Abstract
The COVID-19 pandemic has made the development of novel vaccines a high priority for public health. While many vaccines have focused on the generation of neutralizing antibodies, we have discovered a novel herpes simplex virus (HSV) vaccine candidate, designated ΔgD-2, that can preferentially elicit non-neutralizing antibodies that function through Fcγ receptor (FcγR) activation and thus effector function of antibodies. In particular, the ΔgD-2 vector elicits FcγRIV-activating antibodies of the IgG2c isotype, which are associated with antibody-dependent cellular cytotoxicity (ADCC). The recent paper by Kaugars et al. 2021, demonstrates that a strain of ΔgD-2 expressing the hemagglutinin (HA) protein from influenza, designated ΔgD-2::HAPR8, can be used as a vaccine vector to protect against both influenza and HSV. In immunized sera, ΔgD-2::HAPR8 elicits high levels of anti-HA FcγRIV-activating IgG2c antibodies. Based on recent studies with the ΔgD-2 vector and its interaction with dendritic cells, we hypothesize that the vaccine works by promoting dendritic cell survival, allowing these cells to potently activate helper T cells, and ultimately leading to the immunoglobulin class switch in B cells. In this article, we discuss lessons from analyzing the ΔgD-2 vectors to elucidate antibody-dependent cellular killing. This work highlights the importance of combining antibody effector function and neutralization for optimal protective vaccine-induced immune responses.
Keywords
Cancer immunology, Clinical immunology, Immunochemistry
Antibody Protection Through Neutralization and Effector Function
The need for effective vaccines has never been so apparent as with the recent COVID-19 pandemic. The rapid development and dissemination of the mRNA-based vaccines have been critical in preventing infection and decreasing the morbidity and mortality of severe infection [1]. Much of vaccine development throughout history has been focused on obtaining high levels of neutralizing antibodies, which function by binding to pathogens and interfering with replication [2]. While neutralization is an important mechanism of protection against infection, neutralizing antibodies in particular drive the evolution of viral escape mutants, which ultimately reduce the effectiveness of these same antibodies [3]. However, neutralization assays are more widely used and standardized, whereas measuring other aspects of antibodies, like effector function, is more complicated but still gaining more attention [4-9]. The mRNA vaccines for COVID-19 have been designed to direct the immune response against the spike protein, and the neutralizing titer is used as a correlate of protection [10]. Extensive research in influenza has supported that neutralization titers are also correlated with protection [11]. Neutralization in influenza can occur when the antibodies bind to the surface receptor hemagglutinin (HA) to prevent its action in mediating viral entry and/or egress [12]. The majority of these antibodies from natural infection and vaccination are directed against the head region of the HA protein, which is highly variable [13]. This variability leads to antigenic drift, or a gradual accumulation of mutations over time, and reduced protection from existing immune responses [14].
Neutralizing antibodies can also be deleterious by themselves, such as in the case of dengue virus (DENV). Initial DENV infection is rarely fatal, but subsequent infection with a different subtype can lead to dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS) [15,16]. This is thought to be related to antibody-dependent enhancement (ADE) [17]. With ADE, the initial infection elicits neutralizing antibodies that are effective against that particular DENV subtype [17]. When subsequently infected with a different subtype, these antibodies partially neutralize the virus and lead to increased uptake into immune cells via opsonization [17]. This opsonization is facilitated by the interaction with an antibody-bound viral particle and receptors on the immune cell [18]. As the virus is only incompletely neutralized, the virus can then replicate within the immune cell, worsening the infection [17]. This has been a considerable barrier to the development of an effective DENV vaccine [17]. The live attenuated DENV vaccine from Sanofi Pasteur, Dengvaxia®, showed evidence of ADE in seronegative recipients, substantially limiting its use in resource-poor settings [19]. While neutralization is a widely recognized but sometimes complicated mechanism of protection, antibodies can also help direct the immune response though effector functions determined by their Fc regions.
A type of antibody effector function is antibody-dependent cellular cytotoxicity (ADCC). With ADCC, antibodies bind to antigens from pathogens expressed on the surface of infected cells. The Fc region of the antibodies then bind to the Fc receptors (FcRs) on immune cells [20]. This Fc region determines the subtype of antibodies and the FcRs that they can bind [20]. For example, the IgG2c subtype of antibodies in mice binds with high affinity to FcγRIV, which is associated with ADCC [20,21]. Of note, the IgG2c and IgG2a subtypes in mice are considered equivalent, and their presence depends on the strain of mouse [22]. Overall, the effector function depends on both the antibody subtype and type of immune cell [20].
Growing research into ideal immune responses has demonstrated that ADCC is an effective mechanism of protection against pathogens, like influenza and human immunodeficiency virus (HIV) [23]. Repeated studies have demonstrated that ADCC-mediating antibodies may have enhanced protective benefit against influenza [11]. In investigation of the effect of the trivalent inactivated seasonal influenza vaccine on infection of mice with the 2009 H1N1 virus, it was shown that, rather than enhancing infection, non-neutralizing antibodies led to increased antigen presentation and CD8+ T cell activation [24]. Ultimately, ADCC-mediating antibodies may be more effective against divergent strains of influenza, leading to a ”universal” influenza vaccine [25-28]. Research into optimal antibody response in HIV infection has shown that neutralizing antibodies rapidly generate escape mutants even at low titers while ADCC-mediating non-neutralizing antibodies do not [29,30]. Not only is ADCC increasing in importance in infectious diseases, but it is also recognized as a critical mechanism of action in antibody-mediated chemotherapy. For example, the therapeutic monoclonal antibodies trastuzumab and rituximab work by binding to human epidermal growth factor receptor 2 (HER2) and CD20, respectively; inducing ADCC; and leading to the destruction of cancer cells [31,32].
