Abstract
Endometriosis is a disease with a poorly known etiology, characterized by the presence of dysfunctional endometrial tissue, which evolves to chronic inflammatory reactions in women of reproductive age, causing a great impact on the quality of life of this population, often leading to infertility. This article aims to describe the impact of endometriosis on women's health, as well as the complications it can cause. The information was obtained from interviews and access to the patient's medical records, analyzing diagnosis, surgical procedures, and complications. However, it is hoped to deepen the existing knowledge about endometriosis, emphasizing the importance of correct and early diagnosis of this disease and the risks of complications related to diagnosis, surgery, and rehabilitation.
Keywords
Endometriosis, Laparoscopy, Colostomy, Rectovaginal fistula
Introduction
Endometriosis is considered a clinical condition that is difficult to diagnose, but recurrent in the female population. Known since the 17th century, it was first described by Von Rokitansky in 1860 and a new view emerged with Sampson in 1927, who suggested menstrual flow as a facilitator for endometrial tissue to implant in the peritoneal cavity [1]. It is a gynecological disease characterized by the growth of endometrial tissue outside the uterine cavity, almost exclusively diagnosed in patients of reproductive age in organs such as ovaries, posterior and anterior cul-de-sac, posterior leaflet of the broad ligament, uterosacral ligaments, uterus, fallopian tubes, sigmoid colon, appendix, and round ligaments [2]. More than 60 years have passed for the approach to the disease to change, thus establishing the concept of lesion infiltration, determining that retrograde menstruation causes the deep infiltrative form of endometriosis in the cavity [2,3].
As it progresses, the clinical presentation of endometriosis as signs and symptoms varies considerably, as it does not present pathognomonic clinical features, which makes it difficult to suspect and correctly diagnose [1]. Physical examination and clinical history are of little help in concluding the diagnosis, depending on the stage of the disease, thus requiring the use of diagnostic methods such as imaging tests, especially transvaginal and pelvic ultrasound and magnetic resonance imaging [1,2].
Goal
This is a case report of a patient with deep endometriosis who underwent surgical procedures with complications and is still in the process of rehabilitation due to sequelae.
Methods
The information contained in this clinical case description was obtained through a review of medical records, patient reports, images of diagnostic tests, and literature review.
Case Report
Patient M.S.O.C., 33 years old, sought outpatient health service as a beneficiary of health insurance, on an elective basis on August 17, 2021, at Hospital Ministro Costa Cavalcanti in the city of Foz de Iguaçu-PR, for consultation with a gynecologist. Previously, she had oophorectomy on the left due to ectopic pregnancy in 2015. During her consultation the following symptoms were reported, dysmenorrhea in the first three days, urinary urgency, and infertility. On specular examination blackish nodules in the bottom of the sac, on touch retroverted uterus, totally fixed, retrocervical nodule with apparent invasion of the vagina were observed. A complementary magnetic resonance imaging exam was recommended.
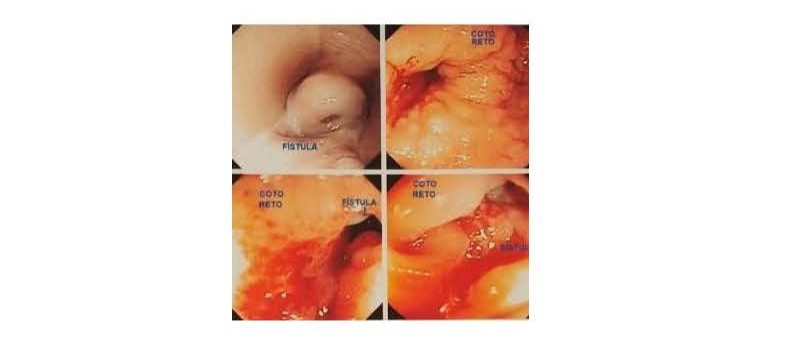
She returned on September 15, 2021, and was diagnosed with complex endometriosis of the posterior and left lateral compartment, endometriosis of the lower rectum, sigmoid, appendix, vagina, rectovaginal septum, adenomyosis, fibroid, left hematosalpinx, and left hypogastric plexus involvement. She underwent elective surgery on November 4, 2021 at the same hospital, where rectosigmoidectomy, right colectomy, hypogastric plexus nodule resection, bilateral parametrectomy, adenomyomectomy, colpectomy, appendectomy and enterectomy, rectovaginal septum tumor resection, uterosacral lesions, round ligaments, bladder peritoneum and ovarian fossa, left salpingectomy, and vaginal nodule were performed, a nodule in the ileocecal valve was identified during the intraoperative period and removed due to the risk of obstruction, and a nodule of endometriosis in the left lower hypogastric plexus. On the 5th postoperative day (PO) of endometriosis, the patient presented vomiting, abdominal distension, dehydration, and paralytic ileus. On 11/10/2021, a surgical reapproach of Laparostomy with colostomy was performed due to rectovaginal fistula, presenting vaginal bleeding three days later, requiring blood transfusion. On the 5th postoperative day of Laparostomy with colostomy, she was presented with bilateral pleural effusion and was referred to the Intensive Care Unit, where she received intensive support for 4 days and returned to the clinic. On the 11th postoperative day of Laparostomy with colostomy, the patient presented with profuse vaginal bleeding and underwent a new approach of laparotomy and colporrhaphy, and the bleeding persisted in the postoperative period, which was evaluated by the vascular surgeon, who opted for embolization of the right internal iliac branch, and after 4 days she was discharged. Hyperbaric treatment was indicated for fistula closure, and during the 5th session there was barotrauma in the right ear, which contraindicated the continuation of the treatment. The patient underwent medical follow-up for one year and two months by means of colonoscopy (Figure 1).
