Abstract
Objective: The aim of this study was to review the scientific literature on the efficacy of neuromuscular integration techniques for the rehabilitation of forward head posture (FHP) and rounded shoulder posture (RSP). Data Sources: Online databases CINAHL, PubMed, and SportDiscus were searched for the Boolean terms: “neuromusc* AND shoulder AND posture”, “neuromusc* AND neck AND posture”, “neuromusc* AND head AND posture”. Study Selection: Reviewed studies were limited to human studies with an exercise intervention. Studies that contained participants with severe chronic conditions or acute musculoskeletal injuries were excluded. Data Extraction: One reviewer extracted data on study and patient characteristics and selected articles were evaluated by 2 raters for methodological quality. Data Synthesis: A total of 281 subjects participated in the six chosen studies that met the inclusion criteria. Exercise intervention protocols were then reviewed and recommendations were made accordingly for the FHP and RSP respectively. Conclusions: Evidence showed efficacy of neuromuscular techniques for FHP, but not for RSP. This review also highlighted the lack of research in this field and the ambiguity in practice for what constitutes a neuromuscular integration method.
Keywords
Exercise intervention; Craniovertebral angle, Dysfunction
Abbreviations
FHP: Forward Head Posture; RSP: Rounded Shoulder Posture; ACL: Anterior Cruciate Ligament; UCL: Ulnar Collateral Ligament; PNF: Proprioceptive Neuromuscular Facilitation; CVA: Craniovertebral Angle; C7: Seventh Cervical Vertebrae; DNS: Dynamic Neuromuscular Stabilization; IC: Ischemic Compression; PEF: Peak Expiratory Flow; CMCPS: Chronic Myofascial Cervical Pain Syndrome
Introduction
Forward head posture (FHP) and rounded shoulder posture (RSP) are common postural misalignments caused by muscular imbalance that lead to a variety of pain patterns in the neck and shoulder [1,2]. FHP prevalence ranges from 61% to 85% and is associated with RSP [3-7]. RSP prevalence ranges from 66% to 78% [3,5,7]. Importantly, FHP and RSP have a number of negative effects on health and functioning, highlighting that these postural misalignments are of major societal concern [2].
FHP is characterized by weakening of the deep neck flexor muscles causing increased cervical lordosis [8] and a protruding head position due to the shortening of the semispinalis cervicis and capitis, along with the upper trapezius and levator scapulae. RSP is typically seen with scapula anterior tilt and internal rotation of the scapula giving a forward and rounded protrusion of the shoulders, caused by shortened pectoralis minor and weakness in the middle trapezius, lower trapezius, and serratus anterior [9-11].
Researchers have linked FHP and RSP to a range of negative functional signs and symptoms, such as increased pain and muscle strain [12-16], decreased strength and range of motion of the mandible, neck, and shoulders [17-21], a reduction in respiratory function [22-26], a decrease in stability [27,28], and alterations in muscle activation patterns and scapular kinematics and position [1,29-32]. FHP and RSP have also been linked to etiological pathologies such as temporomandibular joint dysfunction syndrome [33-35], thoracic outlet syndrome [33,36, 37], chronic neck pain [7,15,38], shoulder overuse injuries [ 1], scapular dyskinesis [31], and even cardiorespiratory impairments [39]. The breadth of these negative effects demonstrates that FHP and RSP are major upper body pathologies in need of addressing.
According to Griegel-Morris et al. [3], 66% of the 20-50- year old healthy subjects studied demonstrated FHP, and prevalence of RSP was reported to be 73% and 66% for right and left shoulders respectively. Thus, given the prevalence of FHP and RSP and their negative consequences for health and optimal functioning, an important question is how to remediate these conditions. Traditionally, clinicians have remediated these postural misalignments through isolated exercise rehabilitation protocols – that is, stretching the overactive muscles and strengthening the underactive muscles. This literature review examines the prevalence and effectiveness of a training methodology known as neuromuscular integration for the rehabilitation of FHP and RSP. In neuromuscular integration approaches, clinicians undertake rehabilitation in a more holistic manner, focusing on optimizing the patient’s ability to stabilize joints and postures, react to proprioceptive changes, and improve activation patterns.
