was the main symptom (Table 1).
In our report, the patient presented abdominal pain as his main complaint.
|
Signs and symptoms |
Number of patients |
% of patients |
|
Abdominal pain |
24 |
54.5 |
|
Vomiting |
10 |
22.7 |
|
Diarrhea |
8 |
18.2 |
|
Nausea |
6 |
13.6 |
|
Melena |
6 |
13.6 |
|
Abdominal mass |
5 |
11.4 |
|
Abdominal distension |
4 |
9.1 |
|
Hyporexia |
3 |
6.8 |
|
Epigastralgia |
2 |
4.5 |
|
Weight Loss |
2 |
4.2 |
|
General malaise |
1 |
2.3 |
|
Respiratory discomfort |
1 |
2.3 |
|
Shock |
1 |
2.3 |
Etiology
The main etiology of intestinal intussusception in adults is malignant tumors, with adenocarcinoma representing approximately 30% of cases [8]. Benign neoplasms represent 25% of cases and 10% are idiopathic [6]. González-Carreró Sixto et al. [9] in a retrospective study, with 21 patients, showed intestinal intussusception due to malignant neoplasm in 42.8% of patients and benign in 28% of cases.
Classification
Intestinal intussusception is classified in the literature into many classifications for this condition, with the anatomical one being the most commonly described [10]. Four types of classification for intestinal intussusception are found in the literature [3]:
- Enteric type: Intussusception is limited to the small intestine (the most common type among adults) [1,6].
- Ileocolic type: the ileum passes through the ileocolic segment, but the appendix does not invaginate.
- Ileocecal type: the ileocecal portion invaginates into the ascending colon (responsible for 24-35%) [1,6].
- Colocolonic type (including colorectal): Intussusception is limited to the colon and rectum, without anal protrusion (with an incidence of 15-26%) [1,6].
In our case, we did not consider the use of this classification due to the lack of change in management in the case of intestinal intussusception.
Diagnosis
The suspicion of obstructive acute abdomen is initially made by the patient's clinic, while its etiology requires imaging tests. Abdominal radiography for diagnosing acute obstructive abdomen can offer consistent information, but it is not used for intussusception research. Abdominal ultrasound can also be used, although it is operator dependent and has complicating factors - such as distension of loops and obesity -, It can provide “target” or “sandwich” images which are signs of intussusception, and can also assess distress of loops with the use of Doppler [6]. In the literature review, no sensitivity and specificity data were found that would justify the use of abdominal ultrasound. Contrast-enhanced abdominal tomography has sensitivity that varies in the literature from 58-100% with specificity of 100% [7]. In addition to diagnosing occlusive syndrome due to intussusception, through typical images such as: “target”, “pseudorim”, “sausage” and intraluminal mesenteric vessels, abdominal tomography provides data such as mechanism, precise location and etiology. Gayer et al. [11] described 16 cases of intussusception in adults where abdominal tomography confirmed the diagnosis. And in cases of lipoma, tomographic signs of homogeneous and well-marginated masses were well associated with lipomatous origin [11]. In our case report, the exam used was abdominal tomography with contrast, which showed an intestinal image in a pseudokidney, associated with a lesion with well-defined and rounded margins (Figures 1–3).
Treatment
Surgical treatment is mandatory, Marinis et al. [8] reported, in a retrospective study, a risk of approximately 65% of malignancy in cases of intestinal intussusception in adults, with oncological surgery being performed routinely [6]. Therefore, surgeries with greater extent of resection and manipulation of the intuscepted intestine must be performed with caution, due to intraluminal and venous dissemination of the tumor, risk of perforation and dissemination to the peritoneal cavity and increased risk of anastomotic dehiscence due to friable tissue and edema of the same [8,12].
In our case, our patient underwent surgical treatment, but due to preoperative information from specialized radiology, it was possible to perform segmental enterectomy with primary anastomosis, without the need for further surgical extension including lymphadenectomy.
Conclusion
In this case report, the preoperative etiological diagnosis of intestinal intussusception in adults due to lipoma proved to be possible through multidisciplinary discussion with the radiology team, specialized in the digestive system.
References
2. Balik AA, Ozturk G, Aydinli B, Alper F, Gumus H, Yildirgan MI, et al. Intussusception in adults. Acta Chir Belg. 2006 Jul-Aug;106(4):409-12.
3. Honjo H, Mike M, Kusanagi H, Kano N. Adult Intussusception: A Retrospective Review. World J Surg. 2015;39:134-38.
4. Namikawa T, Hokimoto N, Okabayashi T, Kumon M, Kobayashi M, Hanazaki K. Adult ileoileal intussusception induced by an ileal lipoma diagnosed preoperatively: report of a case and review of the literature. Surg Today. 2012 Jul;42(7):686-92.
5. Omori H, Asahi H, Inoue Y, Irinoda T, Takahashi M, Saito K. Intussusception in adults: a 21-year experience in the university-affiliated emergency center and indication for nonoperative reduction. Dig Surg. 2003;20(5):433-9.
6. Hasnaoui H, El Bouhaddouti H, Mouaqit O, Benjelloun EB, Ousadden A, Taleb KA. Invagination intestinale aiguë révélant un lymphome T digestif chez l'adulte: à propos d'un cas [Acute intestinal intussusception revealing intestinal T-cell lymphoma in adults]. Pan Afr Med J. 2019 Jul 1;33:153. French.
7. Lu T, Chng YM. Adult intussusception. Perm J. 2015 Winter;19(1):79-81.
8. Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009 Jan 28;15(4):407-11.
9. González-Carreró Sixto C, Baleato-González S, García Palacios JD, Sánchez Bernal S, Junquera Olay S, Bravo González M, et al. Intestinal intussusception in adults: Location, causes, symptoms, and therapeutic management. Radiologia (Engl Ed). 2023 May-Jun;65(3):213-21.
10. Korkmaz O, Yilmaz HG, Taçyildiz IH, Akgün Y. Erişkinlerde invajinasyon [Intussusception in adults]. Ulus Travma Acil Cerrahi Derg. 2009 Mar;15(2):154-8.
11. Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, Hertz M. Intussusception in adults: CT diagnosis. Clin Radiol. 1998 Jan;53(1):53-7.
12. Lin MW, Chen KH, Lin HF, Chen HA, Wu JM, Huang SH. Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma. J Laparoendosc Adv Surg Tech A. 2007 Dec;17(6):789-92