Abstract
Objective: The goal of this review is to provide a succinct, yet comprehensive, guide to the antepartum management of multiple gestations.
Methods: This narrative review on twins and multiple gestation provides a concise guide for providers with this ever-growing patient population. PubMED was utilized for literature search. Each reference was evaluated and graded for quality of evidence by US Preventative Services Task Force and Cochrane Review guidelines. Screening, surveillance, and management strategies are delineated succinctly and organized by type of multiple gestation being managed from the lowest risk dichorionic twin pair to the increasingly escalating risks of twins and higher order multiples sharing a placenta and/or amniotic sac.
Results: The incidence of twin pregnancies has grown over the past several years, due in large part to delayed reproductive timing and surge in assisted reproductive technologies. Twin pregnancies are associated with higher morbidity for both gravidas and offspring, warranting evidence-based approach in counseling and management.
Conclusions: We note the important differences among multiples in chorionicity and amnionicity, in the importance of close surveillance and early delivery. Graded clinical pearls and evidence-based recommendations are presented to guide obstetric providers.
Keywords
Multiple gestation, Twin pregnancy, Triplet pregnancy, High order multiple pregnancy, High risk pregnancy
Introduction
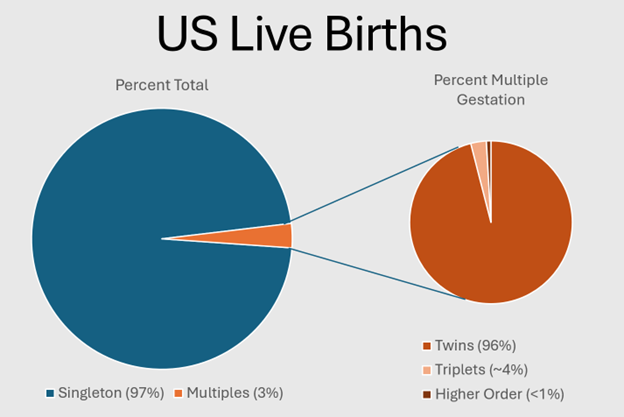
The incidence of twin pregnancies has grown over the past several decades. The observed increase in twining is mostly attributable to two etiologies: 1) increased use of assisted reproductive technology (ART), which is associated with increased risk for multiples, and 2) shift toward childbearing later in life or delayed reproductive timing, which is more likely to result in spontaneous multifetal gestation even without use of ART; (Figure 1) [1-4]. Multiple gestations pose increased risk for both the pregnant person and her fetuses as noted in (Table 1) [1,5-9]. Maternal mortality increases 2.5-fold during multiple gestation compared to a singleton pregnancy [10]. In general, the mean gestational age at delivery of twins is about 35 weeks for multiples [10-12]. More clinically meaningful is the increased incidence of very premature delivery at less than 32 weeks, which occurs in 1.6% of singletons and 12% of twins [12]. This increased prematurity burden leads to a significantly higher incidence of low birth weight; birth weights of less than 1500 g are 10 times more common than in singletons. Further, the stillbirth rate in twins is doubled. In aggregate, these complications result in a significantly higher perinatal mortality rate in all twins, approximately 3 times higher than their singleton counterparts [7].
Figure 1. Epidemiology of twins and multiples in the US.
|
Maternal |
Fetal |
|
Hypertensive disorders of pregnancy Pruritic urticarial papules and plaques of pregnancy Iron deficiency anemia Acute fatty liver of pregnancy Thromboembolic events Placental abruption Preterm labor Preterm premature rupture of membranes Intra-amniotic infections Intrahepatic cholestasis of pregnancy Postpartum hemorrhage Cesarean delivery Gestational diabetes Postpartum depression Mortality |
General Preterm birth Fetal growth restriction Growth discordance Birth anomalies Miscarriage Fetal demise
Monochorionic Specific Twin-twin transfusion syndrome Twin anemia polycythemia syndrome
Monoamnionic Specific Cord Entanglement |
Understanding the most up-to-date management of these pregnancies is critical for patient counselling and identifying patients in need of referral to specialists for support, assistance, and guidance. This narrative review has a broad scope targeting multiple gestations in clinical care and is comprehensive in its aim. The intent of this narrative review is to offer a concise outline of the management of spontaneous multiples to help guide providers with a specific focus on diagnosis, surveillance, and antepartum management. Our narrative review outlines risk pertinent to each type of multiple along with evidence-based clinical strategies uniquely suited to minimize such risks to achieve healthy pregnancy outcomes.
Our objective for this review is to provide a succinct, yet comprehensive, guide to the antepartum management of multiple gestations. Given the broad scope, the format utilized constitutes a narrative review.
Methods
We utilized PubMED to search the obstetric literature. We reviewed previously published review articles, primary research articles, and society recommendations published from the year 2000 to today in the English language in human subjects. Once we achieved our aim in identifying representative studies and manuscripts to support each key point in our review, this author group reached a consensus of adequate sourcing to support our statements and clinical practice recommendations.
Key statements, updates, and recommendations for clinical practice are scored by quality of evidence; see (Tables 2-3). A comprehensive review of the systematic review, articles included, and level of evidence can be seen in Supplemental Table 1 and Supplemental Figure 1. Levels are scored and recorded in the reference section after each source. Provision of guidelines and recommendations rooted in evidence are intended to direct clinicians to the best management and reduce medico-legal risk in these high-risk pregnancies [13,14]. References were evaluated and graded for quality as outlined by the US Preventative Services Task Force (USPSTF) and Cochrane Review.
|
Ia |
Evidence obtained from meta-analysis of randomized controlled trials |
|
Ib |
Evidence obtained from at least one randomized controlled trial |
|
IIa |
Evidence obtained from at least one well-designed controlled study without randomization |
|
IIb |
Evidence obtained from at least one other type of well-designed quasi-experimental study |
|
III |
Evidence obtained from well-designed non-experimental descriptive studies, such as comparative studies, correlation studies and case studies |
|
IV |
Evidence obtained from expert committee reports or opinions and/or clinical experience of respected authorities |
|
A |
At least one randomized controlled trial as part of a body of literature of overall good quality and consistency addressing the specific recommendation (Evidence levels Ia or Ib) |
|
B |
Well-controlled clinical studies available but no randomized clinical trials on the topic of the recommendations (Evidence Levels IIa, IIb, or III) |
|
C |
Evidence obtained from expert committee reports or opinions and/or clinical experiences of respected authorities, indicates an absence of directly applicable clinical studies of good quality (Evidence Level IV) |
|
D |
Recommended best practice based on the clinical experience of the authors |
|
Ryan R, Hill S. How to GRADE the quality of the evidence. Cochrane Consumers and Communication Group. 2016. Available at http://cccrg.cochrane.org/author-resources. Version 3.0 December 2016; www.ahrq.gov (US Preventive Services Task Force) |
|
Multiple Pregnancy
Biology of twinning
The process of human ovulation typically proceeds with follicle stimulating hormone (FSH) driving a signaling pathway that manifests in selection, maturation, and release of an oocyte from a singular, dominant follicle. Dizygotic twinning occurs when more than one follicle matures and each releases their oocyte into the Fallopian tubes. Dizygotic twins are otherwise known as fraternal twins or non-identical twins. Dizygotic twins may or may not share the same sex but typically are conceived by a singular maternal-paternal pair [15]. Rarely, dizygotic twins may not share the same father and be hetero-paternal because of superfecundation—fertilization of two or more ova during the same cycle from sperm from different males inherently via separate acts of sexual intercourse [15].
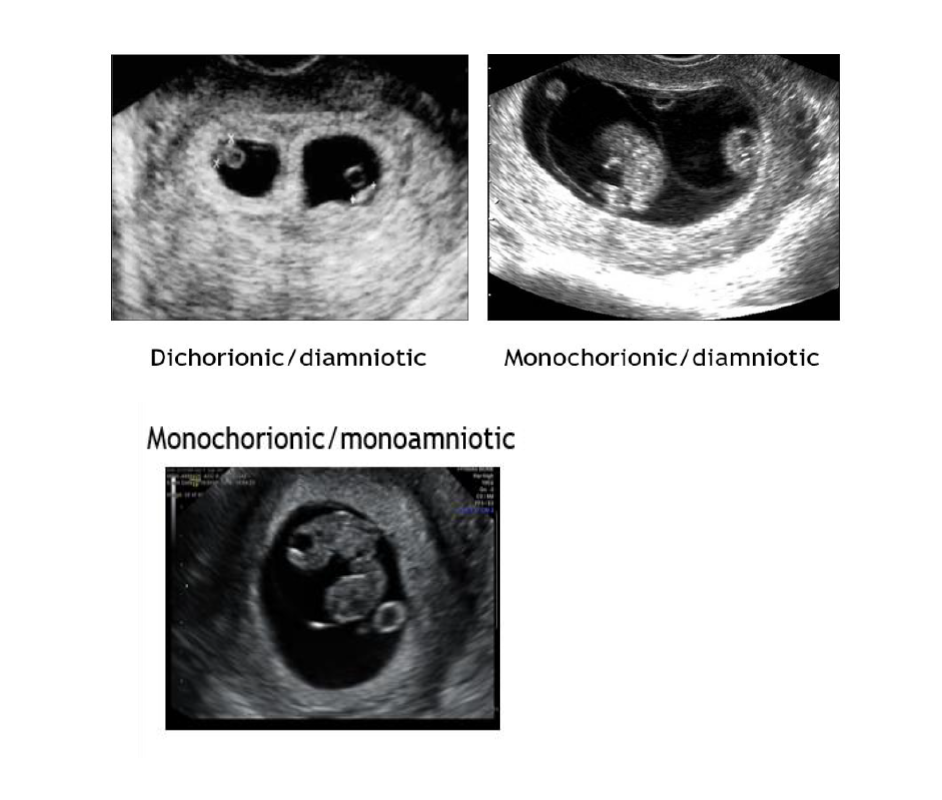
Conversely, monozygotic twinning occurs when there is the typical release of a singular oocyte from the dominant follicle and fertilization occurs. It is followed by division of the resulting zygote. The timing of the division dictates the type of twinning that occurs. Monozygotic twinning will result in a dichorionic-diamniotic twin pair when the division occurs day 0-3. A monochorionic-diamniotic twin pair occurs when the division occurs between day 3 and 8. Division between days 8 and 13 generates a monochorionic-monoamniotic twin pregnancy. Conjoined twins consequently results when division process begins after day 13 [16].
