Abstract
Introduction: Evidence for treating severe rib fractures without a flail component (non-flail) has not yet been adequately evaluated. This study analyzed contemporary evidence for the surgical versus non-surgical treatment of adults with severe chest rib fractures, with further analysis by the flail component.
Materials and Methods: A systematic literature review and meta-analysis included studies evaluating patients with surgical fixation of severe rib fractures. All studies included non-flail patients. Random effects models pooled data for outcomes reported in ≥ 2 studies. The primary outcome was the duration of mechanical ventilation (DMV). Secondary outcomes included post-procedural pain, respiratory complications, mortality, tracheostomy, sepsis, intensive care unit (ICU), and hospital length of stay (LOS).
Results: Thirty-one studies (n=99,640 patients) evaluating surgical fixation of severe rib fracture patients were included in the meta-analysis. Surgical fixation resulted in statistically significantly shorter DMV (-1.81 days, 95% confidence interval (CI): -3.14 to -0.49 days; p=0.007), lower 2-week pain intensity (SMD -3.29, 95% CI: -5.05 to -1.53; p=0.003), lower risk for atelectasis (RR=0.41, 95% CI: 0.25-0.67; p=0.0003), lower risk for any respiratory complication (RR=0.63, 95% CI: 0.43- 0.92, p=0.02), and lower mortality risk (RR=0.41, 95% CI: 0.23-0.73, p=0.003) compared to non-surgical treatment. Statistically significant differences were not observed for pain 3-day after intervention (SMD -1.28, 95% CI: -3.32 to 0.75; p=0.22); pneumonia (RR=0.66, 95% CI: 0.40- 1.08; p=0.10), acute respiratory distress syndrome (RR 1.19, 95% CI: 0.18-7.96; p=0.85), tracheotomy (RR 0.66, 95% CI: 0.30-1.44, p=0.29), sepsis (RR=0.75, 95% CI: 0.17-3.28, p=0.70), ICU LOS (MD -1.01, 95% CI: -2.42 to 0.939; p=0.16), and hospital LOS (MD-1.52, 95% CI: -3.97 to 0.92; p=0.22).
Conclusion: Surgical treatment of patients with severe rib fractures, including a majority of non-flail patients, resulted in statistically significantly shorter DMV, less 2-week pain, lower risk of atelectasis and overall respiratory complications, and reduced mortality compared to non-surgical treatment.
Keywords
Rib fractures, Rib fixation, Surgery, Duration of mechanical ventilation
Introduction
Rib fractures are a commonly encountered traumatic injury and are associated with significant morbidity and mortality [1,2]. They are a marker of severe injury and can lead to defects in the chest wall and severe pain which may hinder breathing [3]. Patients with rib fracture have an increased risk of developing chest infection, impaired pulmonary function, sepsis, atelectasis, respiratory failure, and other pulmonary pathologies, and they are at risk for prolonged hospitalizations [4]. The contribution of rib fractures to prolonged disability and chronic pain has been found to be greater than traditionally expected [5]. Studies have reported a prevalence of chronic pain of 22% and work disability of 53% among patients with rib fractures [6].
As the number of fractured ribs increases, it is believed that the patient’s risk for undesired outcomes is increased not only because of other serious injuries, but also because of the respiratory complications that are a direct consequence of the pain and impaired capacity to ventilate [7-9]. Patients with a ‘flail chest’ are those who have three or more contiguous ribs fractured in two or more places [10]. Patients with a flail chest, or other forms of severe multiple rib fractures, frequently require mechanical ventilation and are at risk for death [11,12]. Older adults with rib fractures are particularly vulnerable as they have twice the morbidity and mortality of younger adults [13-16].
Surgical stabilization of rib fractures (SSRF) has recently been described as an effective approach to treat flail chest or severe rib fracture injuries [11,17]. Evidence for the effectiveness of SSRF compared to non-surgical treatment has been mounting, particularly over the past decade. The preponderance of evidence has centered around patients with flail chest rib fractures. Multiple published systematic reviews and meta-analyses have demonstrated that SSRF of flail chest may lead to shorter hospital and intensive care unit (ICU) stays, fewer cases of pneumonia, and reduced mortality [18-27]. A recent cost-effectiveness analysis also found that surgical stabilization of rib fractures for patients with flail chest was cost-effective [27].
Evidence for the effectiveness of SSRF among patients with non-flail severe rib fractures has been emerging very recently; however, it has not yet been adequately gathered, appraised, and integrated. A meta-analysis from Beks and colleagues [26] evaluated both flail chest and non-flail multiple rib fractures up through June 2017 and found that the evidence for flail chest was strong; however, the authors concluded that the evidence for non-flail multiple rib fractures was insufficient [26]. A systematic review by Ingoe and colleagues [25] evaluated flail chest and multiple rib fractures through March 2017 and found that all outcomes showed a statistically significant improvement in favor of SSRF for flail chest; however, again, the authors concluded that the evidence for multiple, non-flail, rib fractures was limited and the benefits uncertain. Similarly, the cost-effectiveness analysis by Choi and colleagues [27] evaluated SSRF of rib fracture in patients up through 2014 and found that fixation may be cost-effective in some patients without flail chest; however, the authors concluded that characterizing these patients required further study. Most recently, a 2020 meta-analysis by Long et al. evaluating the clinical efficacy of surgical vs non-surgical care for multiple rib fractures, with or without flail chest, concluded that surgical treatment resulted in faster recovery, lower risk of complications and better prognosis than non-surgical care [28].
A better understanding of the current evidence for the clinical and economic value of SSRF for severe rib fractures specifically for non-flail rib fractures would help healthcare providers and payers prioritize resource allocation and develop more effective and targeted interventions. Hence, the objectives of this study were to assess contemporary evidence for the clinical safety, effectiveness and economic outcomes associated with SSRF of severe rib fractures in adults, in studies that include non-flail patients.
Material and Methods
The systematic literature review and meta-analysis compared SSRF to non-surgical treatment for adult patients with severe chest rib fractures. The systematic literature review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [29]. The systematic review protocol was registered in the PROSPERO database.
Search strategy
The literature search was conducted on June 22, 2020, by electronic searching of MEDLINE, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), and Cochrane Database of Systematic Reviews databases. The search terms and search strategy utilized were: (multiple AND rib fractur*) OR ("non flail" OR "not flail" OR "non-flail" OR "nonflail" OR "without flail"). A broad search strategy was used since several relevant articles would have been missed if we narrowed the search using the terms surgery or surgical intervention and displaced or dislocated rib fracture.
Identification of studies to be included in the analysis
The search was intended to identify primary clinical studies evaluating outcomes of SSRF for severe rib fractures compared to non-surgical care, in populations that included at least a proportion of patients with a non-flail component. Severe was defined as multiple and/or displaced fractures. Studies included primary surgical centers as well as database analyses.
The search strategies were designed to identify records based on the following PICOTS (patient-intervention-comparator-outcome-time-source) framework. Patients: Skeletally-mature patients up to and including 80 years of age, with severe rib fractures (multiple and/or displaced). At least some patients in the study had to be diagnosed/identified as non-flail. This comprised studies evaluating only non-flail patients and studies evaluating mixed cohorts of patients with and without flail chest. Some mixed cohort studies stratified patients by the presence of flail chest, while others did not. Patients diagnosed with a tumor, spinal cord injury, or brain injury of moderate and severe intensity were excluded from the review. Studies evaluating only flail chest patients were excluded. Intervention: SSRF was defined as the intervention of interest. All fixation devices and surgical approaches (open vs minimally invasive) were acceptable. Comparators: Non-surgical care was defined as the comparator. Outcomes: The primary outcome was the duration of mechanical ventilation (DMV). Secondary outcomes included post-procedural pain, respiratory complications, mortality, tracheostomy, sepsis, and intensive care unit (ICU) and hospital length of stay (LOS). Papers stating at least one of these outcomes were included in the analysis. An effort was made to capture and consider any and all reported major clinical and economic outcomes. Selected outcomes were based on previously conducted meta-analyses on SSRF [18-27,30]. Time: No limit in the postoperative evaluation window was predefined. Outcomes measured from day of surgery onwards were included in the study. Study: Randomized controlled trials (RCTs), non-randomized clinical trials or studies, cohort studies, case control studies, registry studies, economic studies (budget impact and cost-effective analyses), and case series were included. Excluded studies included: technical articles, animal/cadaver studies, case reports, editorials, commentaries, and letters. Only English language literature was considered for review. The search was not restricted by publication date. Abstracts, case reports and manuscripts were included. Care was taken to ensure no duplication of data: when abstracts were included, subsequent publications were analyzed to ensure that the same patient population was not described twice.
