Abstract
Background: Ovarian cysts are usually treated using medical or surgical interventions. However, in some cases, these treatments may not be feasible or effective, and alternative options need to be considered.
Case presentation: We report a case of a 43-year-old woman with a history of recurrent hemorrhagic ovarian cysts, who was on anticoagulant therapy due to tight mitral stenosis and had multiple autoimmune disorders. Surgical castration was not a viable option due to the bleeding risk, and intramuscular injection of analogues was not preferred. Therefore, external ovarian radiotherapy for hemostasis was planned.
Conclusion: Our case highlights that external ovarian radiotherapy can be an effective option for hemostasis in patients with bleeding ovarian cysts, especially when other treatments are contraindicated or have failed.
Keywords
Radiation therapy, Hemostatic irradiation, Ovarian cysts, Pelvic bleeding
Introduction
Pelvic bleeding, particularly gynecologic bleeding, is a common emergency in patients with neoplastic pathologies. Radiotherapy has been shown to be an important therapeutic tool in alleviating hemostatic emergencies in these cases [1].
However, the use of radiation treatment is rarely justified in cases of gynecological bleeding of benign origin, particularly in cases that are resistant to standard treatments and life-threatening.
The objective of this report is to present a case of non-neoplastic hemostatic pelvic irradiation planned in our radiotherapy department at Farhat Hached Hospital of Sousse. The literature review indicates that published studies concerning hemostatic radiotherapy are scarce in this setting. This report aims to contribute to the literature on the use of radiation therapy as a treatment option in selected cases of severe gynecological bleeding of benign origin that are refractory to standard treatments.
Case Presentation
We present the case of a 43-year-old nulligest, nulliparous woman who was being monitored by her gynecologist for cyclic hemorrhagic ovulations. She has a long history of rheumatic fever, which was discovered when she was 10 years old and was complicated by a tight mitral stenosis, requiring valve replacement surgery twice. She is currently on anticoagulant therapy.
The patient has also been diagnosed with systemic lupus erythematosus, rheumatoid arthritis, and Gougerot Sjogren syndrome since 2011. She initiated Methotrexate treatment, which was shortly substituted by Salazopyrin due to several allergic events. Later, she was treated with chloroquine and Cortancyl, but it was interrupted due to the onset of melanoderma. Additionally, she has a primary biliary cirrhosis and autoimmune hepatitis in the context of a hepatic overlap syndrome, for which a liver transplantation assessment was planned.
In 2017, she was diagnosed with a necrobiose uterine fibroid measuring 8*5 cm. Two years later, she was found to have multiple recurrent hemorrhagic ovarian cysts occurring at the beginning of each ovarian cycle. The patient was repeatedly hospitalized for hemorrhagic syndromes following iterative antivitamin K overdoses. During the last episode, she presented with a hemorrhagic right ovarian cyst rupture complicated by hemoperitoneum and profound anemia, with a 14-INR, controlled by interruption of oral anticoagulation, relayed by UFH and blood transfusions. As her hemodynamic status stabilized and her hemoglobin level increased, she was discharged on coumadin.
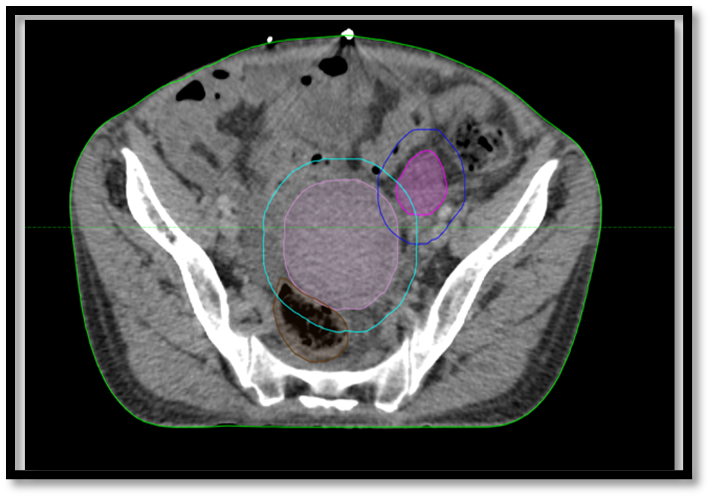
Due to the bleeding risk associated with surgical castration, as well as the potential risk of intramuscular injection of analogues, external ovarian radiotherapy for hemostasis was discussed in our multidisciplinary consultation meeting. A pelvic ultrasound was performed on the same day as the CT simulation, which showed a heterogeneous latero-uterine fluid formation of 53*50 mm with a fine echogenic contour in relation to a hemorrhagic cyst (Figure1).
Figure 1. Ultrasound of the latero-uterine fluid formation with fine echogenic contour in relation to a hemorrhagic cyst.
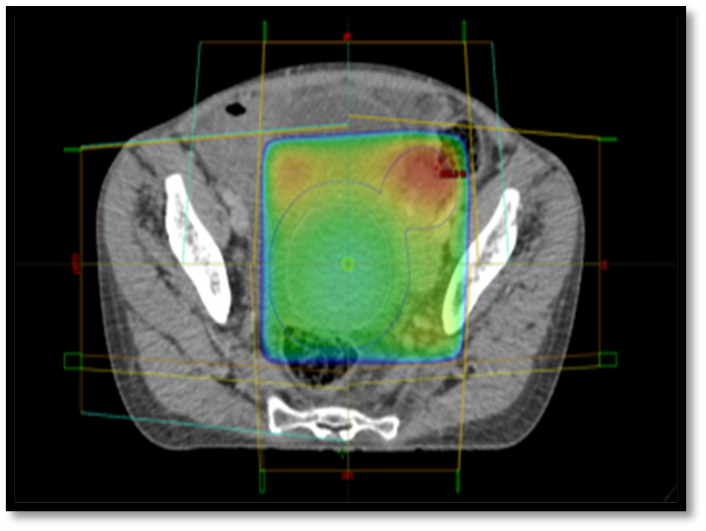
Unfortunately, the planned ovarian irradiation at a dose of 20 Gy in 5 fractions could not be administered to the patient. The patient died before the treatment could start due to a catastrophic and uncontrollable bleeding episode (Figures 2 and 3).