Vanishing twin syndrome
Twins and high order multiples are conceived at a higher frequency than their corresponding birth rate. A fetus may undergo an arrest in development and subsequent resorption as the remaining fetus(es) continue to grow and mature; this biologic occurrence is categorized as a “vanishing twin” and may be demonstrated on ultrasound. In general, surviving twins have a good prognosis but data have implicated increased risk for low birth weight in the surviving twin [17].
Establishment of chorionicity and amnionicity
Twins and multiple gestations that share placentation and/or amnionicity add additional concerns with respect to risks and management strategies. Accordingly, defining chorionicity and amnionicity is paramount in guiding all parameters of the pregnancy. Physicians utilize ultrasound to define fetal number, chorionicity, and amnionicity. When dating by ultrasound in setting of unknown last menstrual period (LMP), the crown-rump length (CRL) of the largest fetus is utilized; this strategy has been selected to avoid using the CRL of a fetus with early growth pathology [17].
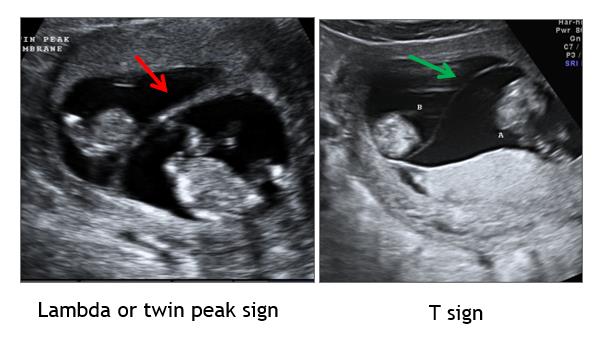
Several guiding principles are used to define chorionicity including membrane thickness, number of membrane layers, number of placental sites, presence of the lambda or T-sign, and other composite measures; (Figure 2) and (Figure 3). Composite measures would include ability to discern the number of placental masses, number of gestational sacs, number of fetal poles, and whether fetal sex is concordant/discordant. The number of yolk sacs usually equates to the number of amnions. Membrane thickness in monochorionic (MC) pairs has been described subjectively as “thin” or “whispy”; this description has been investigated using numerical measurement with thresholds for thickness ranging from <1.0-2.0 mm [18-20].
Figure 2. First trimester ultrasound and chorionicity/amnionicity.
Figure 3. First Trimester membranes and sonographic markers.
Genetic Screening and Testing in Multiples
Screening
There is currently no clear standard of screening for chromosomal anomalies in multiples [21]. There is an increased risk in anomalies in twins primarily due to the increased likelihood of twinning with advanced maternal age [17,21]. Further, zygosity has been shown to impact the results of genetic testing in multiples. In monozygotic twins, the risk for aneuploidy is the same as singleton pregnancies, and both fetuses are either affected or not affected. However, in dizygotic twins, the risk that one fetus is affected by aneuploidy is doubled as each twin has its own individual risk for aneuploidy. The risk of the whole pregnancy being affected by aneuploidy is calculated by the sum of the individual risks of both fetuses. In multiples beyond twins, if separate chorions, then the pregnancy specific risk for aneuploidy can be calculated by multiplying the singleton risk by the total number of fetuses. Screening modalities are outlined in (Table 4) [4,17,21-27].
Due to the risk of vanishing twin or vanishing fetus multiple marker serum screens should be interpreted with caution. A “normal” twin may be offset by an abnormal twin or alternatively abnormal values may be projected due to a vanishing fetus that may or may not be evident on ultrasound [21].
|
Screening Modality |
Considerations |
|
|
First Trimester Screen |
Monochorionic |
Dichorionic |
|
NT measurements are averaged and calculated as single risk estimate. Increased NT of one twin may be early sign of TTTS. |
Each fetus is treated as separate with NT as separate risks. Each twin has its own independent risk and overall pregnancy risk is based on combined risk of both twins. An unaffected twin can mask affected twin. |
|
|
Maternal Serum Screen |
↓ PAPP-A, ↑ HCG, ↑ inhibin associated with preterm birth |
|
|
Noninvasive Prenatal Testing |
tFF can be up to 35% higher, but fetal fraction per twin is lower May be particularly helpful for screening T21 |
|
|
NT: Nuchal Translucency; TTTS: Twin-Twin Transfusion Syndrome; tFF: Total Fetal Fraction; PAPP-A: Pregnancy Associated Plasma Protein-A; HCG: Human Chorionic Gonadotropin; AFP: Alpha Fetoprotein; T21: Trisomy 21. |
||
Diagnostic testing
The primary questions regarding diagnostic genetic testing in twins involve the ability to reliably ascertain that each fetus is being equally sampled (if applicable) and if there is greater risk in fetal loss. To ensure sampling of each amniotic sac in the case of a dichorionic (DC) pregnancy, multiple modalities can be used including instilling colored dye into the initial sac during amniocentesis, injecting your needle through the separating membrane, or merely leaving the needle in the initial sac as a placeholder [28]. It is currently unclear if there is an increased risk for fetal loss during amniocentesis and chorionic villus sampling in multiples. Some studies have shown no increased risk [29], while other articles have shown that there may be an increased risk [17,30]. Patients should be counseled appropriately on the risks of these procedures as well as the current uncertainty regarding increased risk in multiples.
Nutrition, Maternal Activity, and Exercise in Multiple Gestation
Ideally women begin prenatal vitamin with folic acid supplementation preconception to ensure that adequate folic acid levels are present in the first 42 days of conception during the bulk of organogenesis; such strategy aids in prevention of open neural tube defects (ONTD). Most prenatal vitamins include 0.4-0.8 mg folic acid, which falls short of the recommended 1 mg folic acid daily supplement in twins and high order multiple gestation [31].
While all prenatal vitamins include iron, requirements to prevent anemia vary in multiples varies by trimester: 30 mg daily (first trimester) and 60 mg daily (second and third trimesters). A good clinical practice in multiple gestation is to monitor blood count and iron profile each trimester as low ferritin even in the setting of normal hemoglobin can trigger symptoms of restless leg syndrome, low energy/fatigue, irritability/moodiness, difficulty concentrating, and insomnia/poor sleep [32].
Women must consume 100 mg protein daily to achieve adequate protein intake for multiple gestations. Animal-based protein is more easily absorbed than plant-based sources. Hence, vegan diets should be carefully monitored to ensure adequate intake of lentils, legumes, beans, tofu, nuts, and seeds. Modern protein bars and shakes and flavored peptide supplements serve as additional healthy options [33,34].
In multiple gestations, women should increase their daily intake by 300 calories/fetus in the first trimester, 340 calories/fetus in the second trimester, and 452 calories/fetus in the third trimester. Given the expanding gravid uterus and side effects of slowed motility with the progesterone of pregnancy, many women with multiple gestation struggle to maintain adequate intake; such situations should be treated with antiemetics, antacids, and motility agents. Activity and exercise recommendations in multiple pregnancies remains unclear with no official recommendation [35,36].
Antepartum Twin Management: Surveillance of Growth and Fetal Status
Twin and high order multiple pregnancies carry the inherent risk for abnormal growth pattern and require surveillance beyond the fundal height surveillance. Moreover, biometry measurements in twins normally vary from singletons throughout the mid and late trimesters; this effectively generates a twin-specific growth trajectory [37,38]. Despite the evidence mounting that twin growth should be followed by referent metrics specific to twins, practices continue to utilize singleton population data to generate weight percentiles for twin pregnancy.
One of the many unintended consequences of this practice is the false positive identification for Fetal Growth Restriction (FGR), which poses risk of arranging Doppler evaluations, antenatal testing, and iatrogenic preterm birth. Utilizing twin specific growth charts has been shown to be effective in reducing diagnosis of FGR in twins without increasing risk for fetal demise (FD) [39]. While twin-specific growth charts may reduce unnecessary surveillance and iatrogenic preterm birth, data indicate that twins identified as FGR with singleton growth curves exhibit higher perinatal mortality rate than singletons [40]. Because growth patterns and risk vary by chorionicity and amnionicity, surveillance recommendations vary according to type of multiple gestation.