One illustrative example of ideal antigen selection also comes via research into immune responses against influenza. Target selection for novel influenza vaccines is critical yet controversial. Influenza HA has long been central to influenza vaccine development. HA is immunodominant, so much of the immune response in natural infection and current influenza vaccine is directed against HA, specifically the highly variable globular head region [33,34]. Antibodies binding to HA neutralize the virus before it can infect cells and generally work if there are no changes in its structure or glycosylation patterns [33,34]. Recent work has tried optimizing the HA protein itself to be more broadly protective, including strategies to direct the antibody response against less variable regions of HA [35-40]. However, HA may not be an ideal target for ADCC. One study indicated that anti-HA neutralizing antibodies inhibited the function of ADCC-mediating antibodies [41]. Therefore, different characteristics might be used to select other target antigens. As ADCC does not rely on neutralization as a mechanism of protection, non-neutralizing targets can be selected, which expands the repertoire of possible antigens for use in vaccine development. For example, the highly conserved nucleoprotein in influenza can be used as a target antigen for ADCC that could provide protection against a number of influenza strains [42].
Herpes Simplex Virus (HSV) Vaccine Development
One example of the failure of neutralization mediated by antibodies as a correlate of protection in vaccine development is found with HSV. As with many pathogens without efficacious vaccines, there are many types of vaccines in development, including subunit and live attenuated viruses [43,44]. However, none have received regulatory approval for commercialization. One well-known subunit vaccine trial was the HerpeVac trial [45]. A previous trial had established that the vaccine, a recombinant HSV-2 gD protein with adjuvant, was likely only going to be effective in seronegative women [46]. During the HerpeVac trial, sponsored by GlaxoSmithKline, the vaccine elicited high titers of neutralizing antibodies and prevented disease and infection of HSV-1 but not HSV-2 [45]. Further studies into the immune response elicited by the gD-subunit vaccine indicated that the serum from test subjects had higher neutralizing titers against HSV-1 than HSV-2, demonstrating a possible mechanism through which the vaccine may have only provided protection against HSV-1 [47]. Additionally, while the titer of gD-specific antibodies elicited correlated with greater vaccine efficacy, this vaccine did not provide substantial protective benefit in humans [48].
ΔgD-2 Protects by Eliciting Non-neutralizing Antibodies That Activate FcγRIV
The Jacobs and Herold laboratories developed an attenuated, single-cycle vaccine against HSV by deleting glycoprotein D (gD) from HSV-2, designated ΔgD-2, that elicits ADCC-mediating antibodies [49,50]. ΔgD-2-vaccinated mice develop a protective response to vaginal, ocular, and epithelial skin challenge with otherwise lethal doses of HSV-1 and HSV-2 [51-53]. This sterilizing immunity includes very limited symptoms of acute infection and no detectable latent virus in sensory ganglia [49,50]. ΔgD-2 is the first HSV vaccine shown to prevent the establishment of latent infection [54]. Passive transfer of ΔgD-2-immunized sera provided protection, while adoptive T cell transfer did not [49]. Importantly, transfer of immunized sera failed to protect mice lacking the FcγR common chain, allowing us to hypothesize that the mechanism of protection was from antibody-mediated FcγR functions [49]. Furthermore, the ΔgD-2-immunized sera had very low titers of neutralizing and IgG1 antibodies and high titers of IgG2c antibodies [50]. In the ΔgD-2 model, IgG2c antibodies are likely required for a protective immune response [49].
In Kaugars et al., 2021, we introduced a vaccine, ΔgD-2::HAPR8, that is protective against influenza and HSV during in vivo challenge [55]. To create ΔgD-2::HAPR8, we inserted the gene for HA from an H1N1 strain of influenza into ΔgD-2 [55]. We found that this vaccine specifically elicited high levels of FcγRIV-activating IgG2c antibodies against the influenza HA protein encoded within the recombinant virus and not influenza strains with other HAs. This vaccine also elicited IgG2c antibodies against HSV, similar to the parental vector [55]. The immunized sera had high titers in the hemagglutination inhibition assay, a well-established proxy for neutralizing titer for influenza vaccines [55]. To both probe immunological mechanisms and establish the potential study of other viral infections requiring immunodeficient mouse models with this vector, we tested our vector in mice without functional type I and II IFNs, specifically IFN-α/β (IFNAR-/-) and IFN-γ receptor-deficient (IFNγR-/-) mice, respectively [55]. With these studies, we demonstrated that ΔgD-2::RFP (a different recombinant of ΔgD-2 expressing the red fluorescent protein, rather than HA) was protective against HSV challenge in IFNAR-/- mice, and ΔgD-2::HAPR8 was protective against influenza challenge in IFNAR-/- and IFNγR -/- mice [55].