Figure 2. Radiotherapy target contouring for external ovarian irradiation.
Figure 3. Radiation treatment planning for external ovarian irradiation.
Discussion
The case presented here demonstrates the potential benefit of ovarian irradiation in the management of uncontrolled hemorrhage in a patient with multiple benign gynecological pathologies. While radiation therapy has been used for the treatment of benign diseases such as proliferative and inflammatory disorders, its role in the control of hemorrhage is not well established in the literature [2,3]. Ovarian irradiation is based on the hypersensitivity of ovarian tissue to radiotherapy, which suppresses hormone production and has been used in the treatment of hormone-dependent breast cancer [4,5]. The technique involves two opposed photon beams, with doses ranging from 12 to 20 Gy, and has been widely used in patients for whom radiation castration is indicated [6,7].
While ovarian irradiation has been previously reported in patients with endometriosis refractory to medical treatment and who are inoperable, the case presented here is unique due to the complexity of the patient's clinical presentation. Literature on the use of radiation therapy for the management of uncontrolled bleeding is limited, with few studies reporting successful outcomes [3,5,8-9]. In the cases discussed, bleeding was stopped following a hormonal fall with early menopause.
A retrospective study by Lucas Gomes Sapienza et al. showed excellent hemostatic control in patients treated with hypofractionated external beam radiotherapy for emergent palliation of bleeding tumors. This study highlights the effectiveness of hypo-fractionated irradiation, which is preferable to normo-fractionated regimens in preventing the risk of bleeding recurrence [1]. Pelvic radiotherapy is known for its side effects, particularly hormonal disturbances caused by ovarian irradiation, which induce early menopause in young women. However, when first-line treatments are not possible or ineffective, radiotherapy remains a treatment of choice.
From a practical standpoint, the simulation CT and irradiation should be synchronous with the appearance of the hemorrhagic cyst, and a single fraction of radiation therapy should be given with a short interval between simulation and pelvic irradiation to avoid side effects of radiotherapy and interruptions in the fractionation [1,10].
Conclusion
Our report presents a case of a patient with an uncontrolled hemorrhagic ovarian cyst who was deemed unfit for medical and surgical intervention due to her critical condition. Ovarian irradiation was planned to manage the bleeding, but unfortunately, the patient passed away before the treatment could be initiated.
Although the literature on the use of radiotherapy for benign gynecological diseases is limited, our case highlights the potential role of hemostatic radiotherapy in the management of refractory benign pathologies.
Future studies should be conducted to further explore the efficacy and safety of radiotherapy in the management of benign gynecological diseases and to identify the optimal treatment protocols.
Conflicts of Interests
None.
References
2. McKeown SR, Hatfield P, Prestwich RJ, Shaffer RE, Taylor RE. Radiotherapy for benign disease; assessing the risk of radiation-induced cancer following exposure to intermediate dose radiation. The British Journal of Radiology. 2015 Dec;88(1056):20150405.
3. Prabhu AV, Schad MD, Burnett AF, Lewis GD. Radiation treatment for refractory endometriosis: a 38-year-old female presenting with vaginal bleeding. Reports of Practical Oncology and Radiotherapy. 2021;26(3):457-62.
4. Kochbati L, Chaari N, Néji K, Ben Romdhane NK, Ben Amara F, Besbes M, et al. Ovarian irradiation for inoperable refractory endometriosis. Cancer Radiother. 2005;2005:341-2.
5. Leung SF, Tsao SY, Teo PM, Choi PH, Shiu WC. Ovarian ablation failures by radiation: a comparison of two dose schedules. The British Journal of Radiology. 1991 Jun;64(762):537-8.
6. Lemanski C, Cutuli B. Is ovarian radiotherapy still practiced?. In26° Days of the French Society of Senology and Mammary Pathology (SFSPM), Nancy, 2004. Breasts, Hormones and Antihormones. 2004 Nov 10 (pp. 281-289). Datebe SAS.
7. Haglund KE, Viswanathan AN. Computed Tomography–Based Radiation Therapy of Ovarian Remnants for Symptomatic Persistent Endometriosis. Obstetrics & Gynecology. 2008 Feb 1;111(2 Part 2):579-83.
8. Nomiya T, Harada M, Sudo H, Ota I, Ichikawa M, Suzuki M, et al. Radiotherapy for inoperable and refractory endometriosis presenting with massive hemorrhage: a case report. Journal of Medical Case Reports. 2012 Dec;6(1):308.
9. Kim KS, Moon WS, Song HW, Kim JH, Cho SN. A case of persistent endometriosis after total hysterectomy with both salpingo-oophorectomy managed by radiation therapy. Archives of Gynecology and Obstetrics. 2001 Nov;265:225-7.
10. Tetar S, Bruynzeel A, Bohoudi O, Nieboer T, Lagerwaard F. Pitfalls of Ovarian Ablative Magnetic Resonance-guided Radiation Therapy for Refractory Endometriosis. Cureus. 2018 Mar 9;10(3):e2294.