This approach of incorporating neuromuscular training into rehabilitation has become increasingly popular, particularly for lower extremity injuries impacting the ankle, knee, and hip. The literature on anterior cruciate ligament (ACL) rehabilitation literature, in particular, is littered with articles related to ‘neuromuscular control,’ which is defined as muscle strength, power, and activation patterns [40] which can be extended to control of the core and trunk in the coronal plane [41].
Research on the lower extremity has revealed altered muscular recruitment patterns following injury [42,43]. Intriguingly, injuries to the upper body appear to influence lower body functioning, highlighting the integrated nature of human movement. For example, Garrison et al., [44] compared the lower extremity balance ability of baseball players with ulnar collateral ligament (UCL) tears to a healthy cohort and found poorer balance in those who had sustained an injury. Further supporting the integrated nature of human functioning, Ibrahim et al. [13] augmented their management of lumbosacral radiculopathy with FHP corrective exercises and observed reductions in pain and improvements in function for these patients.
Neuromuscular training can improve proprioception and stability [45] and induce isokinetic strength gains [46]. Research has also identified neuromuscular control as a potential prophylactic measure and indicator of injury risk [47,48]. The positive results of a neuromuscular integration philosophy applied to lower extremity injuries, combined with evidence of the integration between upper and lower body in functional movement, suggests there is value in exploring the effects of neuromuscular training on FHP and RSP.
Given the aforementioned background, the aims of the current study were: (i) to assess the availability of research for treating FHP and RSP using a neuromuscular integration exercise approach, and (ii) to critically review the scientific evidence for the effectiveness of these approaches on rectifying these maladaptive postures.
To identify the prevalence of neuromuscular integration approaches to FSP and RSP, we performed a systematic literature search to examine what evidence exists to support the use of neuromuscular training to treat these postural deviations. We considered exercise interventions neuromuscular in nature if they incorporated more than just isolated strengthening and stretching and instead used techniques such as proprioceptive neuromuscular facilitation (PNF) exercises, proprioception or stability training, or exercises that targeted core stability.
Methods
Data sources
A computerized search was conducted of all English available peer-reviewed scientific papers in CINAHL, PubMed, and SportDiscus. Studies were collected up to December 2020, with all articles being published between 2010-2020. To maximize the available literature on posture, searches included the terms head, neck, and shoulder. The following Boolean terms were used: “neuromusc* AND shoulder AND posture”, “neuromusc* AND neck AND posture”, “neuromusc* AND head AND posture”.
These terms were used to encompass all truncated forms of the potential term “neuromuscular”, and the specific body part search was varied on each search engine due to the ambiguous definition of these postures.