Study selection procedure and data extraction
Two reviewers independently applied the PICOTS framework above to screen de-duplicated titles and abstracts obtained from the search strategy. Potentially relevant citations were checked in a full-text screening. Disagreements were resolved through discussion and reasons for exclusion were recorded. Figure 1 illustrates the study selection process as a PRISMA flow diagram.
Pre-specified data that were extracted from the relevant studies included the journal citation, study objectives, study design and data source, intervention, study population (ie, baseline demographic and clinical characteristics), sample size, duration of follow-up, primary and secondary outcome measures, and author’s conclusions.
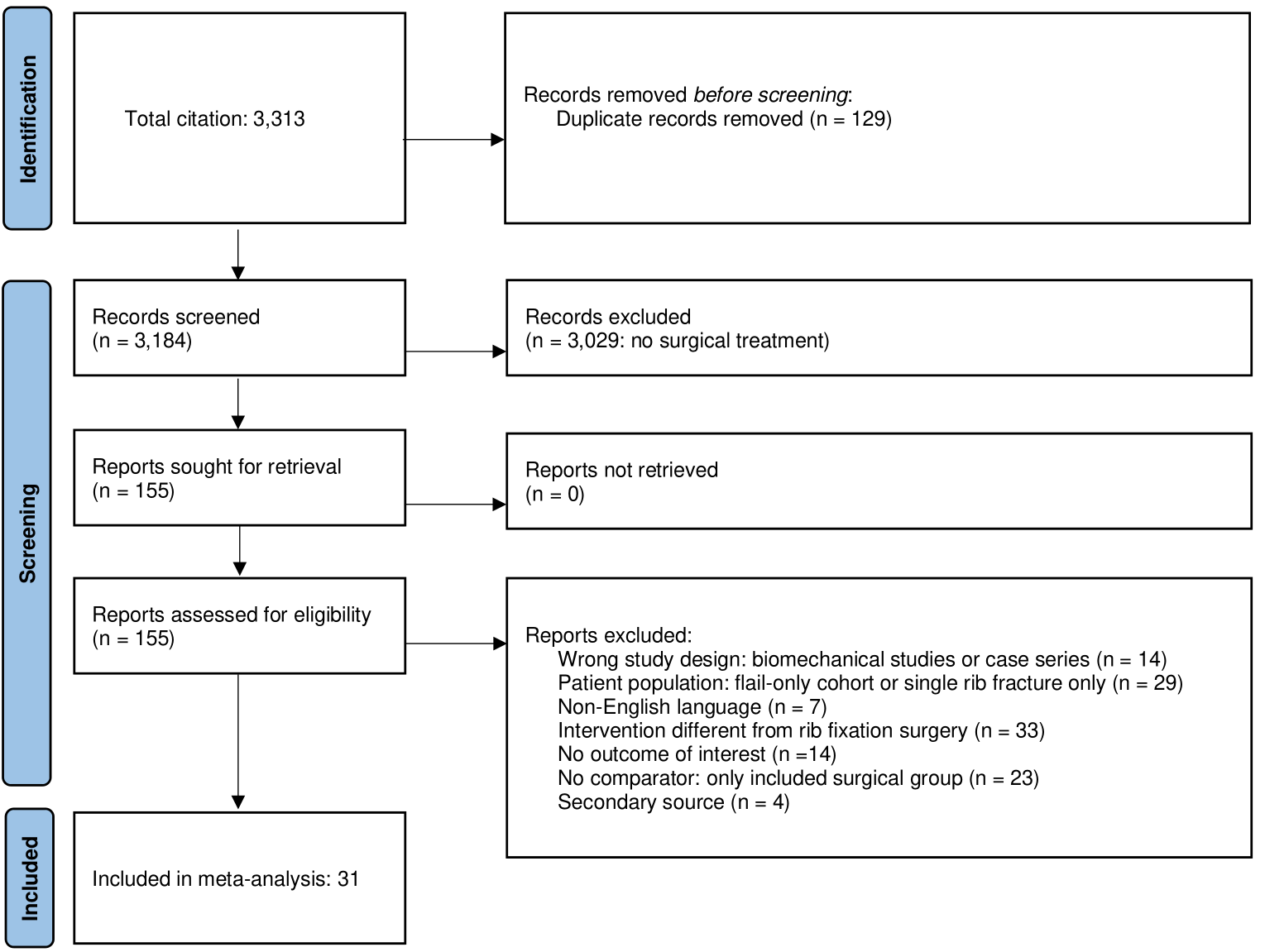
Figure 1. PRISMA flow diagram showing study selection.
Quality assessment of studies
Studies were appraised for their level of evidence based on the study design and the rigor of methodology used, as well as the ability to prevent and/or control for biases to analyze cause and effect. All included studies were critically appraised and ranked as either low, good, or high-quality evidence using the Evidence level and Quality Guide from John Hopkins Nursing Evidence-Based Practice [31,32].
Evidence synthesis and statistical analysis
The studies were initially summarized descriptively using frequency counts and proportions to describe the different types of studies and the numbers of patients. Qualitative synthesis, including narrative summarization, was conducted for outcomes where the meta-analysis of effect estimates was not appropriate or possible (outcomes not reported in at least two included studies), or because characteristics of studies (such as study designs, intervention types, or outcomes) were too diverse to yield a meaningful summary estimate of effect.
A meta-analysis was performed for outcomes that were reported in at least two distinct studies. For continuous outcome measures (ie, DMV, ICU LOS, and hospital LOS), the inverse variance random effects model (REM) with Dersimonian Lair was used to estimate the pooled mean difference (MD) between treatment groups, across all studies. The pooled standardized mean difference (SMD) was used for pain scores since the studies used different pain scales. The mean and standard deviation (SD) were extracted from individual studies or were derived from medians with interquartile ranges or means with p-values. For dichotomous outcomes, the Mantel–Haenszel REM was used to estimate the pooled risk ratios (RR). For the pooled summary statistics for each outcome in the surgical and non-surgical intervention groups, inverse variance REMs were used. All effect sizes were reported with 95% confidence intervals (CI). The χ2 test was used to identify statistical heterogeneity (α=0.05) and heterogeneity was quantified using the I2 statistic. Subgroup analyses evaluating the impact of: (a) presence or absence of flail chest patients; (b) study type; and (c) quality of evidence were also conducted. The statistical significance was set at p-value ≤0.05. RevMan was used for all analyses.
Results
Study identification and selection
The PRISMA flow diagram is shown in Figure 1. The literature search yielded 3,313 citations, of which 129 were duplicates leaving 3,184 studies that were screened for inclusion. Of these, 3,029 articles were excluded because they did not have a surgical treatment group or involved single fractures. Full texts of 155 of the studies were retrieved for further screening, of which 14 were excluded based on study design, 29 based on the patient population, 7 on non-English language, 33 on intervention, 14 due to lack of relevant outcome, 23 due to lack of or different comparator, and 4 that were prior meta-analyses (secondary sources).
Descriptive characterization of studies
A total of 31 studies were included in the analysis, describing outcomes of 99,640 patients, of which 4,675 underwent SSRF and 94,965 were treated non-surgically. The mean age of patients varied from 38 to 70 years. All of the included studies focused on surgical treatment and compared SSRF with non-surgical approaches. Whereas all studies described outcomes of non-flail patients, 8 studies included only non-flail patients, all other reported on a mix of flail and non-flail patients [12,33-39]. When available, the percentage of patients with non-flail component in the surgical and control groups are reported in Table 1. Overall, of the 4,675 SSRF patients, at least 82% (3,829/4,675) were identified as non-flail. In the control group, the proportion of identified non-flail patients was 97% (92,383/94,965). Studies included one randomized controlled trial (RCT) [40] and one hybrid RCT/prospective controlled cohort study [36]. In addition to these 2 studies, 3 cohort studies were prospectively designed [12,41,42]. All other studies were retrospective case-control or controlled cohort studies. The outcomes of 4 studies were presented in abstracts only [33,35,43,44], all other studies were reported in manuscripts. Eighteen of 31 studies were published between 2018 and 2020.
