Abstract
Left ventricular outflow obstruction (LVOTO) is a potential complication following surgical replacement of the aortic valve. We present an 88-year-old man who experienced periodic episodes of pre-syncope following aortic valve replacement. The underlying cause was identified as LVOTO resulting from elongated mitral valve leaflets. The diagnosis was established using stress echocardiography, which detected transient LVOTO with moderate rise in heart rate. The medical approach involved administering beta-blockers and optimising hydration consumption. The patient's symptoms and quality of life showed considerable improvement during the six-month follow-up period. Timely identification and intervention are essential in managing left ventricular outflow tract obstruction (LVOTO) after aortic valve replacement, to mitigate the risk of potential adverse cardiac events.
Keywords
Intermittent pre-syncope episodes, Left ventricular outflow obstruction, Elongated mitral valve leaflets, Aortic stenosis, Stress echocardiogram
Clinical Findings
Preoperative identification of patients with long mitral valve leaflets, basal septal hypertrophy and small left ventricle cavity might suggest a need for mitral valve repair during the same setting of aortic valve surgical replacement, as means of guaranteeing better clinical outcome and avoiding potential pre-syncope.
Abbreviations
LVOT: Left Ventricular Outflow Tract; LVOTO: Left Ventricular Outflow Tract Obstruction; AVR: Aortic Valve Replacement; BPM: Beats Per Minute; mmHg: Millimetres of Mercury
Introduction
Post-aortic valve replacement (AVR), vigilant monitoring is essential due to the potential development of LVOTO, particularly in patients with elongated mitral valve leaflets and a small left ventricle [1]. This case study highlights an 88-year-old male who experienced pre-syncope episodes post successful surgical replacement of the aortic valve, emphasising the imperative nature of early detection and prompt management to avert potential adverse complications.
Investigation
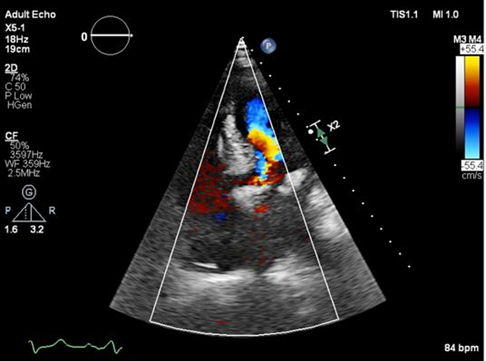
The patient manifested symptoms of pre-syncope upon abrupt postural changes and exertion, accompanied by no chest pain, dyspnea, or interference with the rest of daily activities. Resting echocardiogram findings revealed concentric left ventricular hypertrophy and calcification of the mitral annulus, and mild mitral regurgitation. The aortic valve substitute function was normal, while the mitral valve leaflets exhibited systolic anterior movement, towards the inter-ventricular septum, resulting in LVOTO as depicted in Figure 1. Left ventricular size was small for Patient’s height but systolic function was well preserved and there was mild concentric hypertrophy, but filling pressures were not raised. Patient underwent a tilt test which did not highlight any significant autonomic disturbances. Blood tests did not show any anemia, electrolytes, or kidney function abnormalities.
Figure 1. Apical 5 chamber view showing colour Doppler aliasing at the level of left ventricular outflow tract consistent with high velocity, because of anterior movement mitral valve leaflets in systole.
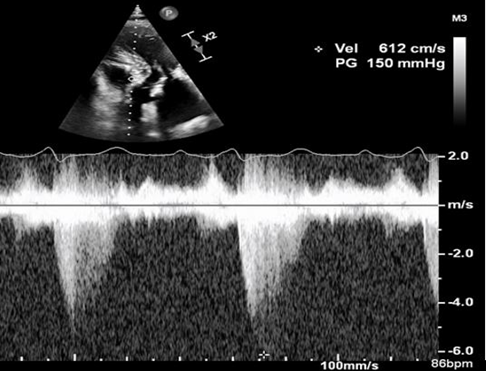
Despite preserved left ventricular dimensions and function, a stress echocardiogram employing a dobutamine infusion protocol highlighted a pronounced LVOTO caused by systolic anterior movement (SAM) of the elongated mitral leaflets when the heart rate increased by 30 bpm. LVOT pressure drop was 100 mmHg, blood pressure dropped by 30 mmHg and the patient developed shortness of breath (Figure 2). Noteworthy is the absence of symptoms of pre-syncope or lightheadedness in the recumbent position during the test, underscoring the positional influence on hemodynamics.