Study selection and methodological quality
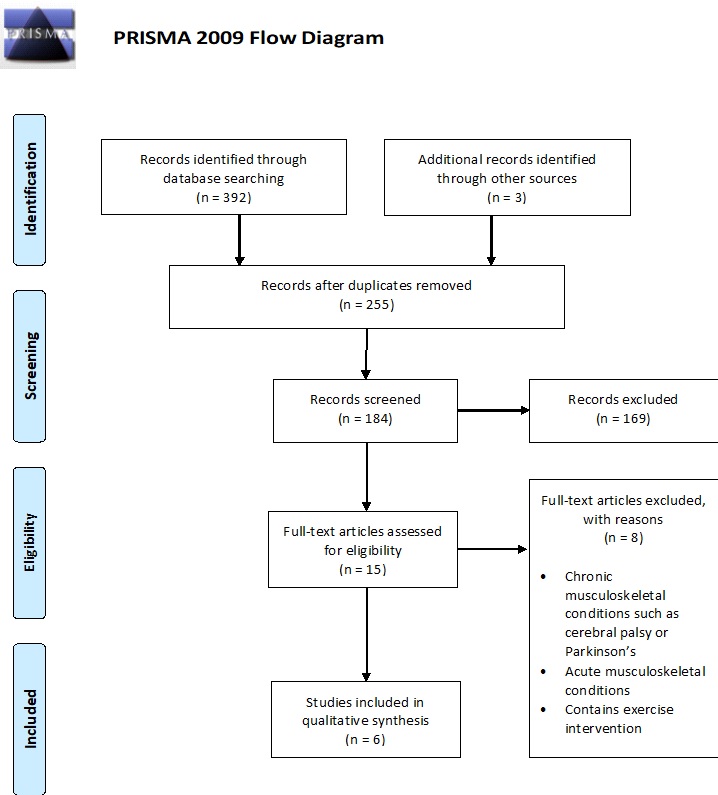
Figure 1 shows the PRISMA Flow Diagram of the processes used to select the final papers for review. A total of 392 papers were identified in the initial search. After removing duplicates and those not related to posture 184 remained. These remaining studies were checked to ensure they used human subjects, included no chronic conditions such as Cerebral Palsy or Parkinson’s Disease, no acute musculoskeletal injury, and contained an exercise intervention. The reference sections of the remaining articles were searched for any appropriate studies that fit the description, leading to the identification of three additional articles – leaving the final study count with six articles. The remaining article from Szczygiel et al. [49] was not a randomized control trial, thus it was excluded from the bias assessment tool.
Figure 1: PRISMA Flowchart paper selection.
Of the final six studies, five were randomized control trials. These were assessed using the Cochrane risk of bias assessment (Table 1), with all showing a low level of bias on all measures of bias assessment. The analyses of these five articles demonstrated heterogeneity in methodology.
| Risk of bias criteria | Birinci et al. (2020) | Lee et al. (2017) | Kim et al. (2019) | Moustafa et al. (2018) | Won-Sik et al. (2019) |
|---|---|---|---|---|---|
| Domain 1: Risk of bias arising from the randomization process |
Low | Low | Low | Low | Low |
| Domain 2: Risk of bias due to deviations from the intended interventions |
Low | Low | Low | Low | Low |
| Domain 3: Risk of bias due to missing outcome data |
Low | Low | Low | Low | Low |
| Domain 4: Risk of bias in measurement of the outcome |
Low | Low | Low | Low | Low |
| Domain 5: Risk of bias in selection of the reported result |
Low | Low | Low | Low | Low |
Data extraction
The results of the literature search are reported according to the specific technique of neuromuscular integration used, followed by the specific results these interventions had on FHP and RSP. The intervention strategies are described in detail and include the aim of the intervention, targeted musculature, and measurement techniques used. Table 2 provides background information for each study as well as a summary of the protocol and the results.