Three studies were used for narrative synthesis only [33,35,45], all other studies contributed outcomes data to the meta-analyses. The primary study outcome, the DMV, was reported in 16 studies, pain was described in 4 studies, respiratory complications in 17 studies, mortality in 19 studies, tracheotomy and sepsis in 8 and 7 studies, respectively, and hospital LOS and ICU LOS in 18 and 16 studies, respectively.
The studies were analyzed and ranked according to the John Hopkins Nursing Evidence-based Practice Level and Quality guidelines [31,32]. A summary of the quality assessment of each of the included clinical studies is available in Table 1. Visual inspection of funnel plots was also used to determine possible publication bias. Funnel plots were generated for outcomes with at least 10 included studies. The funnel plots for the secondary outcome measures are available as Figures S1-S5 of the Supplemental Files.
|
Study |
Year |
Study design |
No. of patients |
Mean age† |
Follow-up |
Surgical Cohort |
Non-Surgical Cohort |
Outcome‡ |
Level and Quality of Evidence |
||
|
N |
Of which: |
N |
Of which: |
||||||||
|
Nirula et al. [63] |
2006 |
Cohort Study |
60 |
51 |
NR |
30 |
50% (15/30) |
30 |
70% (21/30) |
AGH |
III - Low |
|
de Moya et al. [52] |
2011 |
Case Control Study |
48 |
46 |
NR |
16 |
43% (7/16) |
32 |
66% (21/32) |
ACDFGH |
III - Low |
|
Balci et al.* [44] |
2013 |
Cohort Study |
178 |
NR |
25.9 |
92 |
Unknown |
86 |
Unknown |
D |
III - Low |
|
Majercik et al. [64] |
2015 |
Case Control Study |
411 |
56 |
NR |
137 |
26% (36/137) |
274 |
68% (187/274) |
ACEGH |
III - Good |
|
Okoye et al.* [35] |
2015 |
Cohort Study |
13,853 |
48 |
NR |
1339 |
100% |
12514 |
100% |
III - Low |
|
|
Wu et al. [40] |
2015 |
Single-center RCT |
164 |
51 |
2 |
75 |
59% (44/75) |
89 |
61% (54/89) |
ABCDEGH |
I - Low |
|
Fagevik Olsen et al. [45] |
2016 |
Cohort Study |
61 |
58 |
12 |
31 |
Unknown |
30 |
Unknown |
III - Low |
|
|
Metin et al. [65] |
2016 |
Case Series |
44 |
57 |
36 |
17 |
Unknown? |
27 |
Unknown? |
H |
III - Low |
|
Qiu et al. [37] |
2016 |
Cohort Study |
124 |
38 |
6 |
65 |
100% |
59 |
100% |
CDH |
III - Good |
|
Pieracci et al. [42] |
2016 |
Cohort Study |
70 |
51 |
NR |
35 |
20% (7/35) |
35 |
69% (24/35) |
ABCDEGH |
II- Good |
|
Tarng et al. [66] |
2016 |
Case Series |
65 |
56 |
24 |
12 |
25% (3/12) |
53 |
Unknown |
ADEFGH |
III - Low |
|
Velasquez et al. [67] |
2016 |
Cohort Study |
40 |
49 |
NR |
20 |
Unknown |
20 |
Unknown |
ACDFGH |
III - Low |
|
Uchida et al. [48] |
2017 |
Cohort Study |
20 |
60 |
NR |
10 |
40% (4/10) |
10 |
Unknown |
ACDEFG |
III - Low |
|
Ali-Osman et al. [68] |
2018 |
Cohort Study |
199 |
70 |
NR |
64 |
Unknown |
135 |
Unknown |
ACDGH |
III - Good |
|
Kane et al. [69] |
2018 |
Cohort Study |
1,116 |
48 |
NR |
116 |
35% (41/116) |
1000 |
Unknown |
CDEGH |
III - Good |
|
Achary et al.* [43] |
2019 |
Cohort Study |
691 |
NR |
NR |
31 |
Unknown |
660 |
Unknown |
AFGH |
III - Low |
|
Azim et al.* [33] |
2019 |
Cohort Study |
474 |
NR |
NR |
237 |
100% |
237 |
100% |
III - Good |
|
|
Beks et al. [70] |
2019 |
Cohort Study |
332 |
56 |
NR |
65 |
43% (28/65) |
267 |
79% (212/267) |
ACGH |
III - Good |
|
Fokin et al. [71] |
2019 |
Cohort Study |
174 |
56 |
NR |
87 |
49% (44/87) |
87 |
90% (78/87) |
AD |
III - Good |
|
Haddadin et al. [34] |
2019 |
Cohort Study |
65,337 |
53 |
NR |
1240 |
100% |
64097 |
100% |
C |
III - Low |
|
Jiang et al. [72] |
2019 |
Cohort Study |
167 |
55 |
3 |
75 |
Unknown |
92 |
Unknown |
CDH |
III - Good |
|
Marasco et al. [73] |
2019 |
Cohort Study |
1,482 |
54 |
24 |
67 |
48% (32/67) |
1415 |
90% (1277/1415) |
ADG |
III - Good |
|
Mullens et al. [74] |
2019 |
Cohort Study |
12,910 |
57 |
< 1 |
57 |
82% (47/57) |
12853 |
100% |
AEGH |
III - Low |
|
Turner et al. [75] |
2019 |
Cohort Study |
64 |
NR |
NR |
32 |
Unknown |
32 |
Unknown |
D |
III - Low |
|
Xiong et al. [76] |
2019 |
Cohort Study |
123 |
47 |
NR |
68 |
Unknown |
55 |
Unknown |
CH |
III - Good |
|
Zhang et al. [39] |
2019 |
Cohort Study |
78 |
50 |
6 |
39 |
100% |
39 |
100% |
BDEF |
III - Good |
|
Dorman et al. [77] |
2020 |
Cohort Study |
96 |
65 |
NR |
54 |
28% (15/54) |
42 |
57% (24/42) |
C |
III - Low |
|
Dubrov et al. [41] |
2020 |
Cohort Study |
41 |
40 |
NR |
17 |
53% (9/17) |
24 |
63% (15/24) |
ACDFGH |
II - Good |
|
Li et al. [12] |
2020 |
Cohort Study |
98 |
55 |
12 |
66 |
100% |
32 |
100% |
D |
II - Good |
|
Pieracci et al. [36] |
2020 |
Cohort Study◊ |
110 |
55 |
2 |
51 |
100% |
59 |
100% |
BCD |
II - Good |
|
Xiao et al. [38] |
2020 |
Cohort Study |
1,010 |
50 |
1 |
430 |
100% |
580 |
100% |
ACDGH |
III - Good |
|
*Abstract only - no publication † As reported (mean or median) or calculated from reported ages of surgical and non-surgical cohorts ? non-flail percent provided for entire cohort: 68% (30/44) ◊ Mixed design: prospective cohort and RCT ‡ The contribution of each study to the specific meta-analyses is shown with letters (A-H) indicative of each outcome type. Studies that only contributed to the narrative assessments (Table S1 in Supplemental Files) have no associated letters. Abbreviations: A, duration of mechanical ventilation; B, pain scores; C, respiratory complications; D, mortality, E, Tracheotomy; F, Sepsis; G, length of hospital stay; H, length of ICU stay. |
|||||||||||
Meta-analyses
Duration of Mechanical Ventilation: 16 studies contributed to the DVM analysis, as shown in Figure 2. The aggregate mean DVM in the surgical group was 3.9 (SD 0.6) and in the non-surgical group, 5.5 (SD 0.6), for a mean difference of -1.8 (95% confidence intervals (CI): -3.1 to -0.5). This difference was significant (p<0.00001). Significant heterogeneity was identified across all studies (I2 = 95%).