Figure 2. Continuous wave Doppler recording of LVOT velocities showing a pressure drop of 150 mmHg, because of the obstruction caused by systolic anterior movement of the mitral valve leaflets.
Discussion
LVOTO, frequently precipitated by the displacement of elongated mitral leaflets into the left ventricular outflow tract during systole, poses a hemodynamic impediment to blood flow [2]. This intricate interaction between prolonged mitral leaflets and hypertrophied proximal septum culminates in LVOTO, instigating an acute decline in systolic blood pressure. In this disturbed physiology, manifestations encompass symptoms such as dyspnea and light headedness, with syncope emerging in severe cases, mirroring the clinical presentation observed in aortic stenosis [3] and obstructive hypertrophic cardiomyopathy [2].
Our patient's clinical presentation and underlying pathophysiology deviated markedly from the anticipated postoperative trajectory following the successful correction of LVOTO secondary to aortic stenosis. The aetiology, distinctively rooted beneath the aortic valve level, in the left ventricular outflow tract (LVOT), precipitated blood flow obstruction with consequential symptomatic repercussions. Given the dynamic nature of the obstruction attributed to organic components, namely the combination of basal septal hypertrophy and elongated mitral leaflets, therapeutic options are circumscribed.
Beta-blockers, established for their efficacy in mitigating LVOTO and associated symptoms [4,5], proved successful in alleviating the patient's symptoms. Nevertheless, in cases where beta-blockers are intolerable, calcium channel blockers present an alternative. In instances resistant to both pharmacological approaches, our prior research underscores the potential efficacy of alcohol septal reduction in symptom management. Hence, the preoperative identification of individuals exhibiting long mitral valve leaflets, basal septal hypertrophy, and a diminutive left ventricular cavity may advocate for concurrent mitral valve repair during aortic valve replacement. This dual intervention holds promise for optimizing clinical outcomes.
Limitations
The study's focus on a single case limits its general applicability, especially given the patient's advanced age of 88 years. The exclusive exploration of beta-blockers and hydration overlooks alternative interventions for LVOTO. The influence of comorbidities on outcomes is not thoroughly examined, and the absence of a control group restricts the assessment of intervention efficacy. A more in-depth exploration of LVOTO's underlying mechanisms could enhance understanding and inform targeted interventions. Concerns about potential variability in diagnostic tools, specifically stress echocardiography, further impact the study's overall reliability and interpretation.
Ethics
The study upheld ethical standards by obtaining informed consent, ensuring participant confidentiality, and respecting autonomy. Implemented ongoing monitoring for ethical concerns and adhere to publication ethics for transparent reporting. The overarching goal is to safeguard participant well-being while contributing to scientific knowledge.
Conflict of Interest
The authors received no funding for this research and have no conflict of interest to declare.
References
2. Henein M, Arvidsson S, Pilebro B, Backman C, Mörner S, Lindqvist P. Long mitral valve leaflets determine left ventricular outflow tract obstruction during exercise in hypertrophic cardiomyopathy. International journal of cardiology. 2016 Jun 1;212:47-53.
3. Saito T, Inohara T, Yoshijima N, Yashima F, Tsuruta H, Shimizu H, et al. Small left ventricle and clinical outcomes after transcatheter aortic valve replacement. Journal of the American Heart Association. 2021 Apr 6;10(7):e019543.
4. Dybro AM, Rasmussen TB, Nielsen RR, Andersen MJ, Jensen MK, Poulsen SH. Randomized trial of metoprolol in patients with obstructive hypertrophic cardiomyopathy. Journal of the American College of Cardiology. 2021 Dec 21;78(25):2505-17.
5. Henein MY, O’Sullivan C, Sutton GC, Gibson DG, Coats AJ. Stress-induced left ventricular outflow tract obstruction: a potential cause of dyspnea in the elderly. Journal of the American College of Cardiology. 1997 Nov 1;30(5):1301-7.