Abstract
Objectives: The endometrial sampling procedure (ESP) with Pipelle is frequently used for diagnostic purposes in cases where endometrial pathologies are suspected in abnormal uterine bleeding. This study aimed to investigate video-based multimedia information (MMI)’s effect on anxiety and satisfaction levels of women undergoing endometrial sampling procedures.
Methods: The study was conducted prospectively in patients undergoing ESP for medical indications. Patients were randomly assigned to one of the two groups: the control group, which received verbal and written information before their ESP, and the video-based MMI group (case), which received video-based MMI before their ESP. Patients’ anxiety levels were measured with Beck Anxiety Inventory (BAI) 30 minutes before the procedure and ten minutes after ESP.
Results: Median BAI scores in the MMI and control groups were 5 and 9, respectively, and it was significantly lower in the MMI group. The mean VAS score of both groups were 3.1 and 3.3, respectively (p<0.05). Both groups' procedural patient satisfaction rates were 91.1% and 73.3%, respectively (p<0.05). Although there was no significant difference between the two groups in the VAS score of the ESP (p=0.42), the satisfaction rate of patients in the MMI group was significantly higher than patients in the control group.
Conclusion: Women who undergo invasive gynecological procedures such as endometrial sampling procedures have high anxiety levels and require special attention to manage stress and anxiety. Video-based MMI before the process may increase patients' knowledge about the procedure and decrease anxiety and dissatisfaction due to the procedure.
Keywords
Anxiety, Endometrial Sampling Procedure, Multimedia Information
Introduction
The endometrial sampling procedure (ESP) with Pipelle is frequently used for diagnostic purposes in cases where endometrial pathologies are suspected in abnormal uterine bleeding [1,2]. Endometrial sampling in the office setting has replaced the diagnostic dilatation and curettage (D&C) procedure often performed in the hospital. ESP, based on D&C sampling in the Operating Room, is relatively inexpensive and associated with less morbidity. Although it is a minimally invasive procedure that does not usually cause pain, it can sometimes cause anxiety in patients [3,4]. Anxiety is an abnormal and excessive sense of apprehension and fear, often marked by physiological symptoms [5]. Studies report that waiting for a surgical procedure is a very stressful period [6]. Physiological symptoms such as tachycardia, hypertension, sweating, or psychological symptoms such as anxiety, irritability, and aggression can be seen in 60% to 80% of patients who will undergo invasive surgery [7]. Insufficient knowledge about the planned surgical procedure has been identified as one of the most critical components associated with preoperative anxiety [8].
Although various pharmacological agents, such as anxiolytics and sedatives, can often be administered in the inpatient setting to relieve preoperative anxiety, they also have side effects. Pain can be minimized by explaining each step before the procedure and avoiding using a cervical dilator and tenaculum. Some clinicians may use nonsteroidal anti-inflammatory drugs (NSAID), intrauterine local anesthetic instillation, and paracervical block to reduce cramps [9]. The use of non-pharmacological agents is preferred to avoid side effects [10].
Obtaining informed consent is a critical stage in the surgical process that had remained chiefly changed since 1957 when the term was first used. A shift toward a more patient-centered healthcare system has also increased the need for effective doctor-patient communication and information transfer, which is critical to the consent process [11]. Alternatively, patient brochures can be used, but limited information can be given. Therefore, verbal information can lead to insufficient information [12]. The use of multimedia (MMI) tools to obtain patient consent can be helpful in the informed consent process. The objective of this paper was whether video-based MMI affected the anxiety and intra-operative pain scores of individuals undergoing endometrial sampling procedures.
We have identified two main objectives to investigate in patients undergoing ESP.
1: Comparison of preoperative anxiety scores and pain perception in the MMI and control groups.
2: To determine the effect of MMI and traditional information on patient satisfaction.
Materials and Methods
Design
Our study was conducted between October 2021 and April 2022. It was performed on patients between 25 and 70 who underwent ESP with medical indications. Informed consent forms were obtained from all participants, and study patient groups were formed.