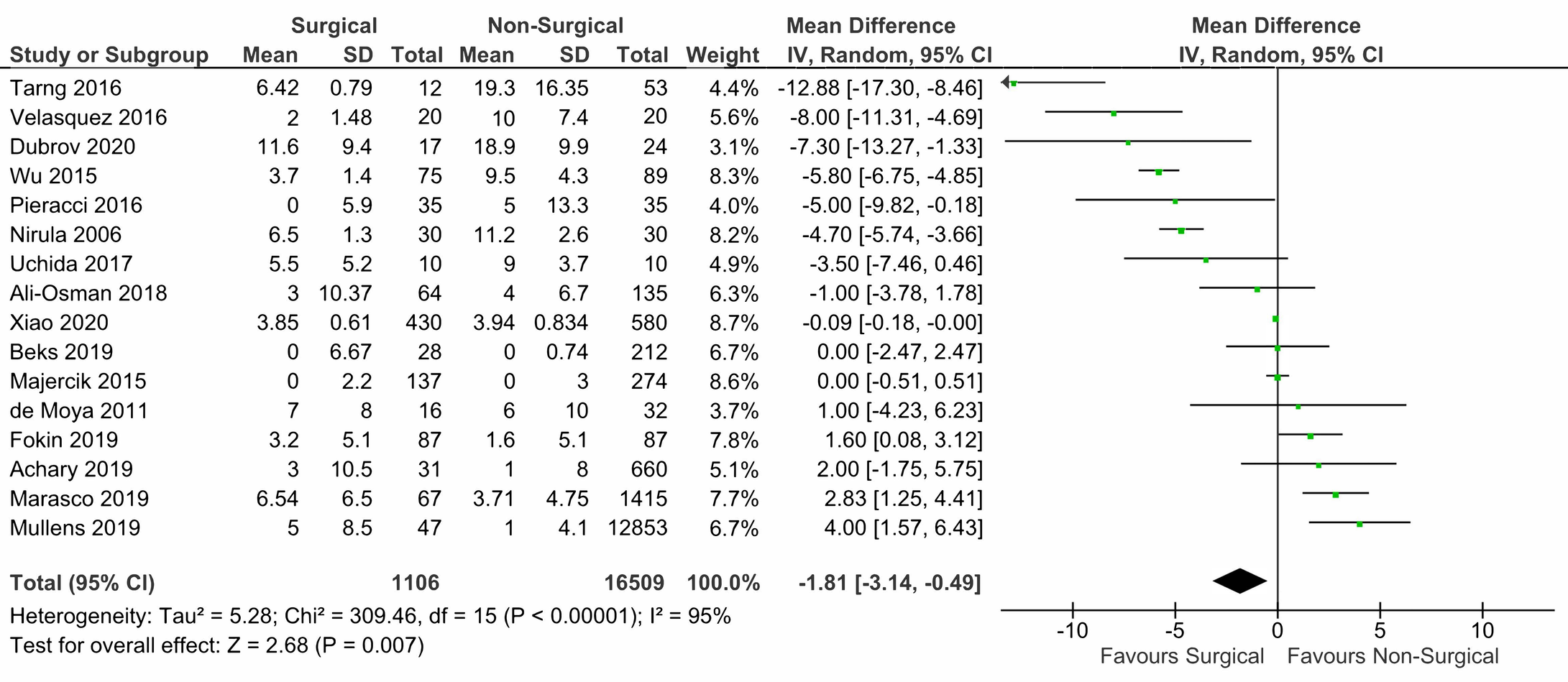
Figure 2. Forest plot of the meta-analysis of surgical vs non-surgical care in patients with severe rib fracture on duration of mechanical intervention (in days).
Post-Treatment Pain: Two different measures of pain were available: pain after 3 days (Figure 3a) vs. after 2 weeks post-intervention (Figure 3b). Only 2 papers described pain within 3 days of admission. In those papers, pain in the surgical cohort was lower (aggregate VAS score: 4.6 (SD: 0.7)) compared to that of patients in the non-surgical group (aggregate VAS score: 5.6 (SD: 0.2)). The mean difference of -1.28 (95%CI: -3.3 to + 0.75) was not significant [39,42]. For the 2 weeks post-intervention pain analysis, 3 studies contributed data. The difference in pain at that time was significant at -3.3 (95%CI: -5.0 to -1.5, p < 0.00001), suggesting lower pain for patients surgically treated [36,39,40]. For both analyses, significant heterogeneity was observed (I2>95%).
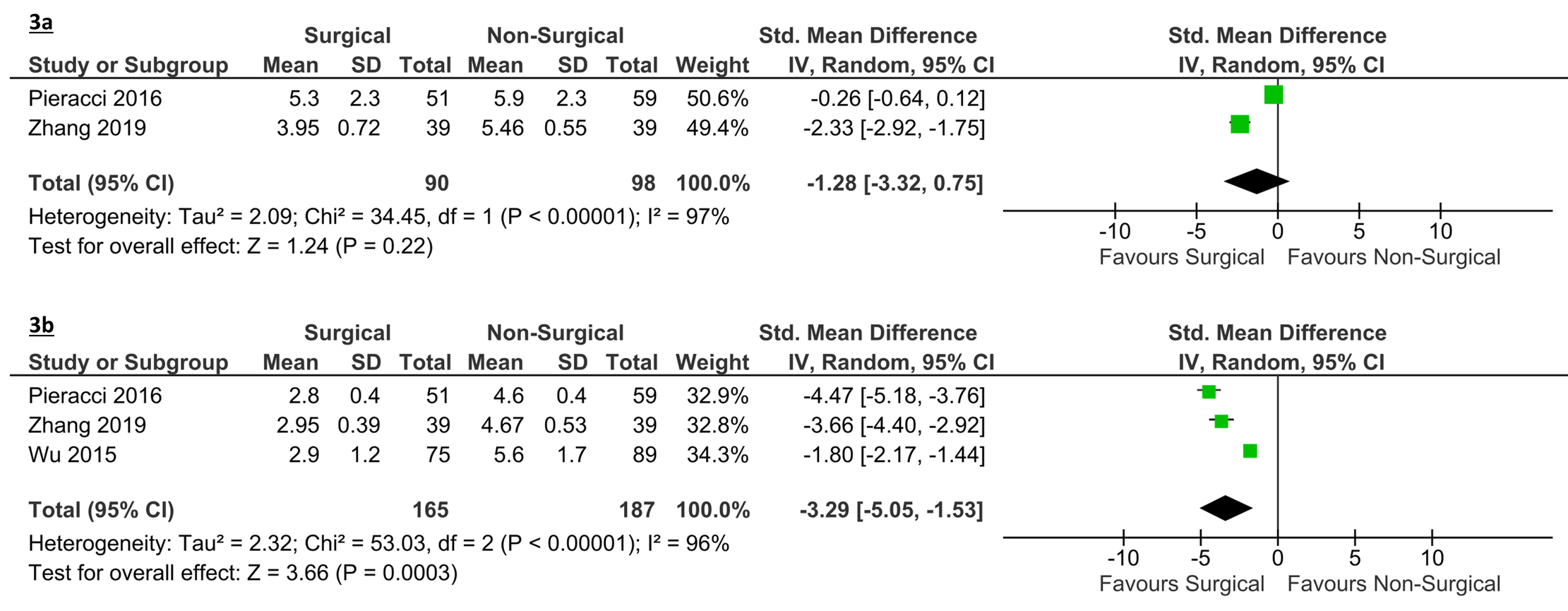
Figure 3. Forest plot of the meta-analysis of surgical vs non-surgical care in patients with severe rib fracture on pain at 3-days and 2 weeks post-intervention. 3a: Effect on pain scores at 3 days post-intervention. 3b: Effect on pain scores at 2 weeks post-intervention.
Respiratory Complications: 17 studies reported on respiratory complications, but not all studies reported on all complication types. Fourteen studies described risk of pneumonia (Figure 4a), 2 for risk of acute respiratory distress syndrome (ARDS) (Figure 4b), 8 studies described risk for atelectasis (Figure 4c), and 7 provided an aggregate risk for any respiratory complications (Figure 4d). The risk for pneumonia was not different between the surgical and non-surgical cohorts (risk ratio: 0.66 (95%CI: 0.40 to 1.08, p=0.1). The risk for ARDS was also not significantly different between groups. However, the risk for atelectasis was significantly lower in the surgical vs non-surgical cohort (risk ratio: 0.41 (95%CI: 0.25 to 0.67, p = 0.0003), and the aggregate risk for any respiratory complications was significantly lower in the surgical vs the non-surgical cohort (risk ratio: 0.63 (95%CI: 0.43 to 0.92), p = 0.02). High heterogeneity was observed for pneumonia, ARDS and the aggregate respiratory complication analyses (I2 > 63%) but low heterogeneity was observed for risk of atelectasis (I2 = 0%).