| Birinci (54) | Lee (55) | Kim (50) | Moustafa (51) | Szczgiel (52) | Won-Sik (53) | |
|---|---|---|---|---|---|---|
| Year of Publication | (2020) | (2017) | (2019) | (2018) | (2018) | (2019) |
| Country of Origin | Turkey | South Korea | South Korea | UAE | Poland | South Korea |
| Aim of Paper | Investigate which type of stretching exercise used after ischemic compression (IC) was more effective on latent trigger points in pectoralis minor | Determine the effect of forward head posture (FHP)-improving exercises on rounded shoulder posture (RSP) when employing the self-stretch exercise, McKenzie exercise, and the Kendall exercise as intervention methods. |
Investigate the effects of the McKenzie exercise program on forward head posture and respiratory function. | Investigate the functional and pain response outcomes of denneroll cervical extension traction compared to standard care in patient cases with chronic myofascial cervical pain syndrome (CMCPS) | Evaluate the effect of whole program exercise for activating deep stabilizer muscles on the posture and quality of respiratory movements. | Investigate the effects of dynamic neuromuscular stabilization (DNS) exercises on the vertebral structures and forward head postures of participants with forward head posture. |
| Target Population | 40 participants (6 male), aged 18-35 years old | 28 participants, aged 19 years and older | 30 adult men and women aged 20-29 | 120 patients (76 male) with chronic CMCPS, average age of 33.1 and 31.9 in the two groups |
18 participants, aged 20- 30 years old |
45 participants in their 20s |
| Protocol | Single-event stretching intervention Divided into 4 groups: IC with contract-relax PNF stretching IC with static stretching IC with myofascial release no intervention. Tests immediately after and 24hr post |
8-week training intervention, 25mins/day, 3x week, for 8 weeks Divided into 3 Groups: McKenzie Exercise Group Self-Stretch Exercise Group Kendall Exercise Group |
15 experimental 15 control Experimental exercises incorporated seven McKenzie exercises 20mins/day, 3x week, for 4 weeks. |
Intervention and control groups both received integrated neuromuscular inhibition techniques (INIT), intervention group received denneroll cervical traction device. 10 weeks treatment time, immediate assessment post intervention and 1 year follow up |
3 times per week for 4 weeks. Breathing exercises performed while prone, bridging, on all 4’s, and on unstable surface |
6-week training intervention. Group A performed neck stabilization exercise. Group B performed stretching and extensor strengthening exercise. |
| Results | Treatment methods using proprioceptive neuromuscular facilitation (PNF) techniques produced statistically significant improvements in RSP as measured by Pec Minor Index and Pec Minor Length. | Significant differences in craniovertebral angle (CVA) and scapular index in all groups, no significant differences between the groups. | CVA significantly improved in the experimental group. No significant difference was found in the control group. Respiratory measures were significantly improved in experimental group. Not so in the control. |
Patients suffering from cervical myofascial pain syndrome completed integrated neuromuscular inhibition technique and saw improvements in neck disability, pain intensity, and posture (CVA, Shoulder angle). | Deep stabilizer muscle exercises resulted in a significant change in the position of the body in the sagittal plane (posture) as well as an increase in the amplitude of breathing (optoelectric body explorer). | All exercise modalities improved FHP even in the DNS group who also saw improvements in core muscle activity and endurance indicating that DNS improves posture and ancillary measures. Measured using whole- body posture measurement system (GPS 400). |
Results
Content description
Of the six eligible papers, one used variations of an acute, single-bout stretching session following ischemic compression [54], one implemented a denneroll traction device combined with neuromuscular inhibition techniques [51], and the remaining four articles focused on stabilization and strengthening of involved musculature using neuromuscular integration techniques [50,52,53,55].
The heterogeneity in study designs, participant populations, forms of neuromuscular integration, durations of interventions, dependent measures, and quantification of FHP and RSP prevented an integrated presentation or meta-analysis of the findings. Therefore, the four FHP articles are summarized separately and the two RSP articles are summarized separately.
Forward head posture
In the selected papers, four articles reported on FHP [50-53] and used varying methods to do so, and all articles implemented their own unique form of neuromuscular integration for the rehabilitation of FHP. Kim et al. [50] used the McKenzie exercise program to investigate changes in FHP and respiratory function. Moustafa et al. [51] used integrated neuromuscular inhibition techniques in conjunction with a denneroll cervical traction device. Szczygiel et al. [52] performed breathing variations aimed at activating the deep core musculature, particularly the transverse abdominus, multifidus, and internal oblique muscles. Won-Sik et al. [53] examined three groups with different modalities of treatment including; Dynamic Neuromuscular Stabilization (DNS) techniques, McKenzie neck stabilization exercises, and cervical extensor stretching and strengthening.