Inclusion criteria
ESP indications were presented; abnormal uterine bleeding, presence of AGC-endometrial, monitoring of patients with endometrial pathology (e.g., endometrial hyperplasia), screening in patients at high risk of endometrial cancer (e.g., Lynch syndrome).
Exclusion criteria
Those who received treatment for anxiety and psychiatric reasons, those who were nulliparous, those with severe cervical infection, those with chronic pelvic pain and severe dysmenorrhea, those with endometrioma, those who had a previous ESP and bad experience, those with bleeding diathesis, or those with a history of cervical stenosis were not included in the study.
The Institutional Ethical Committee approved the study, which was carried out in accordance with the most recent version of the Helsinki Declaration. Institutional Ethical Committee approval was obtained before the subject enrolment (NEÜ/2022.04.147).
Procedure
Patients were randomly assigned to one of two groups: the control group, which received verbal and written information before their ESP procedure, and the video-based MMI group (case), which received video-based MMI before their ESP procedure. In the MMI video, one of the researcher's observations, ESP technique, benefits, side effects, personnel, instruments, and more are all covered in this movie (https://youtu.be/at-CfWUiClg). The video played once during the first hospital visit in a different room. Patients were divided into groups at random using randomization software (http://www.randomization.com) (Figure 1).
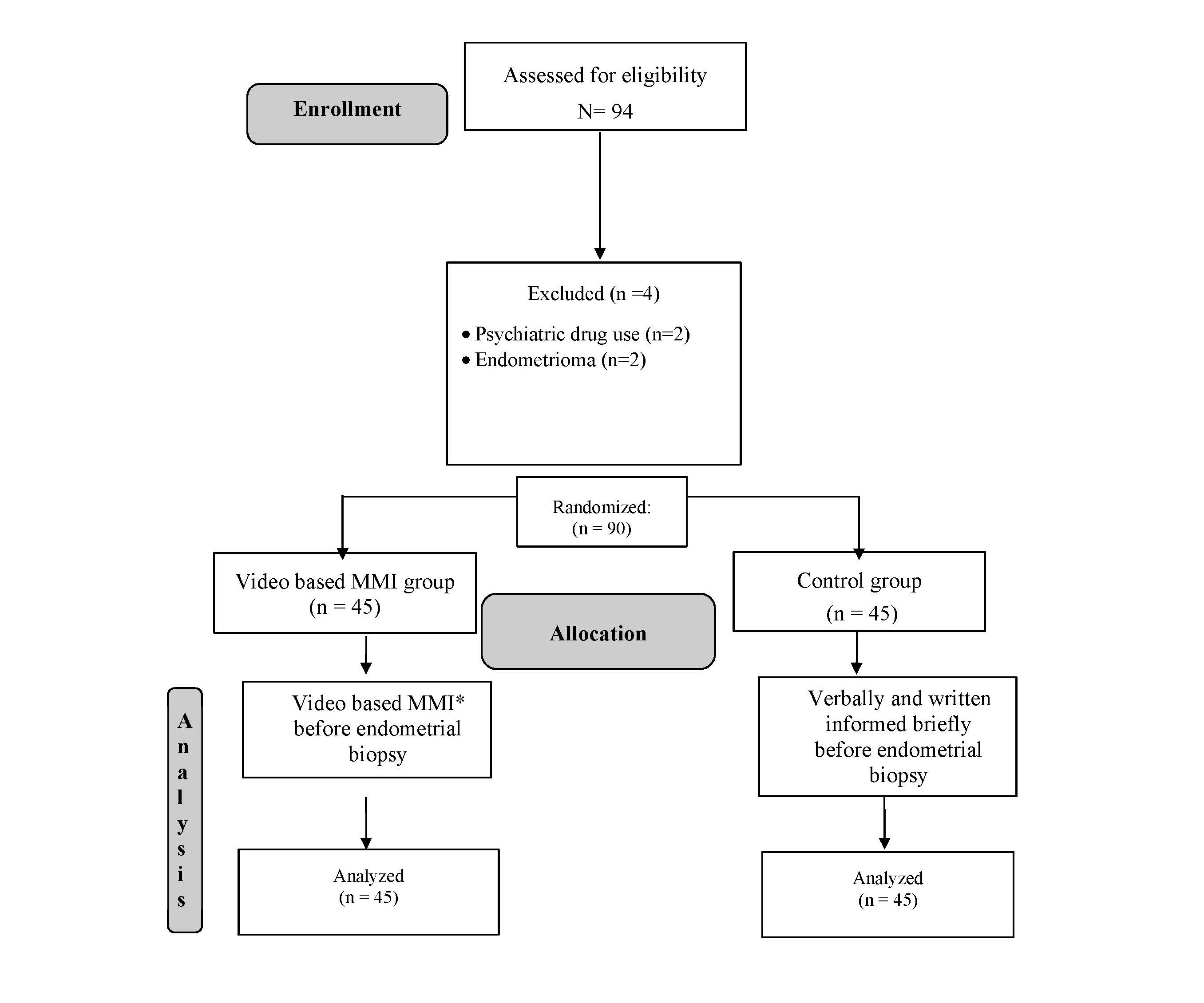
Figure 1. Flow diagram. *MMI: Multimedia Information.
Verbal information: The procedure is like a routine gynecological examination. The nurse will lay the patient on a flat table. The doctor inserts a speculum into the vagina, just like in the examination, and the cervix is cleared. The assistance of a thin plastic catheter (pipelle) from the cervix opening to the beginning of the uterine canal aspiration is performed with negative pressure. The procedure is generally painless.
Anti-inflammatory medications, analgesics, and local anesthetics were not used as premedication administered. In both groups, pain perception was evaluated with VAS score after the procedure.
Process