Mechanism of Elicitation of ADCC-mediating Antibodies
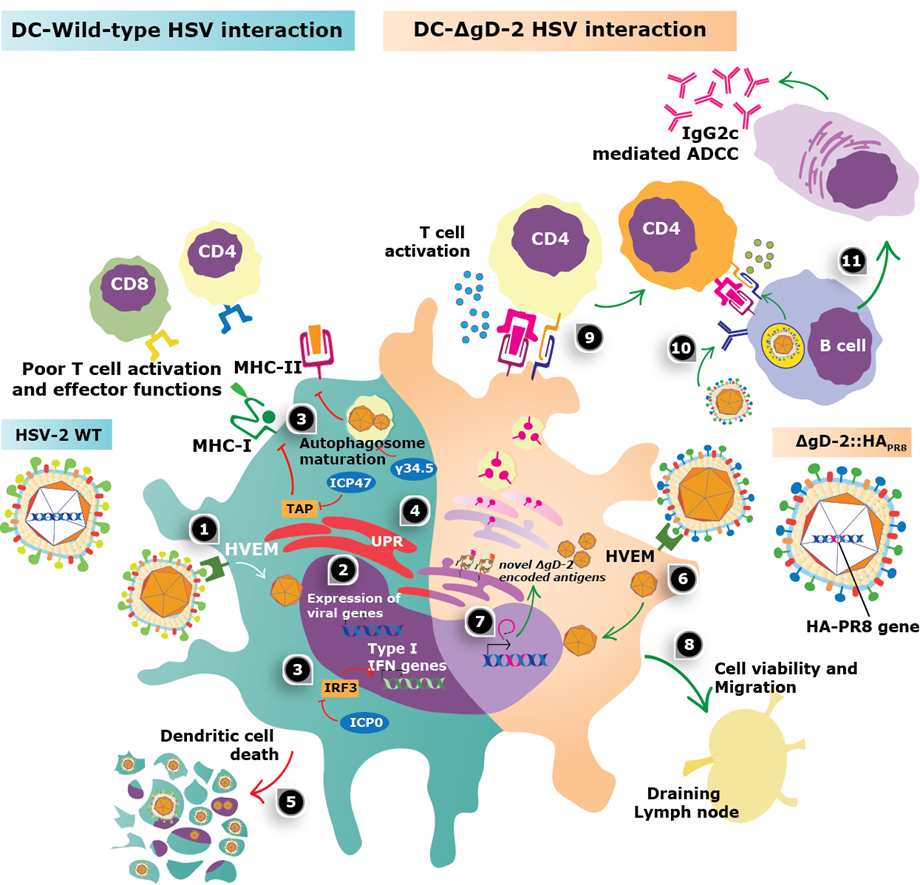
The mechanism through which ΔgD-2 specifically elicits IgG2c antibodies is unknown. Dendritic cells (DCs) are essential for the activation and differentiation of CD4+ T-helper cells that can support B cell differentiation and antibody class-switch; thus, analyzing the outcome of the ΔgD-2-DC interaction may be relevant for understanding how this vector promotes protection against influenza and HSV [55,56]. Previous research into ΔgD-2 found that this live attenuated virus can be favorably processed by DCs, unlike the wild-type virus, which otherwise induces significant DC death and hampers the function of these cells (Figure 1) [57,58]. The ΔgD-2 vector does not elicit the death of DCs, despite the expression of viral-encoded proteins within these cells, which likely promotes HSV antigen presentation. This result sharply contrasts against those obtained with HSV-2 mutants lacking other glycoproteins, such as gH (ΔgH-2), gI (ΔgI-2), or gJ (ΔgJ-2) – all of which rapidly killed DCs [59]. Compared with wild-type HSV, enhanced viability of DCs after inoculation with ΔgD-2 may relate to the fact that upon inoculation, this mutant does not induce an unfolded protein response (UPR) that is lethal for these cells [59,60]. Furthermore, inoculation of ΔgD-2 in the skin or footpads of mice promoted a significantly higher migration of dermal DCs (dDCs) to the draining lymph nodes and promoted both CD4+ and CD8+ T activation, as compared to the inoculation with the wild-type virus or the ΔgH-2 mutant [59]. dDCs have been related to HSV antigen presentation in the lymph nodes upon natural skin infection, particularly through the capture of apoptotic HSV-infected Langerhans cells [61,62]. Notably, the amount, type, kinetics, and phenotype of DCs interacting with antigen-specific T-helper cells in the lymph nodes significantly impacts the outcome of the overall immune response to particular antigens and B cell differentiation [61,63,64]. Thus, it will be relevant to characterize in depth the phenotype of the T-helper cells elicited by ΔgD-2 to assess the effects they exert over B cells to produce the effector antibodies with ADCC capacity. Finally, we have observed that the transfer of ΔgD-2-inoculated DCs into mice supported the production of high titers of antibodies against HSV and was sufficient to protect against intravaginal lethal challenge with HSV-2, highlighting the role of these cells in the protection elicited by this vector vaccine [59].
Thus, by deepening our knowledge of the immunological outcome of the ΔgD-2-DC interaction and focusing on the phenotype of the DCs inoculated with this mutant, the consequent characteristics of the T-helper cells activated by these DCs, and finally, the properties of the B cells secreting the relevant effector antibodies will shed light into the particular properties of ΔgD-2 that relate to the outstanding protection that this vector confers against pathogens. Overall, the assessment of DC interaction with HSV mutant vectors has been poorly explored, yet this might directly relate to protective antiviral immune responses against this and other viruses. The notion that DCs play a fundamental role in effective immune responses to inoculation with HSV is also supported in a report evaluating an HSV-1 mutant virus that lacks the amino terminus of γ34.5, which was also found to promote DCs to elicit an effective antiviral immune response [65].
Because gD from HSV can bind to the host immunomodulatory protein herpesvirus entry mediator (HVEM, HveA, ATAR, TR2, TNFRSF-14), which is widely expressed on the surface of immune cells [66], the contribution of HVEM signaling in the immune response elicited by ΔgD-2 vaccination gains particular relevance. Importantly, HVEM signaling was recently found to be involved in the generation of ADCC protective antibodies [52]. Furthermore, immune cells isolated from HVEM-deficient mice displayed impaired FcγR activation, which also occurred when adding recombinant gD protein to in vitro mouse and human FcγR activation assays [52]. Overall, this study supports an important role for HVEM signaling for ADCC and suggests that HSV utilizes gD to hamper this type of immune response that is ultimately detrimental for the virus. Thus, the capacity of the ΔgD-2 vector to promote ADCC antibodies may be at least partially mediated by the lack of gD expression in cells inoculated with this mutant virus.