Kim et al. [50] investigated the effects of the McKenzie exercise program on FHP and respiratory function in 30 adult men and women following a four-week training exercise protocol. Participants with FHP, as measured by craniovertebral angle (CVA), completed McKenzie exercises three times a week for four weeks, while control group participants received no intervention. CVA is a common FHP measurement technique that involves photographing a subject from the lateral view and marking cervical vertebrae seven (C7) and the tragus of the ear. A vertical line bisects the C7 mark and a diagonal line is drawn from the C7 marker to the tragus. The CVA is the angle between the vertical and diagonal line. A CVA of less than 49° was required and used for measurement of FHP. Forced vital capacity (FVC), FVC% predicted, forced expiratory volume at one second (FEV1), and FEV1 % predicted were measured for respiratory function.
The McKenzie exercises included: head retraction with overpressure while seated, neck extension while seated, head retraction with overpressure while lying, neck extension while lying, side bending of the neck while sitting, neck rotation while sitting, and neck flexion with chin-in in the siting position. These exercises were performed for seven seconds at static maximum muscle strength with a three second rest between each motion, and this was repeated 15-20 times. Exercise sessions lasted approximately 20 minutes and were completed three days per week for four weeks.
Kim et al. found significant differences in CVA and all respiratory measures between pre- and post-tests for the exercise group, and no differences for the control group. Between groups, only CVA and FVC% predicted were statistically different after the four-week intervention. The authors acknowledged that the small sample size and lack of long-term follow-up were limitations of the study. In addition, it could be argued that a longer intervention duration may have resulted in more pronounced results.
Moustafa et al. [51] randomly distributed 120 patients with chronic myofascial cervical pain syndrome (CMCPS) into a control or intervention group to complete a 10-week exercise intervention. They investigated the functional and pain response outcomes of the denneroll cervical traction device compared to traditional care – this traditional care implemented various neuromuscular integration techniques. Both groups received the integrated neuromuscular inhibition techniques (INIT), ischemic compression, strain counterstrain (SCS), and muscle energy techniques as their treatment intervention, but only the intervention group received the denneroll cervical traction device, aimed at improving cervical lordosis and alleviating FHP. Both groups also completed daily home exercises. This prospective, investigator-blinded, randomized clinical trial included patients with a cervical lordosis of less than 25° and a FHP measurement using craniovertebral angle (CVA) of less than 50o. Exercises and traction were performed three times per week for 10 weeks, with measurements taken at baseline, 10 weeks and 1-year post intervention.
Both groups exhibited statistically significant changes in NDI, pain intensity, algometric pressure, posture parameters, and cervical ROM after 10 weeks, however, the changes were significantly greater in the intervention group compared to the traditional care group for algometric pressure, posture parameters, and cervical ROM. At the 1-year follow up, the intervention group demonstrated significantly better outcomes than the traditional care group for all of the dependent measures, highlighting the superiority of the denneroll traction device in inducing positive changes in posture, pain, and function.
The authors attempted to blind participants to the group they were in by using a placebo traction method involving a small cervical towel in place of the denneroll device for control subjects. This sham traction force for the control group was used in a similar manner to the intervention group, but without applying a significant enough extension force to sufficiently bend the spine to mimic the intervention. Though the use of a placebo traction method was a clear strength of the study, sampling of the participants from a single clinic for convenience limited the ability to extrapolate these results out to a larger population.
Szczygiel et al. [52] recruited 18 volunteers aged 20-30 from a healthy, nonsmoking population without respiratory issues to complete a 4-week training intervention aimed at activating the deep stabilizers. The researchers evaluated how deep stabilizer muscle training would impact postural control and quality of breathing movements. Posture was measured using the optoelectric body explorer (OBE), which uses reflective markers placed on various anatomical landmarks to measure posture of the head, pelvis, and trunk in two dimensions. Reflective markers on the central part of the upper lip, occipital tuberosity, and the reference y-axis were used to measure FHP. Participants completed exercises three times per week for 4-weeks, which were designed to activate the transverse abdominus, multifidus, and internal obliques.