Fetal growth restriction in multiples and Delphi procedure
The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) posts guidelines specific to twin pregnancy with respect to the identification and surveillance of selective fetal growth restriction (sFGR). sFGR criteria include the following: (1) One twin less than the 10th percentile in DC pregnancies and (2) Estimated Fetal Weight (EFW) of one twin less than the 10th percentile and EFW discordance is greater than 25% in MC pregnancies [41]. Historically, experts have debated criteria for identifying sFGR in twin pregnancies. The Delphi procedure was generated with the intent of uniform diagnosis for sFGR. According to expert consensus labeled Delphi procedure, EFW less than the third percentile in one twin is sufficient for sFGR categorization in both MC and DC twins. Additional criteria for DC twins include sFGR when two of three contributing criteria are present: (1) EFW less than the 10th percentile, (2) EFW discordance greater than or equal to 25%, or (3) umbilical artery (UA) pulsatility index (PI) greater than the 95th percentile. MC twins meet criteria for sFGR if two out of four parameters are observed: (1) EFW less than the 10th percentile, (2) abdominal circumference less than the 10th percentile, (3) EFW discordance greater than or equal to 25%, or (4) UA-PI greater than the 95th percentile [40]. Given the perinatal morbidity and mortality risks in twins, particularly with FGR, uniform approach in diagnosis and screening strategy has been emphasized by ACOG, RCOG, SMFM and NICE; each type of multiple gestation screening algorithm is discussed by designated sections below [1,8].
Dichorionic diamniotic twins
Dichorionic (DC) twin pregnancies are at risk for discordant twin growth, FGR, malpresentation, and stillbirth. In addition to an early dating ultrasound and routine anatomic survey at 18-22 weeks, Dichorionic Diamniotic (Di-Di) twin surveillance recommendations include monthly growth ultrasound assessments beginning around 28 weeks. Given the increased risk for FD near term, current guidelines include the initiation of antenatal testing by 37 weeks. Such antenatal testing may include any one of the following: 1) twice weekly non-stress tests (NST) with a weekly amniotic fluid index (AFI); 2) weekly biophysical profile (BPP); or, 3) weekly modified biophysical profile (NST with an AFI) [1,43,44].
Monochorionic diamniotic twins
As with DC pregnancies, Monochorionic (MC) and thus Monochorionic Diamniotic (Mo-Di) twin pregnancies are at risk for discordant twin growth, FGR, malpresentation, and stillbirth. MC twins exhibit smaller biometry as compared to singletons and DC pregnancies [45]. Additionally, Mo-Di twin pregnancies are at risk of developing twin-twin transfusion syndrome (TTTS). In virtually all MC placentae, there are vascular connections between the two fetuses’ placental vasculature that serve as the fetal-placental circulation for gas, nutrient, and metabolite exchange. The depths and arterio-venous balance between these connections determine the risk for developing TTTS. TTTS complicates about 10-15% of MC gestations [46]. Additionally, 20% of MC pregnancies are complicated by unequally shared placental territory, leading to FGR of the twin receiving less placental blood flow. Unfortunately, there is no specific treatment available for this condition save for selective reduction by cord ablation, but close fetal surveillance can reduce poor outcomes [47]. Further complicating matters is that it may be difficult to elucidate between these two phenomena in a single pregnancy. Sophisticated fetal echocardiography and detailed ultrasound surveillance may be needed [48].
Being a monozygotic twin is in some ways the ultimate birth defect in that the developing embryo split in half. It is therefore not surprising that there are significantly more fetal congenital malformations observed in monozygotic twins [15,19]. Although the fetuses are genetically identical, they are most often not concordant for the congenital malformation [45,46,49]. Because of the increased risk of congenital heart defects with Mo-Di twins, a fetal echocardiogram should be arranged around 20-22 weeks for optimal image quality.
In aggregate, these complications result in a much higher perinatal mortality rate for MC twins. This is concordant with the observation that perinatal mortality and morbidity is highest in same sex pregnancies – two thirds of which are MC. Because of the increased risks for FGR, TTTS, and FD, surveillance in Mo-Di twin pairs is heightened. Mo-Di twin surveillance includes screening for TTTS every 2 weeks beginning at 16 weeks with monthly growth ultrasound and fluid evaluation assessments; if a significant discordance in amniotic fluid volume is noted, the sonogram may be supplemented with Doppler and/or fetal echocardiography to ascertain the etiology [1,43,44]. Because there is increased risk for FD in Mo-Di twin pairs compared to Di-Di twins, antenatal testing is recommended at 32 weeks. Additionally, given the increased risk for preterm birth, cervical length assessment should occur at 18 weeks and then as clinically indicated until 23 weeks and 6 days [50-52].
Further, MC twin gestations are at an even greater risk for maternal complications. Hypertensive complications of pregnancy are increased by a factor of 2.5. There is a 3 times increased risk of placental abruption, a 2.5 times increased risk of anemia, and 1.5 times increased risk of urinary tract infections [53]. Likewise, due to increased risk of gestational diabetes (GDM) and preeclampsia, an early Glucola screen, metabolic profile, and urine protein creatinine ratio for baseline renal function along with regular screens for bacteriuria per trimester should be considered. If normal, the 1-hour GTT test should be repeated at around 28 weeks.
Commentary on TTTS and staging
TTTS occurs in MC pregnancies when vascular flow is uneven between the two vascular beds that perfuse each fetus. Each fetus has its own vascular bed that serves as fetal placental circulation within the shared singular placenta with anastomosis between these vascular beds in three variations: artery-to-artery, vein-to-vein, or artery-to-vein. An unequal shift occurs when there is an imbalance in artery-to-vein connections between the two respective vascular beds that supply the fetuses, leading to one twin (recipient) receiving more blood flow than and from the other twin (donor). The diagnosis is staged by ultrasound findings as outlined in (Table 5) [54,55].
|
Quintero Stage |
Findings |
|
I |
Oligohydramnios¹ in the donor twin and polyhydramnios² in the recipient twin |
|
II |
No visualization of the fetal bladder in the donor twin. |
|
III |
Abnormal umbilical artery Dopplers |
|
IV |
Hydrops fetalis³ in one or both fetuses |
|
V |
Demise in one or both of the fetuses |
|
¹Maximum vertical pocket <2 cm; ²Maximum vertical pocket >8 cm; ³Ascites, pericardial effusion, pleural effusion, scalp edema in ≥ 2 compartments. |
|
Diagnosis of at least Stage 2 TTTS from week 16-26 is best managed with fetoscopic surgery to ablate (Selective Fetoscopic Laser Photocoagulation, or SFLP) connecting vessels and create two separate fetal-placental circulations. The recipient twin also undergoes an amnioreduction to add to the treatment’s success by restoring hydrostatic balance across the two amniotic sacs. These patients typically require regional anesthesia, with or without IV sedation, depending on placental location. Patients requiring fetoscopic surgery typically are admitted for postoperative observation with planned follow up imaging to gauge effectiveness of therapy within 5 days [56]. After 26 weeks of gestation, diagnosis of Stage 2 or greater TTTS is not treated with fetoscopic surgery as outcomes are similar by simple ultrasound guided amnioreduction.
The overall survival rate for Stage III without intervention is 30% [57]. Therefore, in cases with this advanced stage, it is recommended that some intervention be performed. Additionally, there is the option of cord ligation of the donor twin, which effectively terminates the donor twin. This line of therapy is not limited to TTTS but also in discordant twins with isolated severe FGR cases not meeting criteria for TTTS. These fetuses are at risk for hypoperfusion related neurologic injury or FD.
Both amnioreduction and laser ablation have risks and benefits associated with them. Risks include bleeding, infection, abruption, fetal loss, rupture of membranes, neurologic deficits in the fetuses, preterm delivery, and septostomy with both procedures. There are the added risks of anesthesia, venous thrombosis, and pulmonary edema with the laser ablation surgery. In cases where laser ablation cannot be performed for technical reasons and the clinical picture remains consistent with TTTS, amnioreduction is an option.
Data following SFLP varies, but one center reports 82% overall survival and 73% survival of both twins. Ninety-two percent of those treated result in at least one surviving twin with Quintero Stages I, II, III [58]. Outcomes are not quite as favorable with Quintero Stage IV treated by SFLP as survival of at least one twin is 85%, both twin survival 69%, and overall survival 77% [58].
Commentary on twin anemia-polycythemia sequence (TAPS)
TAPS occurs in MC twin pregnancies because of an imbalance in blood counts between fetuses. As opposed to TTTS where there is primarily a volume disparity between the twins in their respective vascular networks within the shared placenta, TAPS results from discrepancy in cellular components, namely the red blood cells, whereby one twin is rendered anemic while its counterpart is polycythemic. The anemic twin is at risk for hypoxia and impaired organ development. It will demonstrate faster than normal blood flow as measured by Doppler interrogation of the middle cerebral artery (MCA) peak systolic velocity (PSV). The polycythemic twin has slower than normal blood flow by MCA Doppler PSV and may exhibit cardiac modeling with thickening of the right ventricle (the systemic ventricle of the fetus). Unlike TTTS, TAPS does not exhibit any overt ultrasound findings and requires physician suspicion to prompt assessment of MCA Doppler [59].