Additionally, it is noteworthy to mention that the gD protein of HSV has been reported to suppress NK cell-mediated lysis of infected cells [52,67], impair T cell receptor (TCR) signaling in T cells, and inhibit T cell proliferation [68]. These effects of gD are likely to further dampen the host antiviral response upon natural infection with HSV, yet they would be at least partially absent during inoculation with the ΔgD-2 vector given that although this mutant virus is phenotypically complemented with gD in the viral particle, it cannot synthesize this protein de novo.
Discussion
Our research has addressed selection and expression of ideal antigens in vaccine vectors, as well as how best to specifically elicit an ADCC-based immune response. In particular, the ΔgD-2 vector elicits a strong ADCC-mediating humoral response, even to foreign antigens included in the vector. Based on previous work, infection of DCs by ΔgD-2 seems to be a critical step in generating its primarily IgG2c subtype of antibody. Given the importance of DCs in promoting immune responses that support B cell activation and differentiation, it will be interesting to assess the outcome of these cells upon interaction with varying recombinant ΔgD-2 viruses, as this may ultimately determine the levels and characteristics of the antibodies induced by this vector. Already, we have found that even IFNγR-/- mice can develop the same response to ΔgD-2::HAPR8, which is surprising as IFN-γ in particular has been associated with the class switch to IgG2c [55].
With this information, we hypothesize that this class switch could be through the activation of the innate immune response, involving signaling cascades involving molecules like the toll-like receptors (TLRs) and the downstream myeloid differentiation primary response protein 88 (MyD88) pathway in relevant immune cells [69,70]. TLR9 in particular could be involved, as it senses intracellular CpG-rich double-stranded DNA in B cells and plasmacytoid dendritic cells [71]. CpG DNA has been shown to lead to increased T-box transcription factor (T-bet) expression, inhibition of class switch of antibodies to IgG1 and IgE, and increased production of the IgG2a subtype of antibody (which is analogous to the IgG2c subtype in mice) [22,72]. Even in adenoviral vectors, MyD88 and TLR9 are critical in eliciting a strong antibody response [73]. Mice lacking functional MyD88 and TLR9 have been shown to have reduced antibody response to vaccines, particularly in the IgG2a and IgG2c subtypes [70,74]. From the data that we have gathered using ΔgD-2, basic information about specifically generating an ADCC-based humoral immune response can be answered to guide development of vaccines and other therapeutics.
Using this research, we can generate more information about what is important for ADCC-based immune responses, as this will lead to improved putative target selection. For example, some data has been published that supports that ADCC function is enhanced with higher antigen density [75]. Influenza HA is expressed at high levels on both virions and influenza-infected cells, 8-9x more than the neuraminidase protein [76]. The HA protein expressed in our vector elicited protection against challenge from its corresponding H1N1 strain of influenza [55]. However, the vaccine was not protective against challenges with other strains of influenza, including a more recent strain of H1N1 virus, supporting that HA was not the optimal antigen for broad influenza protection in this vector [55]. Ideal antigen selection has been a topic of debate during the COVID-19 pandemic. All current mRNA COVID-19 vaccines use the spike protein as an antigen [77,78]. More recently, the bivalent COVID-19 mRNA vaccines expressing two spike proteins have been approved for use in the US [79]. Future vaccine development may incorporate more and/or updated spike proteins or other viral antigens, like the nucleocapsid protein [80]. While our vector was first used with an antigen from the influenza virus, we are continuing our work on other viruses and types of pathogens, like bacteria such as Streptococcus pneumoniae and Mycobacterium tuberculosis.
Using neutralizing titers of antibodies as a correlate of protection has an established history, and assays to measure neutralization are usually simpler than those to measure other aspects of antibody function. However, there are limitations to relying solely on neutralization. Neutralization is particularly susceptible to mutations in variable regions of antigens and introduces a selective pressure for viral escape mutants. Neutralization is also only one way to assess the effectiveness of antibodies in infections. An ideal antibody response could utilize both neutralization and additional effector functions to provide optimal protection. With some of the monoclonal immunotherapy against both cancer and infectious disease, effector function is an important mechanism of action, as is neutralization [4,81-87]. However, the most established ways to improve ADCC function of antibodies are only for already discovered monoclonal antibodies. For example, modifying antibodies so that their Fc regions are afucosylated has been shown to enhance ADCC [88]. From the research that we have done with the ΔgD-2 vector, we hope to expand what is known about specifically eliciting a polyclonal humoral response that can strongly mediate ADCC in vivo against a selected antigen, as well as help optimize monoclonal antibody therapy for improved effector function.
The successful use of viral vectors in widespread populations has been limited. Outside of the mRNA COVID-19 vaccines, some strategies involved using a viral vector to express the spike protein of SARS-CoV-2. The most well-known and analyzed of these would be the Ad26.COV2.S, which consists of a replication-incompetent adenovirus expressing the COVID-19 spike protein [89]. However, many comparative analyses of Ad26.COV2.S and the mRNA-based vaccines have shown a more limited immune response from the viral vaccine [90,91]. While initial investigations into the use of viral vectors have been somewhat disappointing, viral vectors can still have advantages over more traditional formulations of vaccines. In the case of our previous research, we have found that the viral vector can shape the immune response in a beneficial manner that other approaches seem not to achieve. As we have seen the decrease in efficacy of the COVID-19 vaccines primarily reliant on neutralization, a more long-term effective approach may be to identify ideal immune responses that are beneficial in protecting against a variety of novel strains of COVID-19. This strategy may be not only beneficial in COVID-19, but in other pathogens as well that either do not have vaccines or have vaccines that provide suboptimal protection.
References
2. Tregoning JS, Flight KE, Higham SL, Wang Z, Pierce BF. Progress of the COVID-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nature Reviews Immunology. 2021 Oct;21(10):626-36.
3. Doud MB, Hensley SE, Bloom JD. Complete mapping of viral escape from neutralizing antibodies. PLoS pathogens. 2017 Mar 13;13(3):e1006271.