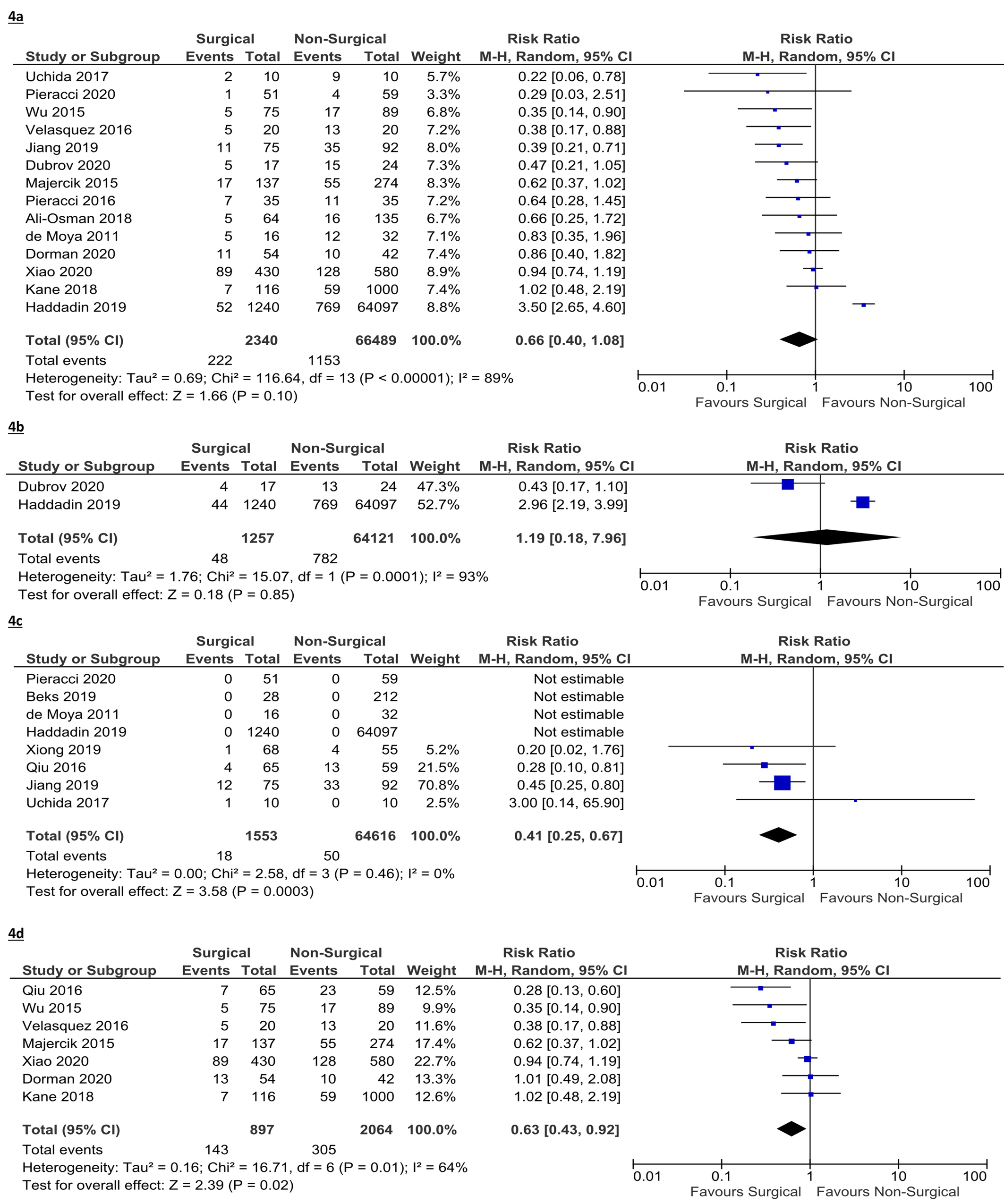
Figure 4. Forest plot of the meta-analysis of surgical vs non-surgical care in patients with severe rib fracture on risk of respiratory complications. 4a: Effect on risk of pneumonia. 4b: Effect on risk of acute respiratory distress syndrome (ARDS). 4c: Effect on risk of atelectasis. 4d: Effect on overall risk of respiratory complications.
Mortality: Nineteen studies evaluated the impact of SSRF on mortality, of which 10 studies reported actual numerical outcomes (Figure 5). The duration of follow-up ranged from the duration of the hospital stay to three months. The meta-analysis found that surgically treated patients had a statistically significantly lower risk of mortality (RR 0.41 (95% CI 0.23 to 0.73, p=0.003).
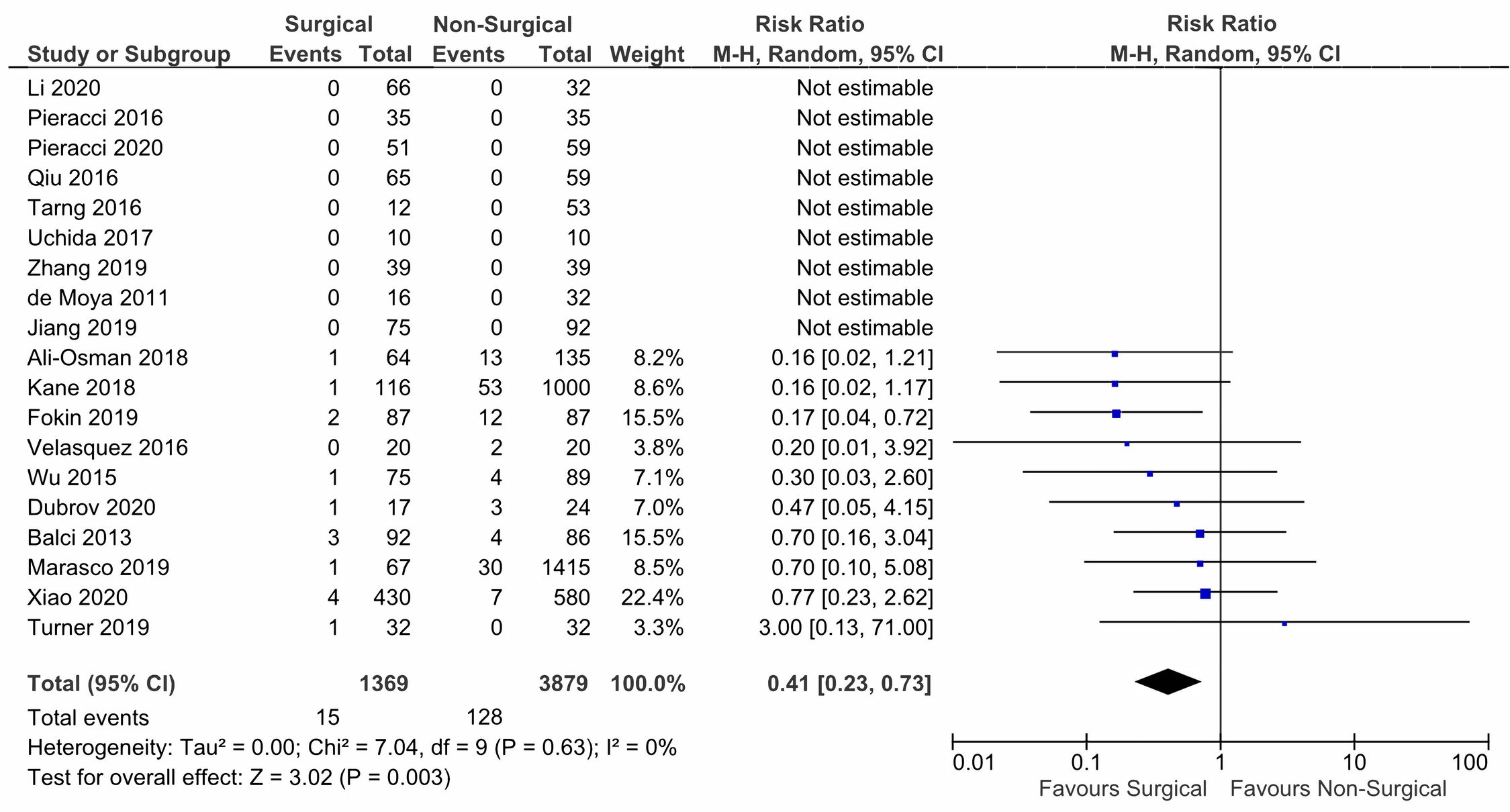
Figure 5. Forest plot of the meta-analysis of surgical vs non-surgical care in patients with severe rib fracture on risk of mortality.