While TAPS may occur randomly or sporadically, the most likely contributing risk factor for TAPS is laser surgery for TTTS. Inherently, in twins without prior history of SFLP, MCA Doppler interrogation is performed when antenatal testing is non-reassuring. Given the variance of presentation and lack of demonstration of findings germane to the Quintero staging system, clinicians developed the Leiden staging system to guide identification of physiologic findings that characterize TAPS. Leiden staging is depicted in (Table 6) [59].
|
Leiden Stage |
Findings |
|
I |
Donor MCA > 1.5 MoM, Recipient MCA-PSV < 1.0 MoM |
|
II |
Donor MCA > 1.7 MoM, Recipient MCA < 0.8 MoM |
|
III |
Stage 1 or Stage 2 with cardiac compromise* in the donor twin |
|
IV |
Donor Hydrops |
|
V |
Demise in one or both of the fetuses |
|
*Cardiac compromise = Umbilical artery absent or reversed end diastolic flow, umbilical vein pulsatile flow, increased pulsatility index (PI), Ductus Venosus (DV) reverse flow; MCA: Middle Cerebral Artery Dopplers; MoM: Multiples of the Medium. |
|
Monochorionic monoamniotic twins
The critical risk in Monochorionic Monoamniotic (Mo-Mo) twins is that of fetal cord entanglement. When twins share an amniotic sac, entanglement is almost guaranteed by mid-trimester of pregnancy and fetal movement can cause significant traction on an entangled cord. This can lead to a cutoff of oxygen to one or both fetuses. For this reason, very intensive antenatal surveillance is indicated. However, the desire to begin surveillance early must be balanced against the significant risks of extreme prematurity. Therefore, many practices recommend patients meet with neonatologists to review available data before viability. Many elect to initiate surveillance between 23- and 28-weeks’ gestation depending on their desire for intervention at increasingly premature gestational ages. Once surveillance is initiated, there is no universal agreement as to the appropriate frequency. While most of the data are anecdotal, fetal death in utero has occurred in pregnancies that have undergone fetal heart rate testing at multiple frequencies and continuously. Effectively, sampling/surveillance of the fetal heart rates may be individualized balancing the patient’s acceptance of risk vs. burden on patient’s life and ability to function with time commitments allocated to surveillance [60].
Sonographic surveillance, including arterial and venous Doppler studies and fetal interval growth, should be planned at least monthly intervals after viability. Previously, obstetricians have advocated weekly administration of antenatal corticosteroids for pregnancies at high risk for preterm birth. However, considering harm (eg, cerebral palsy, small head circumference) posed from serial steroid administration when more than two courses are given, steroids are reserved for a time when fetal heart rate abnormalities are noted or given empirically at the initiation of intensive fetal surveillance with a rescue around 32 weeks’ gestation [61,62]. In addition, Mo-Mo twins are expected to share some placental vessels. Although rare in the setting of mono-amnionicity, this poses at least a theoretical risk for TTTS. Since differential amniotic fluid volumes cannot be used to establish this diagnosis in this setting, the planned serial ultrasounds in MC twin pregnancies should be supplemented by umbilical arterial and venous Doppler studies. In addition to the above considerations, one needs to think of a possible course of action if one of the twins suffers an intrauterine demise. This would place the remaining co-twin at significant risk of embolization, which can have profound neurological and other consequences. In such an event, depending upon gestational age, the patient would either be a candidate for umbilical cord ligation or elective delivery even earlier than originally planned.
Twin reversed arterial perfusion
Twin reversed arterial perfusion (TRAP) sequence occurs in 1% of monochorionic pregnancies, which represents a 1 in 35,000 occurrence in all pregnancies. TRAP arises when one of the twins lacks a heart or at least lacks a functional heart; this acardiac twin and the shared placental circulation means the other twin’s heart must do the work of fetal-placental circulation for the pregnancy—“pump twin.” The pump twin is at risk for cardiac failure and notably the acardiac twin is poorly developed and may also lack a head, limbs, and torso with no prognosis for survival and is effectively a mass of tissue placing the pump twin at risk [63]. Identification of twin pairs affected by TRAP is pivotal to facilitate appropriate evaluation, surveillance, and referral when clinically appropriate. Many acardiac twins do not grow much and do not place significant strain on the pump twin making closely monitored expectant management possible [64]. On the contrary, when the acardiac twin mass grows in size, the pump twin’s heart may become strained and at risk for cardiac failure, hydrops and death. As this sequence is identified, either bipolar coagulation or radiofrequency ablation of the acardiac twin’s cord is paramount to effectively stop the shunting of blood into the acardac mass and generate what amounts to a healthy singleton pregnancy in the majority of cases [65,66].
Conjoined Twins
As with Mo-Mo twins that are not conjoined, there is not a universal consensus for screening and surveillance of conjoined twins with even less available literature. The prognosis for conjoined twins is usually quite poor with a survival rate of 7.5% overall and 60% in surgically separated patients. However, generally only 25% of live births end up qualifying as surgical candidates. The incidence of congenital anomalies is about 80% in conjoined twins and tend to affect female fetuses at a ratio of 3:1 [67].
An early diagnosis is necessary to allow patients to elect for early termination of pregnancy if desired given such poor prognosis. Conjoined twins are typically identifiable on prenatal ultrasonography. Diagnosis is generally easily made with early ultrasound, although the exact type is more difficult to definitively identify. A common early ultrasound finding is increased nuchal translucency. Magnetic resonance imaging can also help discern the type of conjunction, embryological anomalies, and characterizing tissue. If postnatal surgery is recommended, 3D printing can assist with surgical planning and separation [68].
Malformations frequently reported include those affecting the genitourinary tract, the central nervous system, microphthalmia, musculoskeletal system, gastrointestinal atresias, and facial clefts. Musculoskeletal anomalies are occasionally present with limb deficiency defects and polydactyly. While these anomalies are not always clear on ultrasound, they should be screened for during anatomy scans. The Mo-Mo placentation of monozygotic twins is characteristic of conjoined twins. As with other types of Mo-Mo twins, the risk of fetal cord entanglement remains. As surveillance, management, and prognosis of conjoined twins are very complicated, family prenatal counseling is recommended to aid patients in understanding the available management options.
High Order Multiples
The natural history of triplet pregnancy comes with significantly higher risk compared to twins with a mean gestational age at delivery of around 33-34 weeks. Around 7% of triplet pregnancies are lost prior to viability (22 weeks), about 5% of the remainder deliver before 28 weeks, and around 20% of triplets deliver before 32 weeks [69].
Likewise, maternal hazards of triplet pregnancy are increased including the high rate of preterm labor, increased risk of pre-eclampsia and gestational diabetes, and the need for Cesarean delivery. The management of triplet pregnancy includes close monitoring for signs and symptoms of preterm labor; prompt hospitalization with aggressive tocolysis and steroid administration for early preterm labor; serial ultrasounds for fetal growth; antenatal testing to ensure fetal well-being often with biophysical profiles at 32 weeks given the technical challenges for many outpatient settings with three fetuses on an external fetal heart rate monitor.
In triplet and higher order pregnancies, physicians are tasked with discussing multifetal pregnancy reduction to reduce the risks for the pregnant person and fetus(es) pursued with intent to achieve live birth. There is approximately a 5% loss rate associated with reduction of triplets to twins with a similar rate for patients attempting to carry a triplet pregnancy without reduction. Once twin pregnancy is achieved then counseling on expectations for twins becomes relevant with a mean gestational age at delivery of around 35-36 weeks. As one would expect, there is conflicting data and some controversy over whether multifetal pregnancy reduction is justified in triplet pregnancy solely on medical grounds. Although the gestational age at delivery, birth weight, and short-term morbidities are all clearly improved, the improvements in survival and long-term morbidities are much less obvious and not consistent [70].
Maternal Considerations in Multiples
Anemia in twin pregnancy
Inherently, the fetal needs are duplicated or triplicated in twin and triplet pregnancies [1]. Folate supplementation in twins and high order multiples has been investigated given the observation of megaloblastic anemia. Conversely, iron supplementation recommendations have been evaluated due to observation of microcytic anemia in multiple gestation. That said, retrospective case-control study data in twins versus singletons did not exhibit variation in maternal serum hemoglobin concentrations when controlling for gestational age [71,72]. A singular recent randomized controlled trial indicated positive impact on heme profiles in twin pregnancy [73].
While there remains some inherent inconsistency in evidence, risk-benefit considerations appear to be tipped in favor of encouraging presence of dietary iron in multiple gestation. Our most current practice recommendation is to encourage a diet rich in iron along with taking the prenatal vitamin daily. Checking hemoglobin/hematocrit and iron profile on intake and at the third trimester lab interval is likely a good strategy and is what is practiced at our institution.
Hypertension in twin/multiple pregnancy
Any hypertensive disorder—preeclampsia, gestational hypertension, and poorly controlled chronic hypertension—demonstrates increased incidence with increasing fetal number [1]. Twin pregnancies confer 2-3-fold risk for preeclampsia compared to singleton pregnancy [74]. Data from retrospective cohorts have been used to generate a better predictive measure accounting for additional variables (eg, serum creatinine, uric acid, mean platelet volume, high-density lipoprotein, lactate dehydrogenase, fibrinogen, primiparity, prepregnancy body mass index, and regular prenatal care) [75]. Clearly, heightened awareness in prenatal visits and patients understanding precautions are of importance. Monozygosity has been postulated as posing higher risk for hypertensive disorders of pregnancy but data are not consistent with the association [74,75].
Diabetes and gestational diabetes in twin/multiple pregnancy
Pregnancies of multiples are at a higher risk for the development of GDM, thought to be due to larger developing placenta mass as well as in conjunction with other risks associated with multiple gestations such as advanced maternal age and increased gestational weight gain [1,75,76]. Indeed, some reports have shown up to a 2 to 3-fold increase risk in the development of GDM in multiples [77]. Further, the highest rates of GDM in multiples has been shown in African American populations [78]. However, it is unclear if GDM has the same effects on accelerated fetal growth as it does in singleton pregnancies [79].
Prevention of Preterm Birth in Twins and Multiples
Obstetricians must be aware of the evidence-based tools for prevention of preterm delivery, particularly for multiple gestation. Spontaneous preterm delivery is rooted in a spectrum of etiologies from infections, cervical insufficiency, and preterm labor.
Infections
Intrauterine and pelvic infections have a well-established association with preterm delivery. Attention to symptoms of urinary tract infections and bacterial vaginosis are important and should prompt evaluation via urinalysis and urine culture or wet mount, respectively as clinically appropriate. Treatment of BV when symptomatic only and urinary tract infection (UTI) whether asymptomatic or not may help reduce preterm birth [80-84].