4. Garvin D, Stecha P, Gilden J, Wang J, Grailer J, Hartnett J, et al. Determining ADCC Activity of Antibody-Based Therapeutic Molecules using Two Bioluminescent Reporter-Based Bioassays. Current Protocols. 2021 Nov;1(11):e296.
5. Gogesch P, Dudek S, van Zandbergen G, Waibler Z, Anzaghe M. The role of FC receptors on the effectiveness of therapeutic monoclonal antibodies. International Journal of Molecular Sciences. 2021 Aug 19;22(16):8947.
6. Singh K, Marasini B, Chen X, Spearman P. A novel Ebola virus antibody-dependent cell-mediated cytotoxicity (Ebola ADCC) assay. Journal of Immunological Methods. 2018 Sep 1;460:10-6.
7. Chin DS, Lim CS, Nordin F, Arifin N, Jun TG. Antibody-dependent cell-mediated cytotoxicity through Natural Killer (NK) cells: Unlocking NK cells for future immunotherapy. Current Pharmaceutical Biotechnology. 2022 Mar 1;23(4):552-78.
8. Kamen L, Thakurta T, Myneni S, Zheng K, Chung S. Development of a kinetic antibody-dependent cellular cytotoxicity assay. Journal of Immunological Methods. 2019 May 1;468:49-54.
9. Lewis GK, Ackerman ME, Scarlatti G, Moog C, Robert-Guroff M, Kent SJ, et al. Knowns and unknowns of assaying antibody-dependent cell-mediated cytotoxicity against HIV-1. Frontiers in Immunology. 2019 May 10;10:1025.
10. Cromer D, Steain M, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralising antibody titres as predictors of protection against SARS-CoV-2 variants and the impact of boosting: a meta-analysis. The Lancet Microbe. 2022 Jan 1;3(1):e52-61.
11. Cox R. Correlates of protection to influenza virus, where do we go from here?. Human Vaccines & Immunotherapeutics. 2013 Feb 1;9(2):405-8.
12. Brandenburg B, Koudstaal W, Goudsmit J, Klaren V, Tang C, Bujny MV, et al. Mechanisms of hemagglutinin targeted influenza virus neutralization. PloS One. 2013 Dec 11;8(12):e80034.
13. Zost SJ, Wu NC, Hensley SE, Wilson IA. Immunodominance and antigenic variation of influenza virus hemagglutinin: implications for design of universal vaccine immunogens. The Journal of Infectious Diseases. 2019 Apr 8;219(Supplement_1):S38-45.
14. Das SR, Hensley SE, Ince WL, Brooke CB, Subba A, Delboy MG, et al. Defining influenza A virus hemagglutinin antigenic drift by sequential monoclonal antibody selection. Cell Host & Microbe. 2013 Mar 13;13(3):314-23.
15. Dejnirattisai W, Jumnainsong A, Onsirisakul N, Fitton P, Vasanawathana S, Limpitikul W, et al Cross-reacting antibodies enhance dengue virus infection in humans. Science. 2010 May 7;328(5979):745-8.
16. Wang TT, Sewatanon J, Memoli MJ, Wrammert J, Bournazos S, Bhaumik SK, et al. IgG antibodies to dengue enhanced for FcγRIIIA binding determine disease severity. Science. 2017 Jan 27;355(6323):395-8.
17. Shukla R, Ramasamy V, Shanmugam RK, Ahuja R, Khanna N. Antibody-dependent enhancement: a challenge for developing a safe dengue vaccine. Frontiers in cellular and infection microbiology. 2020:597.
18. Kulkarni R. Antibody-dependent enhancement of viral infections. InDynamics of immune activation in viral diseases 2020 (pp. 9-41).
19. Hadinegoro SR, Arredondo-García JL, Capeding MR, Deseda C, Chotpitayasunondh T, Dietze R, et al. Efficacy and long-term safety of a dengue vaccine in regions of endemic disease. New England Journal of Medicine. 2015 Sep 24;373(13):1195-206.
20. Bournazos S, DiLillo DJ, Ravetch JV. The role of Fc–FcγR interactions in IgG-mediated microbial neutralization. Journal of Experimental Medicine. 2015 Aug 24;212(9):1361-9.
21. Nimmerjahn F, Bruhns P, Horiuchi K, Ravetch JV. FcγRIV: a novel FcR with distinct IgG subclass specificity. Immunity. 2005 Jul 1;23(1):41-51.
22. Zhang Z, Goldschmidt T, Salter H. Possible allelic structure of IgG2a and IgG2c in mice. Molecular Immunology. 2012 Mar 1;50(3):169-71.
23. Von Holle TA, Moody MA. Influenza and antibody-dependent cellular cytotoxicity. Frontiers in Immunology. 2019 Jun 25;10:1457.
24. Kim JH, Reber AJ, Kumar A, Ramos P, Sica G, Music N, et al. Non-neutralizing antibodies induced by seasonal influenza vaccine prevent, not exacerbate A (H1N1) pdm09 disease. Scientific Reports. 2016 Nov 16;6(1):1-3.
25. Jegaskanda S, Weinfurter JT, Friedrich TC, Kent SJ. Antibody-dependent cellular cytotoxicity is associated with control of pandemic H1N1 influenza virus infection of macaques. Journal of Virology. 2013 May 15;87(10):5512-22.
26. Jegaskanda S, Luke C, Hickman HD, Sangster MY, Wieland-Alter WF, McBride JM, et al. Generation and protective ability of Influenza virus-specific antibody-dependent cellular cytotoxicity in humans elicited by vaccination, natural infection, and experimental challenge. The Journal of Infectious Diseases. 2016 Sep 15;214(6):945-52.
27. Gao R, Sheng Z, Sreenivasan CC, Wang D, Li F. Influenza A virus antibodies with antibody-dependent cellular cytotoxicity function. Viruses. 2020 Mar 1;12(3):276.