Exercises were performed supine, bridging, in a four-point kneeling position, and on unstable surfaces consisting of three sets of holding specific postures for 10 seconds, resting for five seconds, and repeating for 10 repetitions. Results showed improvements in sagittal plane trunk posture and abdominal excursion, but no other statistically significant improvements in sagittal plane head posture (FHP) were found after the 4-week training intervention.
Limitations of this study included the relatively small sample size, lack of control group, and lack of integration of other deep stabilizing musculature in the exercise intervention. Szczygiel et al. [52] noted that any future programs should include exercises aimed at improving head and upper body control, such as incorporating serratus anterior activation or FHP exercises. In addition, the biomechanical aspect of breathing was not measured through pulmonary function. Future studies would be wise to include this measure.
Won-Sik et al. [53] measured the effects of dynamic neuromuscular stabilization (DNS) exercises on changes in FHP in 45 participants in their 20s divided into three equal groups. The intervention lasted for six weeks. To measure FHP, researchers used the GPS 400 system and drew perpendicular induction lines through the center of the humerus and the outer ear line to calculate degree of FHP. Participants with 1 cm or greater distance between these two points were deemed eligible for the study. Thoracic kyphosis and lumbar lordosis were also measured using the GPS 400 system. In addition to the dynamic neuromuscular stabilization (DNS) group, the authors included two control groups. Control group A performed neck stabilization exercises and control group B performed stretching and extensor strengthening exercises.
The intervention group’s exercises involved using a pressure biofeedback device placed at the waist until the pressure measured 60 mmHg. Participants were then asked to increase this pressure by a further 10 mmHg by inhalation and exhalation. This pressure biofeedback device was then placed under the neck of the participant and used while performing neck stabilization exercises in static positions for 10 seconds and repeated 10 times at a pressure of 20 mmHg. The pressure was increased by two mmHg and repeated until the participant achieved a final measurement of 30 mmHg. Control group A completed the McKenzie neck strengthening exercises [same as those completed by Kim et al. [50] with the omission of two exercises], and control group B used isolated neck strengthening exercises with the same repetition and set structure as above.
Measurements performed at baseline, 3-weeks, and 6-weeks revealed that all three intervention groups improved FHP, thoracic kyphosis, and lumbar lordosis significantly after 6-weeks. No interaction effect was found between the three groups, indicating that although the DNS intervention was effective, it was no more effective than the exercises performed by either control group – one of which specifically implemented McKenzie neck stabilization exercises. Although no significant difference was found between the groups, Won-Sik et al. [53] demonstrated that implementing a DNS exercise program yielded postural results independent of specific isolation of the affected areas, highlighting the efficacy of a neuromuscular approach to rehabilitating postural dysfunctions.
Rounded shoulder posture
Two articles measured RSP [50,54]. Birinci et al. [54] measured RSP and respiratory function following an intervention utilizing different types of stretching maneuvers and manual therapy. Do Youn Lee et al. (2017) utilized FHP interventions (similar to those listed above) to investigate the impact those exercises had on RSP. Unfortunately, with RSP there is no consensus on a gold standard for measurement like the CVA measure for FHP. As such, these two studies used different measurement techniques.
Birinci et al. [54] measured RSP using Pec Minor Length, Pec Minor Index, and lying acromion to table distance – all of which have been validated previously. The aim of this study was to investigate the best neuromuscular stretching technique following a single session ischemic compression (IC) manual treatment. Consequently, there was no specific strengthening protocol put in place for this study, but the PNF stretching techniques utilizes muscle contractions at end-stage ROM and was deemed a neuromuscular technique.
The 40 study participants were randomly divided into four equal study groups: group 1 used IC with a modified contract-relax PNF stretch, group 2 used IC with a static stretch, group 3 used IC with myofascial release, and group 4 had no intervention. A physiotherapist performed all IC’s, a second, blinded therapist performed the stretching interventions, and a third physiotherapist performed all other assessments and data collection. Postural and respiratory outcome measurements were collected at baseline, immediately after the intervention, and 24 hours following the intervention.