A bimanual examination was performed after preparing the patient in the dorsal lithotomy position to determine the uterus position. After the speculum was inserted, the cervix and vagina were cleaned with antiseptic. It was pipetted through the cervical canal, the sheath was fixed with one hand, and the plunger was pulled out to create suction. Aspiration was completed by moving the device tip along the endometrial surface using a corkscrew rotation with cephalic-caudal movement.
Measures
The Beck Anxiety Inventory (BAI) was used to assess the anxiety levels of patients 30 min before the procedure [13]. The patients responded to a questionnaire on an inventory scale that ranged from not at all (0) to severe (3). The overall score varied from 0 to 63 on a scale of one to one hundred. Anxiety was classified using cut-off ratings similar to those used in earlier studies on gynecological procedures. Anxiety ratings were divided into four categories: 0-7, minimal, 8-15, mild, 16-25, moderate, and 26-63, severe anxiety. The following information was gathered: age, infertility type, infertility period, gravidity, parity, and educational status.
Patients' procedural discomfort was rated on a ten-point visual analog scale (VAS) ten minutes after ESP.
Satisfaction: Satisfaction status was assessed on a four-point Likert scale (0; not satisfied, 1; poorly satisfied, 2; satisfied, 3; very satisfied). A Likert scale score ≥ 2 was assumed as satisfaction.
VAS Scale: All patients were observed for 60 minutes after the procedure and were asked to mark the pain they experienced on the VAS scale. In the 10 cm VAS scale, the absence of pain was accepted as 0 points, and the maximum pain was considered 10 points.
Statical analysis
The normality of continuous data was evaluated by The Kolmogorov - Smirnov or Shapiro-Wilk tests. For comparing continuous data, an Independent-sample t-test or Mann-Whitney U test, whichever suits, were used. Categorical data were analyzed with the chi-square test, and P values <0.05 were considered significant.
Primary and secondary outcome
In this study, we aimed to investigate the effect of video-based MMI on patients’ anxiety levels undergoing endometrial biopsy procedures. The secondary outcome was to investigate the impact of video-based MMI pain perception and satisfaction status due to the endometrial biopsy procedure.