28. Jegaskanda S, Vanderven HA, Wheatley AK, Kent SJ. Fc or not Fc; that is the question: antibody Fc-receptor interactions are key to universal influenza vaccine design. Human Vaccines & Immunotherapeutics. 2017 Jun 3;13(6):1288-96.
29. Mielke D, Bandawe G, Pollara J, Abrahams MR, Nyanhete T, Moore PL, et al. Antibody-dependent cellular cytotoxicity (ADCC)-mediating antibodies constrain neutralizing antibody escape pathway. Frontiers in Immunology. 2019 Dec 11;10:2875.
30. Forthal DN, Finzi A. Antibody-dependent cellular cytotoxicity in HIV infection. AIDS. 2018;32(17):2439-51.
31. Weiner GJ. Rituximab: mechanism of action. Seminars in Hematology. 2010 Apr 1;47(2):115-23.
32. Petricevic B, Laengle J, Singer J, Sachet M, Fazekas J, Steger G, et al. Trastuzumab mediates antibody-dependent cell-mediated cytotoxicity and phagocytosis to the same extent in both adjuvant and metastatic HER2/neu breast cancer patients. Journal of translational medicine. 2013 Dec;11(1):1-1.
33. Zost SJ, Wu NC, Hensley SE, Wilson IA. Immunodominance and antigenic variation of influenza virus hemagglutinin: implications for design of universal vaccine immunogens. The Journal of Infectious Diseases. 2019 Apr 8;219(Supplement_1):S38-45.
34. Altman MO, Angeletti D, Yewdell JW. Antibody immunodominance: the key to understanding influenza virus antigenic drift. Viral Immunology. 2018 Mar 1;31(2):142-9.
35. Van der Lubbe JE, Verspuij JW, Huizingh J, Schmit-Tillemans SP, Tolboom JT, Dekking LE, et al. Mini-HA is superior to full length hemagglutinin immunization in inducing stem-specific antibodies and protection against group 1 influenza virus challenges in mice. Frontiers in Immunology. 2018 Oct 12;9:2350.
36. Christensen SR, Toulmin SA, Griesman T, Lamerato LE, Petrie JG, Martin ET, et al. Assessing the protective potential of H1N1 influenza virus hemagglutinin head and stalk antibodies in humans. Journal of Virology. 2019 Apr 15;93(8):e02134-18.
37. Eggink D, Goff PH, Palese P. Guiding the immune response against influenza virus hemagglutinin toward the conserved stalk domain by hyperglycosylation of the globular head domain. Journal of Virology. 2014 Jan 1;88(1):699-704.
38. Manenti A, Maciola AK, Trombetta CM, Kistner O, Casa E, Hyseni I, et al. Influenza anti-stalk antibodies: Development of a new method for the evaluation of the immune responses to universal vaccine. Vaccines. 2020 Jan 24;8(1):43.
39. Neu KE, Dunand CJ, Wilson PC. Heads, stalks and everything else: how can antibodies eradicate influenza as a human disease?. Current Opinion in Immunology. 2016 Oct 1;42:48-55.
40. Steel J, Lowen AC, Wang TT, Yondola M, Gao Q, Haye K, et al. Influenza virus vaccine based on the conserved hemagglutinin stalk domain. MBio. 2010 May 18;1(1):e00018-10.
41. He W, Tan GS, Mullarkey CE, Lee AJ, Lam MM, Krammer F, et al. Epitope specificity plays a critical role in regulating antibody-dependent cell-mediated cytotoxicity against influenza A virus. Proceedings of the National Academy of Sciences. 2016 Oct 18;113(42):11931-6.
42. Carragher DM, Kaminski DA, Moquin A, Hartson L, Randall TD. A novel role for non-neutralizing antibodies against nucleoprotein in facilitating resistance to influenza virus. The Journal of Immunology. 2008 Sep 15;181(6):4168-76.
43. Sandgren KJ, Truong NR, Smith JB, Bertram K, Cunningham AL. Vaccines for herpes simplex: recent progress driven by viral and adjuvant immunology. Herpes Simplex Virus. 2020:31-56.
44. Reyes A, Farías MA, Corrales N, Tognarelli E, González PA. Herpes Simplex Viruses Type 1 and Type 2 Infection and Immunity.
45. Belshe RB, Leone PA, Bernstein DI, Wald A, Levin MJ, Stapleton JT, et al. Efficacy results of a trial of a herpes simplex vaccine. New England Journal of Medicine. 2012 Jan 5;366(1):34-43.
46. Stanberry LR, Spruance SL, Cunningham AL, Bernstein DI, Mindel A, Sacks S, et al. Glycoprotein-D–adjuvant vaccine to prevent genital herpes. New England Journal of Medicine. 2002 Nov 21;347(21):1652-61.
47. Awasthi S, Belshe RB, Friedman HM. Better neutralization of herpes simplex virus type 1 (HSV-1) than HSV-2 by antibody from recipients of GlaxoSmithKline HSV-2 glycoprotein D2 subunit vaccine. The Journal of Infectious Diseases. 2014 Aug 15;210(4):571-5.
48. Belshe RB, Heineman TC, Bernstein DI, Bellamy AR, Ewell M, van der Most R, et al. Correlate of immune protection against HSV-1 genital disease in vaccinated women. The Journal of Infectious Diseases. 2014 Mar 15;209(6):828-36.
49. Petro C, Gonzalez PA, Cheshenko N, Jandl T, Khajoueinejad N, Benard A, et al. Herpes simplex type 2 virus deleted in glycoprotein D protects against vaginal, skin and neural disease. Elife. 2015 Mar 10;4:e06054.
50. Petro CD, Weinrick B, Khajoueinejad N, Burn C, Sellers R, Jacobs Jr WR, et al. HSV-2 ΔgD elicits FcγR-effector antibodies that protect against clinical isolates. JCI Insight. 2016 Aug 8;1(12).