Tracheotomy and Sepsis: As shown in Figures S6 and S7 in the Supplemental Files, no difference in rate of tracheotomy or sepsis were observed between SSRF and non-surgically treated patients (for tracheotomy: RR 0.66 (95%CI: 0.30-1.44, p = 0.29) – for sepsis: RR 0.75 (95%CI: 0.17 to 3.28, p = 0.70).
Length of Stay (LOS) – Intensive Care Unit (ICU) and Hospital: Differences in LOS, both in ICU and in hospital overall, were not significantly different between SSRF and non-surgically treated patients, showing a trend towards shorter LOS in SSRF patients, as shown in Figures S8(a) and S8(b). (Difference between SSRF and non-surgically treated LOS, in days: ICU: - 1.01 (95%CI: -2.42 to +0.39, p = 0.16 - Hospital: - 1.52 (95%CI: -3.97 to +0.92, p = 0.22)).
Discussion
Patients with non-flail, severe rib fractures, particularly older adults [13-16], frequently require mechanical ventilation and are at increased risk for death [11,12]. Many of these patients could benefit from SSRF [36,46-48], however, a lack of consensus regarding the appropriate indications for which to initiate surgical treatment typically leads to non-surgical management [49-52]. As surgical techniques and the technology of internal fixation devices have advanced, SSRF has become safer, easier to perform, and more efficient, and the debate about whether non-flail chest patients would benefit from SSRF continues to evolve as additional evidence emerges [30].
The current study showed that SSRF is beneficial to patients with severe rib fractures, including non-flail cases, as it results in a statistically significant shorter DMV, lower 2-week pain intensity, lower risk of atelectasis and overall respiratory complications, and reduced mortality, compared to non-surgical treatment. Although trending in favor of SSRF, differences between SSRF and non-surgical treatment were not statistically significant for pain three days after the intervention, pneumonia, sepsis, ICU LOS, and hospital LOS.
Differentiating pain levels at three days is challenging as it is expected to be very severe for all patients with severe rib fractures and, hence, it may be too early to detect differences between treatments utilizing validated instruments. For pneumonia, the reduced risk with SSRF approached statistical significance. Also, a subgroup analysis only including the studies with a quality rating of “good” (n=8) showed significantly lower risk of pneumonia (RR = 0.67, 95% CI= 0.51 to 0.87, p = 0.002, I2=28%) for SSRF vs non-surgically treated patients. The occurrence of sepsis was very infrequent, hence showing a statistically significant difference would require large sample sizes. It is also challenging to show statistically significant differences in resource utilization such as the mean hospital and ICU LOS given the variability and unpredictability among patients and the presence of outliers. Studies also included populations from different geographical locations (outside the United States) with potentially different protocols for duration of hospital care and discharge.
There were not adequate data to conduct meta-analyses for dose and duration of pain medicines, rates of emphysema, pneumothorax, hemothorax, pulmonary effusion, and readmission, cost of treatment, functional outcomes, and QoL. Evidence for the effectiveness of SSRF for particular outcomes has been mounting over the past decade, and it would be important to collect data for these outcomes as they have been identified as important considerations in the published medical literature [30].
The majority of studies evaluating SSRF included non-flail, severe patients, with some flail chest cases; however, the population with flail chest, in the SSRF arm, made up less than 5% of the overall sample. Our findings are therefore generalizable to most patients with severe, non-flail rib fractures.
Limitations of the current study include the heterogeneity of the patient populations evaluated, the surgical techniques and technologies employed, and the definitions of outcomes used in the analyses (eg, DMV may be defined as continuous positive airway pressure [CPAP] or tracheostomy and a mechanical ventilator). Heterogeneity is likely to arise when there are differences in patient populations, treatments, study design, outcomes, and data quality and is expected when pooling observational (real-world) data [53]. In the field of orthopedics, a growing opinion suggests that inclusion of observational studies in meta-analyses might lead to more robust conclusions without compromising the quality of the results [54,55]. The current study was conducted in line with recommendations available in the literature for the use of real-world evidence in meta-analyses [56]. Statistical heterogeneity was evaluated using Cochran’s Q test (χ2 test) and the I2 statistic. Since Q was significant and I2 was >50%, it was appropriate to use the random-effects model (REM) to calculate pooled summary estimates. The range of I2 values observed in the current study (0% to 97%) is consistent with the range of those observed in other published meta-analyses of SSRF (0% to 95%) [18-27].
Aside from SSRF, other factors that may influence the outcomes of patients with multiple severe rib fractures are the presence of lung contusion, the presence of pleural effusion including hemothorax and pneumothorax, a change of respiratory mechanics (eg, flail chest), compromised respiratory function due to pain, polytrauma, and the patient’s baseline health conditions [16,49,57-60]. The role of lung contusion in influencing the decision to proceed with surgical treatment is unclear [61]. Lung contusion is considered as a key risk factor for the need for ventilation and for near-term and long-term respiratory function and relevant complications [62]. The current study did not attempt to ascertain the influence of lung contusion on outcome given that the published data were not stratified by the presence of contusion and the studies were not randomized; hence, this variable or other unknown variables may have confounded results. However, it is also plausible that patients who received SSRF were more severe, in which case the bias would be against those treated surgically. A better understanding of the indications and circumstances under which surgical management of rib fractures is the optimal treatment option is needed.
Additional prospective and randomized controlled trials should be conducted among patients with multiple non-flail displaced rib fractures to validate the findings of this meta-analysis. Further studies should focus on the effect of injury severity, surgical technique, timing of surgery, follow-up duration, and the effectiveness of SSRF. Evaluation of economic benefits would also be beneficial to better understand the cost-effectiveness of SSRF in patients with non-flail rib fractures.
Conclusion
In conclusion, SSRF for patients with multiple displaced non-flail rib fractures resulted in shorter DMV, lower 2-week pain intensity, lower risk of atelectasis, lower risk of overall respiratory complications, and reduced mortality compared to non-surgical treatment; SSRF might be indicated in a broader range of cases than is currently performed. Additional studies would be beneficial in more clearly elucidating the specific patient populations that would benefit the most from SSRF.
Conflict of Interest
SW, TG, AW, RES, CEH and MV were employees of Johnson & Johnson (JnJ) at the time of the study. RS was working with ClinChoice as a contractor to JnJ at the time of the study. AMS is a consultant for DePuy Synthes, a J&J company, and a consultant for Globus Medical.
Funding Statement
This study was funded by DePuy Synthes, a Johnson & Johnson (JnJ) Company.
Acknowledgments
The authors would like to acknowledge Ms. Natalie Edwards, from Health Services Consulting Corporation, for editorial support.
References
2. Sharma OP, Oswanski MF, Jolly S, Lauer SK, Dressel R, Stombaugh HA. Perils of rib fractures. The American Surgeon. 2008 Apr;74(4):310-4.
3. Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. Journal of Trauma and Acute Care Surgery. 1994 Dec 1;37(6):975-9.
4. Pressley CM, Fry WR, Philp AS, Berry SD, Smith RS. Predicting outcome of patients with chest wall injury. The American Journal of Surgery. 2012 Dec 1;204(6):910-4.
5. Fabricant L, Ham B, Mullins R, Mayberry J. Prolonged pain and disability are common after rib fractures. The American Journal of Surgery. 2013 May 1;205(5):511-6.
6. Gordy S, Fabricant L, Ham B, Mullins R, Mayberry J. The contribution of rib fractures to chronic pain and disability. The American Journal of Surgery. 2014 May 1;207(5):659-63.
7. Flagel BT, Luchette FA, Reed RL, Esposito TJ, Davis KA, Santaniello JM, et al. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005 Oct 1;138(4):717-25.
8. Testerman GM. Adverse outcomes in younger rib fracture patients. Southern Medical Journal. 2006 Apr 1;99(4):335-40.
9. Whitson BA, McGonigal MD, Anderson CP, Dries DJ. Increasing numbers of rib fractures do not worsen outcome: an analysis of the national trauma data bank. The American Surgeon. 2013 Feb;79(2):140-50.