Results
Ninety-four patients participated in this study. Two patients were excluded due to psychiatric drug use, and two were excluded due to endometrioma. Patients had randomly divided into two groups; the first group was the control group consisting of patients who were verbally and written informed briefly before the ESP (control group), and the second group consisted of patients who received video-based MMI before the ESP. There were 45 patients in the first group and 45 in the second group (Figure 1). The mean ages of the study population, control group, and MMI group were 42.1, 43.0, and 41.2, respectively. There was no significant difference in parity, body mass index (BMI), number of postmenopausal patients, or education status between the two groups (Table 1).
|
|
Study group (n=45) |
control group (n=45) |
p value |
|
Age (years) |
43.0 ± 7.5 |
41.2 ± 8.3 |
0.18 |
|
Parity (n) |
2.2 ± 1.2 |
2.7 ± 1. 3 |
0.21 |
|
BMI (kg/m2) |
27.4 ± 4.9 |
28.3 ± 4.3 |
0.28 |
|
Postmenopausal patients (n,%) |
10 (22.2%) |
13 (28.8%) |
0.31 |
|
Education |
|
||
|
> 8 years (n,%) |
16 (35.5 %) |
21 (46.6%) |
0.39 |
|
≤ 8 years (n,%) |
54 (64.5 %) |
49 (53.4%) |
|
|
Beck Score (median) |
5 |
9 |
<0.05 |
Median BAI scores in the MMI group and control group were 5 and 9, respectively, and it was significantly lower in MMI group. The degree of anxiety scores was classified into three groups; minimal, mild, and moderate/severe. It was compared in both groups. Minimal anxiety was significantly higher in the MMI group, but mild and moderate/severe anxiety were significantly higher in the control group (Table 2). The mean VAS score of both groups were 3.1 and 3.3, respectively. The procedural patient satisfaction rates of both groups were 91.1 % and 73.3%, respectively. Although there was no significant difference between the two groups in the VAS score of the ESP, the satisfaction rate of patients in the MMI group was significantly higher than patients in the control group (Table 3).
|
Beck Score |
Study group |
Control group |
p value |
|
Minimal (n, %) |
36 (80.0%) |
16 (35.5%) |
<0.05 |
|
Mild (n, %) |
8 (17.7%) |
25 (55.7%) |
<0.05 |
|
Moderate/ severe (n, %) |
1 (2.2%) |
4 (8.8%) |
<0.05 |
|
|
Study group |
Control group |
p value |
|
VAS score |
3.1 |
3.3 |
0.42 |
|
Satisfied with procedure (n, %) |
41 (91.1%) |
33 (73.3%) |
<0.05 |
Discussion
In our prospective case-control study, we investigated the effectiveness of an information video in reducing anxiety in patients who underwent endometrial sampling procedures. We found that in patients who will undergo ESP procedure, the group informed by MMI had lower pre-procedural anxiety scores and higher satisfaction than the verbally informed group.
Many surgical procedures increase patients' anxiety levels excessively. The Pipelle procedure is a better and equally tolerated procedure by patients compared to other office-based devices [14,15]. However, patients experience some discomfort during the procedure, which affects the effective use of the procedure. Half of the patients report pain, and the degree of this pain increases as the surgeon's experience decreases. Adambekov et al. [16], reported that patients who underwent ESP were significantly correlated with their pre-procedural anxiety scores and the pain scores they experienced at the procedure. In our study, since equally well-experienced surgeons performed the surgical procedure, the difference that may occur in this respect was prevented. When transferring minor gynecological procedures from the operating room to the office, healthcare providers must ensure that patients are comfortable, and procedures are carried out safely [17].
Providing appropriate information about the procedure for which they are scheduled can reduce concerns about surgery or intervention. Application of MMI before surgery with the advantages of visual perception can facilitate the education of patients and provide clear information instead of complex written information.