51. Herold BC, Petro C, Burn C, Weiss K, Ramsey N, Weinrick B, Jacobs W. Herpes Simplex Virus (HSV)-2 Candidate Vaccine Virus Deleted in Glycoprotein D (ΔgD-2) Elicits High-Titer Immunoglobulin (Ig) G2 Antibodies With Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC) Activity, Protects Mice From Skin and Vaginal Challenge With Clinical Isolates of HSV-1 and HSV-2, and Prevents the Establishment of Latency. InOpen Forum Infectious Diseases 2016 Dec 1 (Vol. 3, No. suppl_1).
52. Burn C, Ramsey N, Garforth SJ, Almo S, Jacobs Jr WR, Herold BC. A herpes simplex virus (HSV)-2 single-cycle candidate vaccine deleted in glycoprotein D protects male mice from lethal skin challenge with clinical isolates of HSV-1 and HSV-2. The Journal of Infectious Diseases. 2018 Feb 14;217(5):754-8.
53. Ramsey NL, Visciano M, Hunte R, Loh LN, Burn Aschner C, Jacobs Jr WR, et al. A single-cycle glycoprotein D deletion viral vaccine candidate, ΔgD-2, elicits polyfunctional antibodies that protect against ocular herpes simplex virus. Journal of Virology. 2020 Jun 16;94(13):e00335-20.
54. Johnston C, Gottlieb SL, Wald A. Status of vaccine research and development of vaccines for herpes simplex virus. Vaccine. 2016 Jun 3;34(26):2948-52.
55. Kaugars K, Dardick J, de Oliveira AP, Weiss KA, Lukose R, Kim J, et al. A recombinant herpes virus expressing influenza hemagglutinin confers protection and induces antibody-dependent cellular cytotoxicity. Proceedings of the National Academy of Sciences. 2021 Aug 24;118(34):e2110714118.
56. Retamal-Díaz AR, Kalergis AM, Bueno SM, González PA. A herpes simplex virus type 2 deleted for glycoprotein D enables dendritic cells to activate CD4+ and CD8+ T cells. Frontiers in Immunology. 2017 Aug 9;8:904.
57. Ma F, Lf D, Ei T, Pa G. Herpes simplex virus interference with immunity: Focus on dendritic cells. Virulence. 2021 Dec 31;12(1):2583-607.
58. Stefanidou M, Ramos I, Mas Casullo V, Trépanier JB, Rosenbaum S, Fernandez-Sesma A, et al. Herpes simplex virus 2 (HSV-2) prevents dendritic cell maturation, induces apoptosis, and triggers release of proinflammatory cytokines: potential links to HSV-HIV synergy. Journal of Virology. 2013 Feb 1;87(3):1443-53.
59. Retamal-Díaz A, Weiss KA, Tognarelli EI, Freire M, Bueno SM, Herold BC, et al. US6 gene deletion in herpes simplex virus type 2 enhances dendritic cell function and T cell activation. Frontiers in Immunology. 2017 Nov 10;8:1523.
60. Tognarelli EI, Retamal-Díaz A, Farías MA, Duarte LF, Palomino TF, Ibañez FJ, et al. Pharmacological inhibition of IRE-1 alpha activity in herpes simplex virus type 1 and type 2-infected dendritic cells enhances T cell activation. Frontiers in Immunology. 2021;12.
61. Puttur FK, Fernandez MA, White R, Roediger B, Cunningham AL, Weninger W, Jones CA. Herpes simplex virus infects skin γδ T cells before langerhans cells and impedes migration of infected langerhans cells by inducing apoptosis and blocking E-cadherin downregulation. The Journal of Immunology. 2010 Jul 1;185(1):477-87.
62. Kim M, Truong NR, James V, Bosnjak L, Sandgren KJ, Harman AN, et al. Relay of herpes simplex virus between Langerhans cells and dermal dendritic cells in human skin. PLoS pathogens. 2015 Apr 13;11(4):e1004812.
63. Han JY, Sloan DD, Aubert M, Miller SA, Dang CH, Jerome KR. Apoptosis and antigen receptor function in T and B cells following exposure to herpes simplex virus. Virology. 2007 Mar 15;359(2):253-63.
64. Benson RA, MacLeod MK, Hale BG, Patakas A, Garside P, Brewer JM. Antigen presentation kinetics control T cell/dendritic cell interactions and follicular helper T cell generation in vivo. Elife. 2015 Aug 10;4:e06994.
65. Ma Y, Chen M, Jin H, Prabhakar BS, Valyi-Nagy T, He B. An engineered herpesvirus activates dendritic cells and induces protective immunity. Scientific Reports. 2017 Feb 2;7(1):1-0.
66. Kwon BS, Tan KB, Ni J, Kwi-Ok-Oh ZH, Kim KK, Kim YJ, et al. A newly identified member of the tumor necrosis factor receptor superfamily with a wide tissue distribution and involvement in lymphocyte activation. Journal of Biological Chemistry. 1997 May 30;272(22):14272-6.
67. Grauwet K, Cantoni C, Parodi M, De Maria A, Devriendt B, Pende D, et al. Modulation of CD112 by the alphaherpesvirus gD protein suppresses DNAM-1-dependent NK cell-mediated lysis of infected cells. Proceedings of the National Academy of Sciences. 2014 Nov 11;111(45):16118-23.
68. La S, Kim J, Kwon BS, Kwon B. Herpes simplex virus type 1 glycoprotein D inhibits T-cell proliferation. Molecules and Cells. 2002 Dec 31;14(3):398-403.
69. Barr TA, Brown S, Mastroeni P, Gray D. B cell intrinsic MyD88 signals drive IFN-γ production from T cells and control switching to IgG2c. The Journal of Immunology. 2009 Jul 15;183(2):1005-12.