Cervical shortening
Vaginal progesterone remains a staple for prevention of preterm birth in women who demonstrate cervical length shortening on ultrasound as defined by closed functional length measured less than 2.5 cm, regardless of their preterm birth history. While most data regarding the effectiveness of vaginal progesterone for short cervix are derived from studies in singleton pregnancies [85-89], the therapy is relatively low cost (when compared to the cost of preterm birth and neonatal care) and poses little to no appreciable risk to the patient [90]. To this effect, a meta-analysis in 2014 on 1731 twin pregnancies from seven randomized controlled trials on vaginal progesterone used in twin pregnancy complicated by short cervix demonstrated a reduction in composite adverse perinatal outcome (RR=0.57, 95 CI 0.47-0.70) with number needed to treat of 10 twin pregnancies [91]. A similar meta analysis showed vaginal progesterone in twins with short cervix to reduce preterm birth (RR= 0.67, 95% CI 0.49-0.91, NNT=6) and neonatal morbidities and mortality (RR=0.49, 95% CI 0.33-0.69; NNT=6 [92]. Accordingly, we recommend vaginal progesterone supplementation in twin pregnancy complicated by short cervix.
Cervical insufficiency
Historically, cerclage has been considered as “not indicated in twin or other multiple pregnancies” as based on lack of randomized studies demonstrating benefit when compared with proper controls [93]. There is only one randomized controlled trial (RCT) on physical exam indicated cerclage in twins with dilated cervix before 24 weeks to evaluate benefit [94], noting this study has been critiqued as not having adequate power to address the question. Nonetheless, to be consistent with current expert opinion and lack of data our recommendation is that cerclage is not indicated in twin pregnancy [93,94].
fFN and preterm labor
Fetal fibronectin fFN has been studied extensively for the prediction of preterm delivery in singletons, noting the predictive value largely rests in its negative predictive value (NPV). Similarly, data on cohort studies in twins demonstrate only 66.7% positive predictive value (PPV) but a NPV of 97.2%. Hence data show that while fFN is not a diagnostic tool for preterm labor it remains a very effective tool when negative to provide reassurance that preterm delivery is not imminent in setting of symptoms [95]. Meta-analysis utilizing data from symptomatic women with multiple gestation showed only 1.6% of those with negative cervicovaginal fetal fibronectin will deliver within the next week [96].
Intrapartum Management of Multifetal Pregnancies: Delivery and Mode
In addition to antenatal surveillance as outlined above, the remaining question around multiple pregnancies involves delivery management. The optimal timing of delivery for multiples is varied and depends on the chorionicity and amnionicity of the gestation, as well as current fetal and maternal complications. In general, perinatal mortality increases beyond 37 weeks in twin gestations [97,98]. The current data proposes that MC twins deliver between 32-37 weeks, while DC twins deliver between 34-38 weeks [1,97-101], with uncomplicated gestations in the latter half of those ranges [99]. Beyond 38 weeks, the risk of perinatal death outweighs the risk of prematurity [100,101]. Placental sharing between MC twins increases the risk of fetal demise, and thus earlier delivery is warranted [101].
The second question is the mode of delivery: Should multiples be scheduled Cesarean deliveries, or should vaginal delivery be attempted? Here the data are mixed. Some studies have shown that planned Cesarean delivery has been associated with higher five-minute APGAR scores [7] and that planned, pre-labor Cesarean delivery decreases the risk of fetal death for the second twin [100-102]. This may or may not be related to inter-twin delivery time, with the current literature inconclusive [97-102]. Other studies have shown that planned Cesarean delivery does not improve perinatal mortality as compared to vaginal delivery [97-102].
Delayed Interval Delivery of the Second Twin (Periviable/Previable Twins)
Delayed delivery of the second twin is a practice that has been attempted with limited data with the intent to improve the outcome of the second twin when delivery of the first twin occurs in the second trimester particularly in the previable or periviable periods. Neonatal outcomes are inherently improved with increasing gestational age at delivery particularly as a pregnancy increases in gestational age in the pre-viable and/or periviable gestational age windows. Conversely, delaying delivery in setting of a dilated cervix and delivery of one of the fetuses in multiple gestation presents risk for maternal infection and hemorrhage for the pregnant patient. While outcome data vary widely given small sample sizes of published cohorts, latency between delivery of the second twin ranges from 0->150 days [103-106].
Review of literature, while limited given the rarity of such deliveries, would lead to a recommendation for individualized patient-doctor counseling and joint decision-making. Interventions such as high ligation of the cord of the delivered twin, administration of latency antibiotics to promote increased time for delay in interval delivery, and cerclage have been offered, performed and published, noting there are no well-designed RCTs for any of these interventions in the specific setting of delayed interval delivery of the second twin [103-107].
Key Updates and Listed Summary of Recommendations
- Supplement folate pre- and periconception [Level Ia; A];
- Supplement iron and folate in the mid- and late trimesters [Level IIb; B].
- First trimester ultrasound remains paramount in discerning chorionicity in twins and high order multiple gestations [Level II-2A; B].
- Multiple marker screening by either first trimester screen or second trimester Maternal Serum Screen must be interpreted with caution as altered serum levels generated by an abnormal fetus may be “normalized” by the other twin. Serum screening is never valid in triplets or other higher order pregnancies [Level II; B].
- Each amniotic sac should be sampled in a diagnostic amniocentesis of multiple gestation except with a monochorionic twin pair in that monochorionicity was confirmed in the first trimester and growth is concordant. [Level II2b; B].
- In multiple gestations, women should increase their daily intake by 300 calories/fetus in the first trimester, 340 calories/fetus in the second trimester, and 452 calories/fetus in the third trimester [Level IV; C].
- Iron-rich diet in addition to the prenatal vitamin may be beneficial [Level Ib; A].
- Patients with twins/multiples should be advised to consume ≥100 gm protein daily [Level IV; C].
- Fetal fibronectin in setting of threatened preterm labor remains of high negative predictive value (~97%) for delivery within 2 weeks of sampling [Level IIb; B].
- Cervical length monitoring is of limited utility in twin/multiple gestation:
- Cervical cerclage has not been demonstrated to be of benefit for either history-based (prophylactic) or short cervix on ultrasound (ultrasound-indicated) and may pose risk of increased preterm delivery in twins and/or multiples [Level IIa/b; B].
- Vaginal progesterone for treatment of short cervix has not been demonstrated to be of clear benefit in twins and multiple gestation [Level IIa; B].
- Of twins with imminent risk for preterm birth for any indication from 23-34 weeks’ gestational age, antenatal corticosteroids are well-established as beneficial to reduce fetal morbidity and mortality [Level 1b; A].
- Serial growth evaluation by ultrasound biometry is essential for management of all twin and multiple gestations given risk for fetal growth restriction and discordant twin pairs [Level III; B].
- Discordant twin pairs should receive antenatal testing until delivery, noting timing of delivery should be based on UA Doppler studies (when indicated for FGR), antenatal testing results, and other medical indications as appropriate for that comorbidity (eg, preeclampsia, diabetes, hypertensive disorders, renal disease) [Level III; B].
- Monochorionic twin pregnancies are at risk for TTTS and as such are recommended to have limited ultrasounds biweekly (ever 2 weeks) in the mid- and late-trimesters from 16 weeks to delivery along with antenatal testing beginning at 32 weeks until delivery [Level III; B].
- TTTS complicates 10-15% of monochorionic twin gestations [Level II; B]
- Identification of twin pairs affected by TTTS, Twin Reverse Arterial Perfusion (TRAP), Twin Anemia Polycythemia Sequence (TAPS), and selected fetal growth restriction is best for outcomes when identified early in onset to facilitate appropriate evaluation, surveillance, and referral when clinically appropriate [Level IV; C].
- Untreated TTTS is associated with fetal mortality of 60-100% [Level II; B]
- The Eurofetus study demonstrated that fetoscopic laser surgery generates more favorable outcomes compared to serial amnioreduction for TTTS when apparent as a stage II case between 16-26 weeks’ gestational age (66% vs. 57%); [Level II; B].
- Intrapartum monitoring should be continuous in multiple gestation; [Level III; B].
- Data indicates uncomplicated monochorionic-diamniotic twin pregnancies should be delivered at 37 weeks if not indicated sooner [Level III; B].
- Evidence supports delivery of monoamniotic twin pairs at 32-34 weeks by cesarean delivery given risk for stillbirth and inter-locking twins in parturition [Level III; B].
- The stillbirth rate of uncomplicated DC twins at 38 weeks matches singleton stillbirth rate at 42 weeks. Hence, delivery of uncomplicated dichorionic twins appears to be best-timed for 38 weeks, with some experts suggesting delivery at 37 weeks or shortly thereafter (by 38 weeks) [Level III; B].
- There appears to be unnecessary risk of prematurity when delivering uncomplicated DC twins prior to 36 weeks completed gestational age [Level III; B].
- Delivery of uncomplicated triplets is generally recommended by 35 weeks by cesarean except in the instance of an obstetrician experienced with vaginal delivery and the patient has been counseled appropriately regarding risks [level IIb, B].
- Delayed interval delivery may be considered in periviable or severely preterm pregnancies, noting monochorionicity, chorioamnionitis, preeclampsia and abruption are representations of many potential contraindications [Level IIb; B].
- Oxytocin infusion prophylactically in the third stage of labor to prevent postpartum hemorrhage [Level Ia; A].