10. Helzel I, Long W, Fitzpatrick D, Madey S, Bottlang M. Evaluation of intramedullary rib splints for less-invasive stabilisation of rib fractures. Injury. 2009 Oct 1;40(10):1104-10.
11. Simon B, Ebert J, Bokhari F, Capella J, Emhoff T, Hayward III T, et al. Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. Journal of Trauma and Acute Care Surgery. 2012 Nov 1;73(5):S351-61.
12. Li Y, Gao E, Yang Y, Gao Z, He W, Zhao Y, et al. Comparison of minimally invasive surgery for non-flail chest rib fractures: a prospective cohort study. Journal of Thoracic Disease. 2020 Jul;12(7):3706.
13. Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. Journal of Trauma. 2000; 48(6):1040-6.
14. Elmistekawy EM, Abd Almohsen MH. Isolated rib fractures in geriatric patients. Annals of Thoracic Medicine. 2007 Oct;2(4):166.
15. Abdulrahman H, Afifi I, El-Menyar A, Al-Hassani A, Almadani A, Al-Thani H, et al. Clinical outcomes of multiple rib fractures: does age matter? European Journal of Trauma and Emergency Surgery. 2013 Dec;39(6):605-11.
16. Barry R, Thompson E. Outcomes after rib fractures in geriatric blunt trauma patients. The American Journal of Surgery. 2018 Jun 1;215(6):1020-3.
17. Bhatnagar A, Mayberry J, Nirula R. Rib fracture fixation for flail chest: what is the benefit?. Journal of the American College of Surgeons. 2012 Aug 1;215(2):201-5.
18. Slobogean GP, MacPherson CA, Sun T, Pelletier ME, Hameed SM. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. Journal of the American College of Surgeons. 2013 Feb 1;216(2):302-11.
19. Leinicke JA, Elmore L, Freeman BD, Colditz GA. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Annals of Surgery. 2013 Dec;258(6):914-921.
20. Cataneo AJ, Cataneo DC, de Oliveira FH, Arruda KA, El Dib R, de Oliveira Carvalho PE. Surgical versus nonsurgical interventions for flail chest. Cochrane Database of Systematic Reviews. 2015; 2015(7).
21. Coughlin TA, Ng JW, Rollins KE, Forward DP, Ollivere BJ. Management of rib fractures in traumatic flail chest: a meta-analysis of randomised controlled trials. The Bone & Joint Journal. 2016 Aug;98(8):1119-25.
22. Swart E, Laratta J, Slobogean G, Mehta S. Operative treatment of rib fractures in flail chest injuries: a meta-analysis and cost-effectiveness analysis. Journal of Orthopaedic Trauma. 2017 Feb 1;31(2):64-70.
23. Schuurmans J, Goslings JC, Schepers T. Operative management versus non-operative management of rib fractures in flail chest injuries: a systematic review. European Journal of Trauma and Emergency Surgery. 2017 Apr;43(2):163-8.
24. Liang YS, Yu KC, Wong CS, Kao Y, Tiong TY, Tam KW. Does surgery reduce the risk of complications among patients with multiple rib fractures? A meta-analysis. Clinical Orthopaedics and Related Research. 2019 Jan;477(1):193-205.
25. Ingoe HM, Coleman E, Eardley W, Rangan A, Hewitt C, McDaid C. Systematic review of systematic reviews for effectiveness of internal fixation for flail chest and rib fractures in adults. BMJ Open. 2019 Apr 1;9(4):e023444.
26. Beks RB, Peek J, de Jong MB, Wessem KJ, Öner CF, Hietbrink F, et al. Fixation of flail chest or multiple rib fractures: current evidence and how to proceed. A systematic review and meta-analysis. European Journal of Trauma and Emergency Surgery. 2019 Aug;45(4):631-44.
27. Choi J, Gomez GI, Kaghazchi A, Borghi JA, Spain DA, Forrester JD. Surgical stabilization of rib fracture to mitigate pulmonary complication and mortality: a systematic review and Bayesian meta-analysis. Journal of the American College of Surgeons. 2021 Feb 1;232(2):211-9e2.
28. Long R, Tian J, Wu S, Li Y, Yang X, Fei J. Clinical efficacy of surgical versus conservative treatment for multiple rib fractures: a meta-analysis of randomized controlled trials. International Journal of Surgery. 2020 Nov 1;83:79-88.
29. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Transparent Reporting of Systematic Reviews and Meta-Analyses. 2021 [cited 2021 April 18]; Available from: http://www.prisma-statement.org/.
30. de Campos JR, White TW. Chest wall stabilization in trauma patients: why, when, and how?. Journal of Thoracic Disease. 2018 Apr;10(Suppl 8):S951-S962.
31. Newhouse R, Dearholt S, Poe S, Pugh LC, White KM. Evidence-based practice: a practical approach to implementation. JONA: The Journal of Nursing Administration. 2005 Jan 1;35(1):35-40.
32. Newhouse RP, Dearholt SL, Poe SS, Pugh LC, White KM. Johns Hopkins nursing evidence-based practice model and guidelines. Indianapolis, IN: Sigma Theta Tau International Honor Society of Nursing; 2007.
33. Azim A, Khan MN, Jehan FS, Con J. In-Hospital Outcomes after Operative Fixation of Multiple Rib Fractures with Non-Flail Chest: A Propensity Matched Analysis. Journal of the American College of Surgeons. 2019 Oct 1;229(4):e232.
34. Haddadin Z, Hanna K, Castanon L, Zeeshan M, Ditillo M, Tang A, et al. Rib Plating the Non-Flail Chest May Not Be as Good as You Think. Journal of the American College of Surgeons. 2019 Oct 1;229(4):e241-2.
35. Okoye O, Horn C, Pieper M, Putty B, Naughton D, Freeman C. Impact of rib fixation on outcomes in mechanically ventilated blunt trauma patients. Critical Care Medicine. 2015 Dec 1;43(12):2.
36. Pieracci FM, Leasia K, Bauman Z, Eriksson EA, Lottenberg L, Majercik S, et al. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). Journal of Trauma and Acute Care Surgery. 2020 Feb 1;88(2):249-57.
37. Qiu M, Shi Z, Xiao J, Zhang X, Ling S, Ling H. Potential benefits of rib fracture fixation in patients with flail chest and multiple non-flail rib fractures. Indian Journal of Surgery. 2016 Dec;78(6):458-63.
38. Xiao X, Zhang S, Yang J, Wang J, Zhang Z, Chen H. Surgical fixation of rib fractures decreases intensive care length of stay in flail chest patients. Annals of Translational Medicine. 2020 Mar;8(5).
39. Zhang JP, Sun L, Li WQ, Wang YY, Li XZ, Liu Y. Surgical treatment ofpatients with severe non-flail chest rib fractures. World Journal of Clinical Cases. 2019 Nov 26;7(22):3718-3727.
40. Wu WM, Yang Y, Gao ZL, Zhao TC, He WW. Which is better to multiple rib fractures, surgical treatment or conservative treatment? International Journal of Clinical and Experimental Medicine. 2015;8(5):7930-6.
41. Dubrov S, Burianov O, Lianskorunskyi V, Miasnikov D, Tkalich V. Surgical stabilization of multiple rib fractures and multiple long bone fractures of lower extremities in polytrauma patients. Georgian Medical News. 2020 Apr 1(301):28-34.
42. Pieracci FM, Lin Y, Rodil M, Synder M, Herbert B, Tran DK, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. Journal of Trauma and Acute Care Surgery. 2016 Feb 1;80(2):187-94.
43. Achary CP, McCartney C, Zolfaghari P. 39th International Symposium on Intensive Care and Emergency Medicine. Critical Care. 2019;23(2):137-138.
44. Balci AE, Özyurtkan MO, Çakmak M. Treatment Alternatives for Traumatic Rib Fractures: Comparison of Operative Fixation and Conservative Approach - Abstract 123. Interactive CardioVascular and Thoracic Surgery. 2013;17(S2):S99.
45. Fagevik Olsén M, Slobo M, Klarin L, Caragounis EC, Pazooki D, Granhed H. Physical function and pain after surgical or conservative management of multiple rib fractures-a follow-up study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2016 Dec;24(1):1-9.