70. Kang SM, Yoo DG, Kim MC, Song JM, Park MK, O E, et al. MyD88 plays an essential role in inducing B cells capable of differentiating into antibody-secreting cells after vaccination. Journal of Virology. 2011 Nov 1;85(21):11391-400.
71. Ma Y, He B. Recognition of herpes simplex viruses: toll-like receptors and beyond. Journal of Molecular Biology. 2014 Mar 20;426(6):1133-47.
72. Liu N, Ohnishi N, Ni L, Akira S, Bacon KB. CpG directly induces T-bet expression and inhibits IgG1 and IgE switching in B cells. Nature Immunology. 2003 Jul;4(7):687-93.
73. Zhu J, Huang X, Yang Y. The TLR9-MyD88 pathway is critical for adaptive immune responses to adeno-associated virus gene therapy vectors in mice. The Journal of Clinical Investigation. 2009 Aug 3;119(8):2388-98.
74. Lin L, Gerth AJ, Peng SL. CpG DNA redirects class‐switching towards" Th1‐like" Ig isotype production via TLR9 and MyD88. European Journal of Immunology. 2004 May;34(5):1483-7.
75. Temming AR, de Taeye SW, de Graaf EL, de Neef LA, Dekkers G, Bruggeman CW, et al. Functional attributes of antibodies, effector cells, and target cells affecting NK cell-mediated antibody-dependent cellular cytotoxicity. The Journal of Immunology. 2019 Dec 15;203(12):3126-35.
76. Hutchinson EC, Charles PD, Hester SS, Thomas B, Trudgian D, Martínez-Alonso M, et al. Conserved and host-specific features of influenza virion architecture. Nature Communications. 2014 Sep 16;5(1):1-1.
77. Heinz FX, Stiasny K. Distinguishing features of current COVID-19 vaccines: knowns and unknowns of antigen presentation and modes of action. NPJ Vaccines. 2021 Aug 16;6(1):1-3.
78. Dai L, Gao GF. Viral targets for vaccines against COVID-19. Nature Reviews Immunology. 2021 Feb;21(2):73-82.
79. Chalkias S, Eder F, Essink B, Khetan S, Nestorova B, Feng J, Chen X, Chang Y, Zhou H, Montefiori D, Edwards DK. Safety, immunogenicity and antibody persistence of a bivalent beta-containing booster vaccine against COVID-19: a phase 2/3 trial. Nature Medicine. 2022 Oct 6:1-0.
80. Thura M, Sng JX, Ang KH, Li J, Gupta A, Hong JM, et al Targeting intra-viral conserved nucleocapsid (N) proteins as novel vaccines against SARS-CoVs. Bioscience Reports. 2021 Sep 30;41(9).
81. Cui T, Huang M, Su X, Lin Z, Zhong J, Yang X, et al. Potential of Antibody-Dependent Cellular Cytotoxicity in Acute and Recovery Phases of SARS-CoV-2 Infection. Infectious Diseases & Immunity. 2022 Apr 20;2(02):74-82.
82. Yu L, Liu X, Ye X, Su W, Zhang X, Deng W, et al. Monoclonal Antibodies against Zika Virus NS1 Protein Confer Protection via Fc γ Receptor-Dependent and-Independent Pathways. Mbio. 2021 Feb 9;12(1):es03179-20.
83. Tso FY, Lidenge SJ, Poppe LK, Pena PB, Privatt SR, Bennett SJ, et al. Presence of antibody-dependent cellular cytotoxicity (ADCC) against SARS-CoV-2 in COVID-19 plasma. PLoS One. 2021 Mar 4;16(3):e0247640.
84. Focosi D, McConnell S, Casadevall A, Cappello E, Valdiserra G, Tuccori M. Monoclonal antibody therapies against SARS-CoV-2. Lancet Infect Dis. 2022 Nov;22(11): e311-e326.
85. VanBlargan LA, Errico JM, Halfmann PJ, Zost SJ, Crowe JE, Purcell LA, et al. An infectious SARS-CoV-2 B. 1.1. 529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nature Medicine. 2022 Mar;28(3):490-5.
86. Beaudoin-Bussières G, Chen Y, Ullah I, Prévost J, Tolbert WD, Symmes K, et al. A Fc-enhanced NTD-binding non-neutralizing antibody delays virus spread and synergizes with a nAb to protect mice from lethal SARS-CoV-2 infection. Cell Reports. 2022 Feb 15;38(7):110368.
87. Cameroni E, Bowen JE, Rosen LE, Saliba C, Zepeda SK, Culap K, et al. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature. 2022 Feb;602(7898):664-70.
88. Pereira NA, Chan KF, Lin PC, Song Z. The “less-is-more” in therapeutic antibodies: Afucosylated anti-cancer antibodies with enhanced antibody-dependent cellular cytotoxicity. InMAbs 2018 Jul 4 (Vol. 10, No. 5, pp. 693-711).
89. Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, et al. Final analysis of efficacy and safety of single-dose Ad26. COV2. S. New England Journal of Medicine. 2022 Mar 3;386(9):847-60.
90. Padhiar NH, Liu JB, Wang X, Wang XL, Bodnar BH, Khan S, et al. Comparison of BNT162b2-, mRNA-1273-and Ad26. COV2. S-Elicited IgG and Neutralizing Titers against SARS-CoV-2 and Its Variants. Vaccines. 2022 May 27;10(6):858.
91. Barbeau DJ, Martin JM, Carney E, Dougherty E, Doyle JD, Dermody TS, et al. Comparative analysis of human immune responses following SARS-CoV-2 vaccination with BNT162b2, mRNA-1273, or Ad26. COV2. S. NPJ Vaccines. 2022 Jul 6;7(1):1-6.