Concluding Remarks
All obstetricians will encounter twins and may even encounter higher order multiples in their careers. Until care can be transferred to a provider who is comfortable managing the associated increased complications of such pregnancies, practitioners should be generally aware of multiples and the standard of care. Here, we reviewed the current literature in management of pregnancies affected by multiple gestations and outlined current management practices that are considered best practices in the setting of conflicting data, controversies, and limitations to current understanding, namely, complications associated with advanced chorionicity and amnioncity. We discussed the importance of close antepartum surveillance and outlined the differences in management among the different types of multiple gestations. We also identified areas of research still needed to provide the best care for this patient population.
Author Contributions
Jeffrey Morgan Denney, MD, MS, FACOG: Literature review, Overview of multiples; Biology of twinning; Antepartum Twin Management: Surveillance of Growth and Fetal Status; Dichorionic Diamniotic Twins; Monochorionic Diamniotic twins; Commentary on TTTS and Staging Commentary on TAPS; Monochorionic monoamniotic twins; TRAP sequence; High Order Multiples; Antenatal testing; Maternal hypertension; infection/UTI; Iron supplementation; short cervix and progesterone; cerclage for cervical insufficiency; fFN; Delayed interval delivery; Manuscript editing; Back end work; Sophia Nicole Brancazio, MD, MPH: Literature review; Manuscript editing; Introduction; Abstract; Conclusion; Tables and figures; Intrapartum management; Back end work; Lexi Rose Frankel, MD: Genetic and antenatal testing; Manuscript editing; Kristen H. Quinn, MD: Overview of multiples; Biology of twinning; Antepartum Twin Management: Surveillance of Growth and Fetal Status; Dichorionic Diamniotic Twins; Monochorionic Diamniotic twins; Commentary on TTTS and Staging Commentary on TAPS; Monochorionic monoamniotic twins; High Order Multiples; Tables and figures; Manuscript editing.
Funding
Not applicable.
Institutional Review Board Statement
Not applicable
Acknowledgements
Thank you to the Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine. Thank you to our incredible sonographers at our Comprehensive Fetal Care Center in educating our trainees and providing outstanding images. Prior to peer review: this article has been published online by Preprints as follows: Denney, J. M.; Brancazio, S. N.; Frankel, L. R.; Quinn, K. H. Narrative Review on Multiple Gestation: A Clinician’s Pocket Guide to Navigate Management of Multiple Gestation with an Evidence-Based Perspective. Preprints 2024, 2024041429. https://doi.org/10.20944/preprints202404.1429.v1.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
AFI: Amniotic Fluid Index; AFP: Alphafeto Protein; BPP: Biophysical Profile; CRL: Crown Rump Length; DC: Dichorionic; Di-Di: Dichorionic Diamniotic; EFW: Estimated Fetal Weight; FD: Fetal Demise; FGR: Fetal Growth Restriction; FSH: Follicle Stimulating Hormone; HCG: Human Chorionic Gonadotropin; LMP: Last Menstrual Period; MC: Monochorionic; MCA: Middle Cerebral Artery; Mo-Di: Monochorionic Diamniotic; Mo-Mo: Monochorionic Monoamniotic; NST: Nonstress Test; NT: Nuchal Translucency; ONTD: Open Neural Tube Defects; PAPP-A: Pregnancy Associated Plasma Protein-A; PI: Pulsatility Index; PSV: Peak Systolic Velocity; RCT: Randomized Controlled Trial; sFGR: Selective Fetal Growth Restriction; SFLP: Selective Fetoscopic Laser Photocoagulation; T21: Trisomy 21; TAPS: Twin Anemia-Polycythemia Sequence; tFF: Total Fetal Fraction; TRAP: Twin Reverse Arterial Perfusion; TTTS: Twin-Twin Transfusion Syndrome; UA: Umbilical Artery; USPSTF: United States Preventative Services Task Force
References
2. Oepkes D, Sueters M. Antenatal fetal surveillance in multiple pregnancies. Best Pract Res Clin Obstet Gynaecol. 2017 Jan;38:59-70.
3. Owen DJ, Wood L, Neilson JP. Antenatal care for women with multiple pregnancies: the Liverpool approach. Clin Obstet Gynecol. 2004 Mar;47(1):263-71.
4. Audibert F, Gagnon A. No. 262-Prenatal Screening for and Diagnosis of Aneuploidy in Twin Pregnancies. J Obstet Gynaecol Can. 2017 Sep;39(9):e347-61.
5. Vogel JP, Torloni MR, Seuc A, Betrán AP, Widmer M, Souza JP, et al. Maternal and perinatal outcomes of twin pregnancy in 23 low- and middle-income countries. PLoS One. 2013 Aug 1;8(8):e70549.
6. Rao A, Sairam S, Shehata H. Obstetric complications of twin pregnancies. Best Pract Res Clin Obstet Gynaecol. 2004 Aug;18(4):557-76.
7. Malone F, D’Alton M. Multiple Gestation: Clinical Characteristics and Management. In Lockwood C, Moore T, Copel J, Silver R, Resnik R, Dugoff L, et al. Eds. Creasy and Resnik’s Maternal-fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2018. pp. 660-86.
8. Gezer A, Rashidova M, Güralp O, Oçer F. Perinatal mortality and morbidity in twin pregnancies: the relation between chorionicity and gestational age at birth. Arch Gynecol Obstet. 2012 Feb;285(2):353-60.
9. Santana DS, Surita FG, Cecatti JG. Multiple Pregnancy: Epidemiology and Association with Maternal and Perinatal Morbidity. Rev Bras Ginecol Obstet. 2018 Sep;40(9):554-62.
10. National Collaborating Centre for Women's and Children's Health (UK). Multiple Pregnancy: The Management of Twin and Triplet Pregnancies in the Antenatal Period. London: RCOG Press; 2011, revised 2019. (NICE Clinical Guidelines, No. 129).
11. Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: Final Data for 2021. Natl Vital Stat Rep. 2023 Jan;72(1):1-53.
12. McNamara HC, Kane SC, Craig JM, Short RV, Umstad MP. A review of the mechanisms and evidence for typical and atypical twinning. Am J Obstet Gynecol. 2016 Feb;214(2):172-91.
13. Cochrane AL. 1931-1971: a critical review, with particular reference to the medical profession. In: Medicines for the Year 2000. Office to Health Economics; London: 1979:1-11.
14. Ransom SB, Studdert DM, Dombrowski MP, Mello MM, Brennan TA. Reduced medicolegal risk by compliance with obstetric clinical pathways: a case--control study. Obstet Gynecol. 2003 Apr;101(4):751-5.
15. Mogollón F, Casas-Vargas A, Rodríguez F, Usaquén W. Twins from different fathers: A heteropaternal superfecundation case report in Colombia. Biomedica. 2020 Dec 2;40(4):604-8.
16. Hirshberg A, Dugoff L. First-trimester Ultrasound and Aneuploidy Screening in Multifetal Pregnancies. Clin Obstet Gynecol. 2015 Sep;58(3):559-73.
17. Maruotti GM, Saccone G, Morlando M, Martinelli P. First-trimester ultrasound determination of chorionicity in twin gestations using the lambda sign: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016 Jul;202:66-70.
18. Sperling L, Tabor A. Twin pregnancy: the role of ultrasound in management. Acta Obstet Gynecol Scand. 2001 Apr;80(4):287-99.
19. Lu J, Ting YH, Leung TY. Determining chorionicity and amnionicity in twin pregnancies: Pitfalls. Best Pract Res Clin Obstet Gynaecol. 2022 Nov;84:2-16.
20. Cleary-Goldman J, Berkowitz RL. First trimester screening for Down syndrome in multiple pregnancy. Semin Perinatol. 2005 Dec;29(6):395-400.
21. Rosner JY, Fox NS, Saltzman D, Klauser CK, Rebarber A, Gupta S. Abnormal Biochemical Analytes Used for Aneuploidy Screening and Adverse Pregnancy Outcomes in Twin Gestations. Am J Perinatol. 2015 Dec;32(14):1331-5.
22. Hedriana H, Martin K, Saltzman D, Billings P, Demko Z, Benn P. Cell-free DNA fetal fraction in twin gestations in single-nucleotide polymorphism-based noninvasive prenatal screening. Prenat Diagn. 2020 Jan;40(2):179-84.
23. Casasbuenas A, Wong AE, Sepulveda W. Nuchal translucency thickness in monochorionic multiple pregnancies: value in predicting pregnancy outcome. J Ultrasound Med. 2008 Mar;27(3):363-9.
24. Dugoff L, Koelper NC, Chasen ST, Russo ML, Roman AS, Limaye MA, et al. Cell-free DNA screening for trisomy 21 in twin pregnancy: a large multicenter cohort study. Am J Obstet Gynecol. 2023 Oct;229(4):435.e1-435.e7.
25. Fosler L, Winters P, Jones KW, Curnow KJ, Sehnert AJ, Bhatt S, et al. Aneuploidy screening by non-invasive prenatal testing in twin pregnancy. Ultrasound Obstet Gynecol. 2017 Apr;49(4):470-7.
26. Kim MJ, Kim HM, Cha HH, Kim JI, Seong WJ. Correlation between serum markers in the second trimester and preterm birth before 34 weeks in asymptomatic twin pregnancies. Int J Gynaecol Obstet. 2022 Feb;156(2):355-60.
27. Delisle MF, Brosseuk L, Wilson RD. Amniocentesis for twin pregnancies: is alpha-fetoprotein useful in confirming that the two sacs were sampled? Fetal Diagn Ther. 2007;22(3):221-5.