46. Pieracci FM, Agarwal S, Doben A, Shiroff A, Lottenberg L, Whitbeck SA, et al. Indications for surgical stabilization of rib fractures in patients without flail chest: surveyed opinions of members of the Chest Wall Injury Society. International Orthopaedics. 2018 Feb;42(2):401-8.
47. Pieracci FM, Lin Y, Rodil M, Synder M, Herbert B, Tran DK, Stoval RT, Johnson JL, Biffl WL, Barnett CC, Cothren-Burlew C. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. Journal of Trauma and Acute Care Surgery. 2016 Feb 1;80(2):187-94.
48. Uchida K, Nishimura T, Takesada H, Morioka T, Hagawa N, Yamamoto T, et al. Evaluation of efficacy and indications of surgical fixation for multiple rib fractures: a propensity-score matched analysis. European Journal of Trauma and Emergency Surgery. 2017 Aug;43(4):541-7.
49. Bemelman M, De Kruijf MW, Van Baal M, Leenen L. Rib fractures: to fix or not to fix? An evidence-based algorithm. The Korean Journal of Thoracic and Cardiovascular Surgery. 2017 Aug;50(4):229.
50. Kasotakis G, Hasenboehler EA, Streib EW, Patel N, Patel MB, Alarcon L, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. Journal of Trauma and Acute Care Surgery. 2017 Mar 1;82(3):618-26.
51. Ho AM, Karmakar MK, Critchley LA. Acute pain management of patients with multiple fractured ribs: a focus on regional techniques. Current Opinion in Critical Care. 2011 Aug 1;17(4):323-7.
52. De Moya M, Bramos T, Agarwal S, Fikry K, Janjua S, King DR, et al. Pain as an indication for rib fixation: a bi-institutional pilot study. Journal of Trauma and Acute Care Surgery. 2011 Dec 1;71(6):1750-4.
53. Higgins J, Thompson S, Deeks J, Altman D. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. Journal of Health Services Research & Policy. 2002 Jan 1;7(1):51-61.
54. Smeeing DP, van der Ven DJ, Hietbrink F, Timmers TK, van Heijl M, Kruyt MC, et al. Surgical versus nonsurgical treatment for midshaft clavicle fractures in patients aged 16 years and older: a systematic review, meta-analysis, and comparison of randomized controlled trials and observational studies. The American Journal of Sports Medicine. 2017 Jul;45(8):1937-45.
55. Abraham NS, Byrne CJ, Young JM, Solomon MJ. Meta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trials. Journal of Clinical Epidemiology. 2010 Mar 1;63(3):238-45.
56. Briere JB, Bowrin K, Taieb V, Millier A, Toumi M, Coleman C. Meta-analyses using real-world data to generate clinical and epidemiological evidence: a systematic literature review of existing recommendations. Current Medical Research and Opinion. 2018 Dec 2;34(12):2125-30.
57. He Z, Zhang D, Xiao H, Zhu Q, Xuan Y, Su K, et al. The ideal methods for the management of rib fractures. Journal of thoracic Disease. 2019 May;11(Suppl 8):S1078-S1089.
58. Söderlund T, Ikonen A, Pyhältö T, Handolin L. Factors associated with in-hospital outcomes in 594 consecutive patients suffering from severe blunt chest trauma. Scandinavian Journal of Surgery. 2015 Jun;104(2):115-20.
59. 59. Huber S, Biberthaler P, Delhey P, Trentzsch H, Winter H, Van Griensven M, et al. Predictors of poor outcomes after significant chest trauma in multiply injured patients: a retrospective analysis from the German Trauma Registry (Trauma Register DGU®). Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2014; 22(1):1-9.
60. Chien CY, Chen YH, Han ST, Blaney GN, Huang TS, Chen KF. The number of displaced rib fractures is more predictive for complications in chest trauma patients. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2017 Dec;25(1):1-10.
61. Dogrul BN, Kiliccalan I, Asci ES, Peker SC. Blunt trauma related chest wall and pulmonary injuries: An overview. Chinese Journal of Traumatology. 2020 Jun 1;23(03):125-38.
62. Ganie FA, Lone H, Lone GN, Wani ML, Singh S, Dar AM, et al. Lung contusion: a clinico-pathological entity with unpredictable clinical course. Bulletin of Emergency & Trauma. 2013 Jan;1(1):7.
63. Nirula R, Allen B, Layman R, Falimirski ME, Somberg LB. Rib fracture stabilization in patients sustaining blunt chest injury. The American Surgeon. 2006 Apr;72(4):307-9.
64. Majercik S, Wilson E, Gardner S, Granger S, VanBoerum DH, White TW. In-hospital outcomes and costs of surgical stabilization versus nonoperative management of severe rib fractures. Journal of Trauma and Acute Care Surgery. 2015 Oct 1;79(4):533-9.
65. Metin B, Intepe YS. Operative ease and efficiency of nitinol memory rib plaque on the multiple costa and sternum fractures: three-year clinical experience. International Journal of Clinical and Experimental Medicine. 2016 Jan 1;9(6):11510-7.
66. Tarng YW, Liu YY, Huang FD, Lin HL, Wu TC, Chou YP. The surgical stabilization of multiple rib fractures using titanium elastic nail in blunt chest trauma with acute respiratory failure. Surgical Endoscopy. 2016 Jan;30(1):388-95.
67. Velasquez M, Ordoñez CA, Parra MW, Dominguez A, Puyana JC. Operative versus nonoperative management of multiple rib fractures. The American Surgeon. 2016 May;82(5):103-5.
68. Ali-Osman F, Mangram A, Sucher J, Shirah G, Johnson V, Moeser P, et al. Geriatric (G60) trauma patients with severe rib fractures: Is muscle sparing minimally invasive thoracotomy rib fixation safe and does it improve post-operative pulmonary function? The American Journal of Surgery. 2018 Jul 1;216(1):46-51.
69. Kane ED, Jeremitsky E, Bittner KR, Kartiko S, Doben AR. Surgical stabilization of rib fractures: a single institution experience. Journal of the American College of Surgeons. 2018 Jun 1;226(6):961-6.
70. Beks RB, Reetz D, de Jong MB, Groenwold RH, Hietbrink F, Edwards MJ, et al. Rib fixation versus non-operative treatment for flail chest and multiple rib fractures after blunt thoracic trauma: a multicenter cohort study. European Journal of Trauma and Emergency Surgery. 2019 Aug;45(4):655-63.
71. Fokin AA, Wycech J, Weisz R, Puente I. Outcome analysis of surgical stabilization of rib fractures in trauma patients. Journal of Orthopaedic Trauma. 2019 Jan;33(1):3.
72. Jiang Y, Wang X, Teng L, Liu Y, Wang J, Zheng Z. Comparison of the effectiveness of surgical versus nonsurgical treatment for multiple rib fractures accompanied with pulmonary contusion. Annals of Thoracic and Cardiovascular Surgery. 2019; 25(4):185-191.
73. Marasco S, Lee G, Summerhayes R, Fitzgerald M, Bailey M. Quality of life after major trauma with multiple rib fractures. Injury. 2015 Jan 1;46(1):61-5.
74. Mullens CL, Seamon MJ, Shiroff A, Cannon JW, Kaplan LJ, Pascual JL, et al. A statewide assessment of rib fixation patterns reveals missed opportunities. Journal of Surgical Research. 2019 Dec 1;244:205-11.
75. Turner T, Shahid A, Bowdren K, Rutherford-Davies J. A Retrospective 2-Year Review Of The Outcomes Of Surgical Rib Fixation Following Chest Wall Injury By The Multi-Disciplinary Chest Wall Injury Group In A Major Trauma Centre And The Change In Outcomes As The Service Has Developed. Association of Surgeons of Great Britain and Ireland (ASGBI) Annual Congress 2019 - Telford, 2019. Abstract # 2195.
76. Xiong M, Hu W, Lou Q, Yin S, Wang X. Efficacy of nickel?titanium memory alloy in the treatment of multiple rib fracture combined with sternal fracture. Experimental and Therapeutic Medicine. 2019 Jul 1;18(1):537-42.
77. Dorman JR, Clarke PT, Simpson RB, Edwards JG. Testing the clinical validity of the Bemelman Rib Fracture Management Guideline. Interactive CardioVascular and Thoracic Surgery. 2020 Apr;30(4):597-9.