This acute study showed differences in Pec Minor index in the PNF group and myofascial release group immediately and 24 hours after the intervention. The PNF group was the only group to report a statistically significantly improvement in pain pressure threshold immediately after the intervention. Pec Minor length improved in the PNF and myofascial release groups and FEV1, peak expiratory flow (PEF), FEV1/FVC, and maximum expiratory pressure all improved in the PNF group. The myofascial release group was the only other group to see improvements in respiratory function, with significant differences in maximum inspiratory pressure and maximum expiratory pressure. Non-significant changes were seen in the other groups and no group saw improvements in RSP.
Although Birinci et al. [54] did not utilize an extended exercise protocol, they still found improvements in pectoralis minor length and respiratory measures. This finding suggests that a longer PNF intervention may lead to improvements in RSP.
Do Youn Lee et al. (2017) split 28 participants into three distinct exercise groups: McKenzie exercise group (9), Kendall exercise group (9), and self-stretch exercise group (10) to determine whether neuromuscular exercises designed to improve FHP could also improve RSP. The exercise interventions lasted 25 minutes per day and were done three times per week for eight weeks. Measurements were taken pre- and post-intervention. Although the intervention focused on RSP and used the scapular index, FHP was also measured using the traditional CVA.
The McKenzie exercises were identical to those listed in the Kim et al. [50] paper. The Kendall exercises were more traditional, focusing on 15 repetitions of isolated stretching and strengthening techniques more commonly seen in FHP treatments. The self-stretch group performed 10 sets of 10 second stretch holds followed by five seconds of rest on the various neck musculature.
At the end of the training intervention, all groups showed statistically significant improvements from pre- to post-measures, but there was no statistically significant difference between groups for either FHP or RSP. Although no differences were found between groups, much like in Won Sik et al. [53], the findings demonstrated that a neuromuscular integration approach to FHP and RSP can still yield results. In particular, the exercises prescribed by Do Youn Lee et al. (2017) focused on correcting FHP to investigate the impact these exercises had on RSP – demonstrating the efficacy of a non-specific neuromuscular approach for treating postural dysfunction.
Discussion
This literature review aimed to identify and critically evaluate evidence for the efficacy of implementing a neuromuscular integration approach to the treatment of FHP and RSP in adult individuals. As discussed earlier, because neuromuscular integration techniques are commonly implemented in lower body rehabilitation programs, there is a need to investigate the efficacy of this training method for upper body rehabilitation. It is difficult to draw firm conclusions from the review, but a range of neuromuscular integration techniques appear to have the potential to correct FHP and RSP. Overall, however, the current evidence for the effectiveness of neuromuscular integration techniques in upper body rehabilitation is moderate given the limited number of studies, their heterogeneity, and the positive changes seen in control groups that were exposed to non-neuromuscular integration techniques, thus supporting the idea that more research is clearly needed.
Over a period of 10 years (2010-2020), six studies with strong methodological quality and low risk of bias were conducted. These studies included five RCTs and an observational study that evaluated the level of posture restoration using neuromuscular integration techniques in a combined total of 281 adult individuals. All five RCTs reported improvements in FHP and RSP, while the observational study did not reveal any changes in FHP and did not include a control group for comparison purposes. Despite the consistent improvements reported in the five RCTs, it is important to note that these improvements were generally equal to those of participants in control groups who received non-neuromuscular integration techniques. At the very least, these findings suggest that neuromuscular integration techniques are as effective as well-established exercise protocols, like McKenzie and Kendall, for improving upper body posture.
Two interrelated factors cloud the interpretation of the findings from this review and the conclusions that can be reached. The first is the lack of agreement in the field of rehabilitation on what constitutes a neuromuscular integration technique. The second factor, which logically stems from the first, is the high degree of methodological heterogeneity in the studies included in the review.