28. Lenis-Cordoba N, Sánchez MÁ, Bello-Muñoz JC, Sagalá-Martinez J, Campos N, Carreras-Moratonas E, et al. Amniocentesis and the risk of second trimester fetal loss in twin pregnancies: results from a prospective observational study. J Matern Fetal Neonatal Med. 2013 Oct;26(15):1537-41.
29. Navaratnam K, Khairudin D, Chilton R, Sharp A, Attilakos G, Stott D, et al. Foetal loss after chorionic villus sampling and amniocentesis in twin pregnancies: A multicentre retrospective cohort study. Prenat Diagn. 2022 Nov;42(12):1554-61.
30. Appelman Z, Furman B. Invasive genetic diagnosis in multiple pregnancies. Obstet Gynecol Clin North Am. 2005 Mar;32(1):97-103.
31. Whitaker KM, Baruth M, Schlaff RA, Talbot H, Connolly CP, Liu J, et al. Provider advice on physical activity and nutrition in twin pregnancies: a cross-sectional electronic survey. BMC pregnancy and childbirth. 2019 Dec;19:1-4.
32. Georgieff MK. Iron deficiency in pregnancy. Am J Obstet Gynecol. 2020 Oct;223(4):516-24.
33. Bricker L. Optimal antenatal care for twin and triplet pregnancy: the evidence base. Best Pract Res Clin Obstet Gynaecol. 2014 Feb;28(2):305-17.
34. Ijzerman RG, Boomsma DI, Stehouwer CD. Intrauterine environmental and genetic influences on the association between birthweight and cardiovascular risk factors: studies in twins as a means of testing the fetal origins hypothesis. Paediatr Perinat Epidemiol. 2005 Jan;19 Suppl 1:10-4.
35. Briffa C, Stirrup O, Huddy C, Richards J, Shetty S, Reed K, et al. Twin chorionicity-specific population birth-weight charts adjusted for estimated fetal weight. Ultrasound Obstet Gynecol. 2021 Sep;58(3):439-49.
36. Stirrup OT, Khalil A, D'Antonio F, Thilaganathan B; Southwest Thames Obstetric Research Collaborative (STORK). Fetal growth reference ranges in twin pregnancy: analysis of the Southwest Thames Obstetric Research Collaborative (STORK) multiple pregnancy cohort. Ultrasound Obstet Gynecol. 2015 Mar;45(3):301-7.
37. Kalafat E, Sebghati M, Thilaganathan B, Khalil A; Southwest Thames Obstetric Research Collaborative (STORK). Predictive accuracy of Southwest Thames Obstetric Research Collaborative (STORK) chorionicity-specific twin growth charts for stillbirth: a validation study. Ultrasound Obstet Gynecol. 2019 Feb;53(2):193-9.
38. Hamilton EF, Platt RW, Morin L, Usher R, Kramer M. How small is too small in a twin pregnancy? Am J Obstet Gynecol. 1998 Sep;179(3 Pt 1):682-5.
39. Khalil A, Rodgers M, Baschat A, Bhide A, Gratacos E, Hecher K, et al. ISUOG Practice Guidelines: role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol. 2016 Feb;47(2):247-63.
40. Khalil A, Beune I, Hecher K, Wynia K, Ganzevoort W, Reed K, et al. Consensus definition and essential reporting parameters of selective fetal growth restriction in twin pregnancy: a Delphi procedure. Ultrasound Obstet Gynecol. 2019 Jan;53(1):47-54.
41. American College of Obstetricians and Gynecologists. Antepartum Fetal Surveillance. Obstet & Gynecol. 2014;137(6):e116-27.
42. Indications for Outpatient Antenatal Fetal Surveillance: ACOG Committee Opinion, Number 828. Obstet Gynecol. 2021 Jun 1;137(6):e177-97.
43. Stirrup OT, Khalil A, D'Antonio F, Thilaganathan B; Southwest Thames Obstetric Research Collaborative (STORK). Fetal growth reference ranges in twin pregnancy: analysis of the Southwest Thames Obstetric Research Collaborative (STORK) multiple pregnancy cohort. Ultrasound Obstet Gynecol. 2015 Mar;45(3):301-7.
44. Grewal J, Grantz KL, Zhang C, Sciscione A, Wing DA, Grobman WA, et al. Cohort Profile: NICHD Fetal Growth Studies-Singletons and Twins. Int J Epidemiol. 2018 Feb 1;47(1):25-251.
45. Xia YQ, Lyu SP, Zhang J, Chen YT, Gao L, Zhao AD, et al. Development of fetal growth charts in twins stratified by chorionicity and mode of conception: a retrospective cohort study in China. Chin Med J (Engl). 2021 Jul 7;134(15):1819-27.
46. Chang YL, Chao AS, Chang SD, Cheng PJ, Li WF, Hsu CC. Incidence, prognosis, and perinatal outcomes of and risk factors for severe twin-twin transfusion syndrome with right ventricular outflow tract obstruction in the recipient twin after fetoscopic laser photocoagulation. BMC Pregnancy Childbirth. 2022 Apr 15;22(1):326.
47. Chiu LC, Chang YL, Chao AS, Chang SD, Cheng PJ, Liao YC. Effect of Gestational Age at Fetoscopic Laser Photocoagulation on Perinatal Outcomes for Patients with Twin-Twin Transfusion Syndrome. J Clin Med. 2023 Feb 28;12(5):1900.
48. Roman A, Saccone G, Dude CM, Ward A, Anastasio H, Dugoff L, et al. Midtrimester transvaginal ultrasound cervical length screening for spontaneous preterm birth in diamniotic twin pregnancies according to chorionicity. Eur J Obstet Gynecol Reprod Biol. 2018 Oct;229:57-63.
49. Klein K, Gregor H, Hirtenlehner-Ferber K, Stammler-Safar M, Witt A, Hanslik A, et al. Prediction of spontaneous preterm delivery in twin pregnancies by cervical length at mid-gestation. Twin Res Hum Genet. 2008 Oct;11(5):552-7.
50. Khalil MI, Alzahrani MH, Ullah A. The use of cervical length and change in cervical length for prediction of spontaneous preterm birth in asymptomatic twin pregnancies. Eur J Obstet Gynecol Reprod Biol. 2013 Jul;169(2):193-6.
51. Melamed N, Pittini A, Hiersch L, Yogev Y, Korzeniewski SJ, Romero R, et al. Do serial measurements of cervical length improve the prediction of preterm birth in asymptomatic women with twin gestations? Am J Obstet Gynecol. 2016 Nov;215(5):616.e1-616.e14.
52. Bamberg C, Hecher K. Update on twin-to-twin transfusion syndrome. Best Pract Res Clin Obstet Gynaecol. 2019 Jul;58:55-65.
53. Bamberg C, Hecher K. Twin-to-twin transfusion syndrome: Controversies in the diagnosis and management. Best Pract Res Clin Obstet Gynaecol. 2022 Nov;84:143-54.
54. Sacco A, Van der Veeken L, Bagshaw E, Ferguson C, Van Mieghem T, David AL, et al. Maternal complications following open and fetoscopic fetal surgery: A systematic review and meta-analysis. Prenat Diagn. 2019 Mar;39(4):251-68.
55. Baschat AA, Barber J, Pedersen N, Turan OM, Harman CR. Outcome after fetoscopic selective laser ablation of placental anastomoses vs equatorial laser dichorionization for the treatment of twin-to-twin transfusion syndrome. Am J Obstet Gynecol. 2013 Sep;209(3):234.e1-8.
56. Cincinnati Fetal Center. Volumes & Outcomes Summary 2020. https://www.cincinnatichildrens.org/-/media/cincinnati%20childrens/home/service/f/fetal-care/conditions/2020%20volumesoutcomes_final.pdf
57. Moldenhauer JS, Johnson MP. Diagnosis and Management of Complicated Monochorionic Twins. Clin Obstet Gynecol. 2015 Sep;58(3):632-42.
58. Quinn KH, Cao CT, Lacoursiere DY, Schrimmer D. Monoamniotic twin pregnancy: continuous inpatient electronic fetal monitoring-an impossible goal? Am J Obstet Gynecol. 2011 Feb;204(2):161.e1-6.
59. Wapner RJ, Sorokin Y, Thom EA, Johnson F, Dudley DJ, Spong CY, et al. Single versus weekly courses of antenatal corticosteroids: evaluation of safety and efficacy. Am J Obstet Gynecol. 2006 Sep;195(3):633-42.
60. Committee on Obstetric Practice. Committee Opinion No. 713: Antenatal Corticosteroid Therapy for Fetal Maturation. Obstet Gynecol. 2017 Aug;130(2):e102-9.
61. Post A, Heyborne K. Managing Monoamniotic Twin Pregnancies. Clin Obstet Gynecol. 2015 Sep;58(3):643-53.
62. Van Mieghem T, Abbasi N, Shinar S, Keunen J, Seaward G, Windrim R, et al. Monochorionic monoamniotic twin pregnancies. Am J Obstet Gynecol MFM. 2022 Mar;4(2S):100520.
63. Vitucci A, Fichera A, Fratelli N, Sartori E, Prefumo F. Twin Reversed Arterial Perfusion Sequence: Current Treatment Options. Int J Womens Health. 2020 May 28;12:435-43.
64. Jelin E, Hirose S, Rand L, Curran P, Feldstein V, Guevara-Gallardo S, et al. Perinatal outcome of conservative management versus fetal intervention for twin reversed arterial perfusion sequence with a small acardiac twin. Fetal Diagn Ther. 2010;27(3):138-41.