Figure 1.
A new medical evaluation was carried out and the re-approach was scheduled for January 30, 2023. A new surgical approach was performed, with partial colectomy by colostomy, reducing surgery, posterior access surgery, enterorrhaphy and removal of adhesions from previous surgery. She was discharged on the 3rd postoperative day, with collection of subsequent tests (D4 and D7). On the 14th postoperative day, she was presented with vaginal and rectal hemorrhage at home and was taken to the primary care unit in her hometown, where she had to be referred to the referral hospital in the neighboring city. She was evaluated in the emergency room and requested for a transfer to another hospital that had better facilities, during the care she presented severe hypotension, and the use of noradrenaline was necessary. The patient was referred from SAMU to another hospital, where she underwent computed tomography and red blood cell concentrate was administered. On further evaluation by a surgeon and gynecologist she was diagnosed with a new rectovaginal fistula. Patient continues to have a colostomy (transversostomy) and rectovaginal fistula. Rectal anastomotic stenosis was identified during control colonoscopy (Figure 2).
Figure 2.
Case Discussion
Rectovaginal fistula is an abnormal connection between the lower gastrointestinal tract and the vagina. They pose a great challenge to colorectal surgeons because of their complexity which depends on location, etiology and quality of the surrounding tissues. They are most often caused by obstetric trauma, gynecological surgeries, traumas, inflammatory diseases, among others. Small- diameter, distal fistulas in the rectovaginal septum secondary to traumatic injury or infection are considered simple. Those with a larger diameter, closer to the rectovaginal septum, and associated with underlying inflammatory bowel disease, radiation, neoplasia, or insufficient anterior repairs are considered more complex. There are several well-described surgical approaches that can be divided into trans anal, trans vaginal, trans perineal, and trans abdominal repairs. The type of procedure will depend on the quality of the surrounding tissues, the location, and the etiology of the fistula. In the last decade there has been a rapid use of bioprostheses in the form of plugs and gloves in the treatment of fistulas. A small number of cases have shown promising results, but there is still a paucity of long-term data. Therefore, we can verify the difficulty in the management of rectovaginal fistulas, treatment success, and latent risk of recurrence [4,5,6].
Conclusion
The present work aims to contribute to a deeper knowledge about endometriosis and its complications, since it is a topic of enormous relevance today, with the objective of motivating new health professionals and researchers to delve deeper into the pathology and its sequelae, encouraging them to produce new studies and demonstrate the impact of endometriosis on the quality of life of patients. For this, it is necessary to recognize the importance of early diagnosis and treatment of the disease, in order to avoid possible complications such as the one described in this case report, which directly influences the woman's infertility and fertilization rate, and the development of public policies aimed at the prevention and/or early detection of endometriosis is essential.
References
2. Ministry of Health; Clinical Protocol and Therapeutic Guidelines for Endometriosis; Ordinance nº879 of 12 July 2016; Retrieved from www.gov.br
3. Podgaec, Sérgio Manual of endometriosis / Sérgio Podgaec. -- Sao Paulo : Brazilian Federation of Gynecology and Obstetrics Associations (FEBRASGO), Manual Endometriosis 2015.pdf Retrieved from: (pucgoias.edu.br).
4. Soares GdeQ., Camargo de Jesus E, Lacerda da Silva IV, Faria Sarmento L. Fístula retovaginal: relato de caso clínico. Caminhos da Clínica. 2023.
5. Machado IB, Vieira MG, Rangel MP, Nishida FS. IMPACTO DA ENDOMETRIOSE NA SAÚDE DA MULHER: RELATO DE CASO. Electronic Annals XII EPCC, Unicesumar. 2021 (unicesumar.edu.br).
6. Costa ATD, Barbosa JC, Delfino GFdeL, Westphalen AP, Cipriani RFF, Fracaro GB, et al. FÍSTULA RETOVAGINAL: DA COLOSTOMIA AO AVANÇO DE RETALHO DE MARTIUS. Journal of Coloproctology. 2017; 37(Suppl 1):61.