The effect of video information on anxiety is contradictory to previous studies. Freeman et al. reported that video information reduces anxiety in treatments such as colposcopy performed with the one-step see and treat method [18]. In a previous study, Yllmaz et al. stated that the application of MMI was associated with less anxiety and less postoperative pain [19]. While reducing patient stress in surgical interventions such as colonoscopy [20], Kazanclollu et al. reported that video information before dental surgery increased the anxiety scores of patients [21]. Eriç et al. also reported increased anxiety scores of informing with MMI in patients undergoing IUD (Intrauterine device) [22]. On the other hand, Wouters et al. reported that informing with video did not cause a significant decrease in anxiety in patients who underwent colposcopy [23]. They also reported that the level of satisfaction did not differ between the two groups. They attributed these results to the fact that patients access information more easily from the internet and ask questions until satisfied.
In our study, pre-procedural MMI provided lower anxiety scores and higher satisfaction than ESP patients' traditional written and verbal information.
Pain occurs during ESP Dilation of the cervix, uterine manipulation, and removal of the uterus. The content may cause pain during ESP. Anxiety is a significant risk factor in pain perception [24]. Yllmaz et al. stated that patients with video information felt less procedural pain than the control group. Furthermore, attributed this to a decrease in stress hormones [19]. On the other hand, a study showed that while anxiety levels decreased in ESP patients, procedural pain levels did not change [25]. Consistent with this study; in our study, no statistically significant difference was found between the two groups in procedural pain.
Strengths and limitations
Some limitations can be stated regarding this study. Correction of the axis by holding the cervix with the tenaculum may also cause pain. We used the tenaculum in some difficult to enter endometrium cases during ESP, which may have prevented an accurate assessment of the pain experience. The limitation of this study is that we did not exclude patients for whom we used the tenaculum. Anxiety-related symptoms can be determined hemodynamically. Our other limitation is that we did not record and evaluate these parameters in patients.
This study aimed to investigate the MMI method to reduce anxiety and procedural pain in patients to increase success during successful ESP. This study concluded that although MMI application reduced anxiety, it was ineffective in reducing procedural pain. Anxiety reduction may increase the patient's acceptance and compliance with the procedure, and elimination of patient anxiety increases the procedure's success and increases patient satisfaction.
Conflict of Interest
The author declares that there is no conflict of interest between the authors of the article.
Funding
The author declares that she did not receive any financial support in this study.
Author Contributions
Jule Eriç Horasanli: Writing – reviewing and editing, conceptualization, methodology, analysis and interpretation, and the final draft. Hasan Energin: Conceptualization, Methodology, video recording, analysis and interpretation, and the final draft.
References
2. DEMİR ET. 10-year endometrium cancer management in our clinic. Selçuk Tıp Dergisi. 2019 Oct 26;37(2):166-71.
3. Roomruangwong C, Tangwongchai S, Chokchainon A. Preoperative anxiety among patients who were about to receive uterine dilatation and curettage. J Med Assoc Thai. 2012 Oct;95(10):1344-51.
4. Kaiyrlykyzy A, Linkov F, Foster F, Bapayeva G, Ukybassova T, Aimagambetova G, et al. Pipelle endometrial biopsy for abnormal uterine bleeding: do patient's pain and anxiety really impact on sampling success rate? BMC Womens Health. 2021 Nov 12;21(1):393.
5. Crocq MA. A history of anxiety: from Hippocrates to DSM. Dialogues Clin Neurosci. 2015 Sep;17(3):319-25.
6. Leach M, Tanner S, Zernike W. How anxious are surgical patients?. ACORN Journal: Official Journal of the Australian Confederation of Operating Room Nurses. 2000 Mar 1;13(1).
7. Vetter D, Barth J, Uyulmaz S, Uyulmaz S, Vonlanthen R, Belli G, et al. Effects of Art on Surgical Patients: A Systematic Review and Meta-analysis. Ann Surg. 2015 Nov;262(5):704-13.