65. Cabassa P, Fichera A, Prefumo F, Taddei F, Gandolfi S, Maroldi R, et al. The use of radiofrequency in the treatment of twin reversed arterial perfusion sequence: a case series and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2013 Feb;166(2):127-32.
66. Prefumo F, Fichera A, Zanardini C, Frusca T. Fetoscopic cord transection for treatment of monoamniotic twin reversed arterial perfusion sequence. Ultrasound Obstet Gynecol. 2014 Feb;43(2):234-5.
67. Oostra RJ, Schepens-Franke AN, Magno G, Zanatta A, Boer LL. Conjoined twins and conjoined triplets: At the heart of the matter. Birth Defects Res. 2022 Jul 15;114(12):596-610.
68. Spitz L. Conjoined twins. Prenat Diagn. 2005 Sep;25(9):814-9.
69. Dias T, Akolekar R. Timing of birth in multiple pregnancy. Best Pract Res Clin Obstet Gynaecol. 2014 Feb;28(2):319-26.
70. Mhatre M, Craigo S. Triplet pregnancy: What do we tell the prospective parents. Prenat Diagn. 2021 Nov;41(12):1593-601.
71. Dera-Szymanowska A, Filipowicz D, Misan N, Szymanowski K, Chillon TS, Asaad S, et al. Are Twin Pregnancies at Higher Risk for Iron and Calcium Deficiency than Singleton Pregnancies? Nutrients. 2023 Sep 18;15(18):4047.
72. Blickstein I, Goldschmit R, Lurie S. Hemoglobin levels during twin vs. singleton pregnancies. Parity makes the difference. J Reprod Med. 1995 Jan;40(1):47-50.
73. Shinar S, Skornick-Rapaport A, Maslovitz S. Iron Supplementation in Twin Pregnancy - The Benefit of Doubling the Iron Dose in Iron Deficient Pregnant Women: A Randomized Controlled Trial. Twin Res Hum Genet. 2017 Oct;20(5):419-24.
74. Chantanahom N, Phupong V. Clinical risk factors for preeclampsia in twin pregnancies. PLoS One. 2021 Apr 15;16(4):e0249555.
75. Han Q, Zheng S, Chen R, Zhang H, Yan J. A New Model for the Predicting the Risk of Preeclampsia in Twin Pregnancy. Front Physiol. 2022 Apr 8;13:850149.
76. Simões T, Queirós A, Correia L, Rocha T, Dias E, Blickstein I. Gestational diabetes mellitus complicating twin pregnancies. J Perinat Med. 2011 Jul;39(4):437-40.
77. Dimitris MC, Kaufman JS, Bodnar LM, Platt RW, Himes KP, Hutcheon JA. Gestational Diabetes in Twin Versus Singleton Pregnancies With Normal Weight or Overweight Pre-Pregnancy Body Mass Index: The Mediating Role of Mid-Pregnancy Weight Gain. Epidemiology. 2022 Mar 1;33(2):278-86.
78. Rauh-Hain JA, Rana S, Tamez H, Wang A, Cohen B, Cohen A, et al. Risk for developing gestational diabetes in women with twin pregnancies. J Matern Fetal Neonatal Med. 2009 Apr;22(4):293-9.
79. Ashwal E, Berger H, Hiersch L, Yoon EW, Zaltz A, Shah B, et al. Gestational diabetes and fetal growth in twin compared with singleton pregnancies. Am J Obstet Gynecol. 2021 Oct;225(4):420.e1-420.e13.
80. Nadeau HC, Subramaniam A, Andrews WW. Infection and preterm birth. Semin Fetal Neonatal Med. 2016 Apr;21(2):100-5.
81. Denney JM, Culhane JF. Bacterial vaginosis: a problematic infection from both a perinatal and neonatal perspective. Semin Fetal Neonatal Med. 2009 Aug;14(4):200-3.
82. US Preventive Services Task Force; Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, et al. Screening for Bacterial Vaginosis in Pregnant Persons to Prevent Preterm Delivery: US Preventive Services Task Force Recommendation Statement. JAMA. 2020 Apr 7;323(13):1286-92.
83. Smaill FM, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev. 2019 Nov 25;2019(11):CD000490.
84. Twin and Triplet Pregnancy. London: National Institute for Health and Care Excellence (NICE); 2019. PMID: 31513365.
85. Care A, Nevitt SJ, Medley N, Donegan S, Good L, Hampson L, et al. Interventions to prevent spontaneous preterm birth in women with singleton pregnancy who are at high risk: systematic review and network meta-analysis. BMJ. 2022 Feb 15;376:e064547.
86. Conde-Agudelo A, Romero R, Da Fonseca E, O'Brien JM, Cetingoz E, Creasy GW, et al. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: updated indirect comparison meta-analysis. Am J Obstet Gynecol. 2018 Jul;219(1):10-25.
87. EPPPIC Group. Evaluating Progestogens for Preventing Preterm birth International Collaborative (EPPPIC): meta-analysis of individual participant data from randomised controlled trials. Lancet. 2021 Mar 27;397(10280):1183-94.
88. Romero R, Conde-Agudelo A, Da Fonseca E, O'Brien JM, Cetingoz E, Creasy GW, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Am J Obstet Gynecol. 2018 Feb;218(2):161-80.
89. Norman JE, Marlow N, Messow CM, Shennan A, Bennett PR, Thornton S, et al. Vaginal progesterone prophylaxis for preterm birth (the OPPTIMUM study): a multicentre, randomised, double-blind trial. Lancet. 2016 May 21;387(10033):2106-16.
90. El-Refaie W, Abdelhafez MS, Badawy A. Vaginal progesterone for prevention of preterm labor in asymptomatic twin pregnancies with sonographic short cervix: a randomized clinical trial of efficacy and safety. Arch Gynecol Obstet. 2016 Jan;293(1):61-7.
91. Schuit E, Stock S, Rode L, Rouse DJ, Lim AC, Norman JE, et al. Effectiveness of progestogens to improve perinatal outcome in twin pregnancies: an individual participant data meta-analysis. BJOG. 2015 Jan;122(1):27-37.
92. Romero R, Nicolaides K, Conde-Agudelo A, Tabor A, O'Brien JM, Cetingoz E, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: a systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012 Feb;206(2):124.e1-19.
93. Berghella V, Roman A. Cerclage in twins: we can do better! Am J Obstet Gynecol. 2014 Jul;211(1):5-6.
94. Roman A, Calluzzo I, Fleischer A, Rochelson B.Physical examination indicated cerclage in twin pregnancy. Am J Obstet Gynecol. 2014;210:S391-2.
95. Fuchs F, Lefevre C, Senat MV, Fernandez H. Accuracy of fetal fibronectin for the prediction of preterm birth in symptomatic twin pregnancies: a pilot study. Sci Rep. 2018 Feb 1;8(1):2160.
96. Conde-Agudelo A, Romero R. Cervicovaginal fetal fibronectin for the prediction of spontaneous preterm birth in multiple pregnancies: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2010 Dec;23(12):1365-76.
97. Ganchimeg T, Morisaki N, Vogel JP, Cecatti JG, Barrett J, Jayaratne K, et al. Mode and timing of twin delivery and perinatal outcomes in low- and middle-income countries: a secondary analysis of the WHO Multicountry Survey on Maternal and Newborn Health. BJOG. 2014 Mar;121 Suppl 1:89-100.
98. Lee YM. Delivery of twins. Semin Perinatol. 2012 Jun;36(3):195-200.
99. Robinson BK, Miller RS, D'Alton ME, Grobman WA. Effectiveness of timing strategies for delivery of monochorionic diamniotic twins. Am J Obstet Gynecol. 2012 Jul;207(1):53.e1-7.
100. Dodd JM, Crowther CA, Haslam RR, Robinson JS; Twins Timing of Birth Trial Group. Elective birth at 37 weeks of gestation versus standard care for women with an uncomplicated twin pregnancy at term: the Twins Timing of Birth Randomised Trial. BJOG. 2012 Jul;119(8):964-73.
101. Hoffmann E, Oldenburg A, Rode L, Tabor A, Rasmussen S, Skibsted L. Twin births: cesarean section or vaginal delivery? Acta Obstet Gynecol Scand. 2012 Apr;91(4):463-9.
102. Aviram A, Lipworth H, Asztalos EV, Mei-Dan E, Melamed N, Cao X, et al. Delivery of monochorionic twins: lessons learned from the Twin Birth Study. Am J Obstet Gynecol. 2020 Dec;223(6):916.e1-9.
103. Roman AS, Fishman S, Fox N, Klauser C, Saltzman D, Rebarber A. Maternal and neonatal outcomes after delayed-interval delivery of multifetal pregnancies. Am J Perinatol. 2011 Feb;28(2):91-6.
104. Farkouh LJ, Sabin ED, Heyborne KD, Lindsay LG, Porreco RP. Delayed-interval delivery: extended series from a single maternal-fetal medicine practice. Am J Obstet Gynecol. 2000 Dec;183(6):1499-503.
105. Hamersley SL, Coleman SK, Bergauer NK, Bartholomew LM, Pinckert TL. Delayed-interval delivery in twin pregnancies. J Reprod Med. 2002 Feb;47(2):125-30.
106. Lavery JP, Austin RJ, Schaefer DS, Aladjem S. Asynchronous multiple birth. A report of five cases. J Reprod Med. 1994 Jan;39(1):55-60.
107. Livingston JC, Livingston LW, Ramsey R, Sibai BM. Second-trimester asynchronous multifetal delivery results in poor perinatal outcome. Obstet Gynecol. 2004 Jan;103(1):77-81.