8. Palmer JA. Decreasing anxiety through patient education. Plast Surg Nurs. 2007 Oct-Dec;27(4):215-20.
9. Dogan E, Celiloglu M, Sarihan E, Demir A. Anesthetic effect of intrauterine lidocaine plus naproxen sodium in endometrial biopsy. Obstet Gynecol. 2004 Feb;103(2):347-51.
10. Wongkietkachorn A, Wongkietkachorn N, Rhunsiri P. Preoperative Needs-Based Education to Reduce Anxiety, Increase Satisfaction, and Decrease Time Spent in Day Surgery: A Randomized Controlled Trial. World J Surg. 2018 Mar;42(3):666-74.
11. Nehme J, El-Khani U, Chow A, Hakky S, Ahmed AR, Purkayastha S. The use of multimedia consent programs for surgical procedures: a systematic review. Surg Innov. 2013 Feb;20(1):13-23.
12. Ashraff S, Malawa G, Dolan T, Khanduja V. Prospective randomised controlled trial on the role of patient information leaflets in obtaining informed consent. ANZ J Surg. 2006 Mar;76(3):139-41.
13. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988 Dec;56(6):893-7.
14. Narice BF, Delaney B, Dickson JM. Endometrial sampling in low-risk patients with abnormal uterine bleeding: a systematic review and meta-synthesis. BMC Fam Pract. 2018 Jul 30;19(1):135.
15. Leclair CM, Zia JK, Doom CM, Morgan TK, Edelman AB. Pain experienced using two different methods of endometrial biopsy: a randomized controlled trial. Obstet Gynecol. 2011 Mar;117(3):636-41.
16. Adambekov S, Lopa S, Edwards RP, Bovbjerg DH, Linkov F, Donnellan N. Anxiety and Pain in Patients Undergoing Pipelle Endometrial Biopsy: A Prospective Study [11F]. Obstetrics & Gynecology. 2020 May 1;135:63S.
17. Urman RD, Punwani N, Bombaugh M, Shapiro FE. Safety considerations for office-based obstetric and gynecologic procedures. Rev Obstet Gynecol. 2013;6(1):e8-e14.
18. Freeman-Wang T, Walker P, Linehan J, Coffey C, Glasser B, Sherr L. Anxiety levels in women attending colposcopy clinics for treatment for cervical intraepithelial neoplasia: a randomised trial of written and video information. BJOG. 2001 May;108(5):482-4.
19. Yilmaz G, Akca A, Ay N, Koroglu N, Omaygenc DO, Ozdemir I, et al. The role of video-based multimedia information in reduction of anxiety before dilatation and curettage. North Clin Istanb. 2020 Nov 23;8(1):76-81.
20. Bytzer P, Lindeberg B. Impact of an information video before colonoscopy on patient satisfaction and anxiety - a randomized trial. Endoscopy. 2007 Aug;39(8):710-4
21. Kazancioglu HO, Tek M, Ezirganli S, Demirtas N. Does watching a video on third molar surgery increase patients' anxiety level? Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Mar;119(3):272-7.
22. Eriç J, Purut YE, Harmancı H. The Effect of Video Assisted Information on Anxiety and Pain Associated with Intrauterine Device Insertion. Gynecol Obstet Invest. 2020;85(1):82-87.
23. Wouters T, Soomers J, Smink M, Smit RA, Plaisier M, Houterman S, et al. The effect of an animation video on consultation time, anxiety and satisfaction in women with abnormal cervical cytology: Animation video reduces colposcopy time. Prev Med Rep. 2019 Jan 15;13:238-43.
24. De Iaco P, Marabini A, Stefanetti M, Del Vecchio C, Bovicelli L. Acceptability and pain of outpatient hysteroscopy. J Am Assoc Gynecol Laparosc. 2000 Feb;7(1):71-5.
25. Sert ZS. Effect of video information on anxiety level in women undergoing endometrial biopsy. Journal of Contemporary Medicine. 2020;10(4):505-9.