With regard to the first factor, the lack of agreement in exercise based physical rehabilitation as to what constitutes neuromuscular integration is clearly problematic. Myer et al. [56] referred to neuromuscular training as a training model to enhance health and skill-related components of physical fitness – this includes training modalities such as strength and conditioning modalities that focus on resistance and core-based strength, as well as stability, plyometric and agility training. Typically, in the lower extremity literature we see references to controlling the frontal and transverse planes of movement [57] and ability to control the body’s trunk during exercise [58]. Despite only one article measuring trunk posture [52], all articles integrated neuromuscular principles in their exercise selection which focused on exercises involving multiple planes of motion. Well established methodologies such as the McKenzie, Kendall, and DNS protocols were used in half of the studies, all of which led to improvements in the posture measurements [50,53,55], although sometimes these protocols were assigned to participants in the control groups rather than the primary intervention group. The remaining studies [51,52,54] implemented less structured methodologies, such as manual therapy techniques and home exercise prescription, and saw more mixed results.
With respect to the second factor, methodological heterogeneity was particularly high in terms of how the interventions were supervised and their durations. Three studies relied solely on home-based intervention protocols [50,53,55], one was a mix of home-based and therapist supervision [51], and the remaining two were treatment protocols led by a therapist [51,54]. Regarding duration, the studies ranged from an immediate intervention protocol to 10-week exercise interventions. For the purpose of comparison, exercise intervention protocols for treating FHP and RSP using non-neuromuscular approaches typically range from 6-12 weeks in duration [13,59-65]. Specifically, the neuromuscular intervention-based exercise programs included in this literature review had the following durations: immediate [54], 4-weeks [50,52], 6-weeks [53], 8-weeks [55], and 10-weeks [51] – meaning half of the articles in the current review used durations that fell below the typical duration of non-neuromuscular intervention protocols. It is also informative to compare the durations of the protocols used by the studies in the current review with the durations of neuromuscular integration protocols for the lower extremity. Traditional neuromuscular integration approaches for the lower extremity typically range from 6-10 weeks in duration or can be season-long interventions in certain sporting contexts [57,66-73]. Therefore, it could be argued that lack of improvement in posture in the two RSP articles [54,55] could be attributed to the fact that neither study reached the 6-week threshold considered ‘typical’ for a neuromuscular training intervention.
Finally, research on FHP has long used CVA as a valid and reliable measure of FHP [74,75], but RSP has no equivalent gold standard of measurement. The two articles that measured RSP used different measurement techniques. Birinci et al. [54] measured RSP by having the participant lie supine on a table, legs bent, with arms by their side, and measured the vertical distance between the posterior border of the acromion and the table. This technique’s obvious flaw is the lack of functionality - with the patient in a non-weightbearing, non-standing position to measure posture. In contrast to Birinci et al. [54], Do Youn Lee et al. [55] used the scapular index method which is becoming increasingly popular. It is performed with the patient standing in a relaxed posture. A tape measure is used to measure the distance between the sternal notch and coracoid process and the distance between the posterolateral angle of the scapula (acromion) to the thoracic spine is recorded. The former becomes the numerator and the latter the denominator, with the resultant number multiplied by 100 to capture a final measurement [76]. Lack of a gold standard of measurement for RSP compromises the repeatability and generalizability of findings generated by studies designed to test the efficacy of interventions for this type of postural deviation.
In conclusion, more research is needed before firm conclusions can be drawn about whether the implementation of neuromuscular integration techniques is an effective method for treating upper body postural disorders. The findings from this literature review indicate that this rehabilitation approach is effective for FHP, but the effectiveness of the approach for RSP is less clear. In the reviewed articles, the neuromuscular integration techniques were never shown to be inferior to traditional approaches to correcting these postural deviations, indicating that as this field continues to grow in evidence and practice, patients exposed to these techniques are unlikely to experience detrimental effects. The review also highlighted alternative avenues for application of these techniques, such as in the improvement of respiratory function.
Overall, it appears that neuromuscular integration techniques have the potential to correct FHP and RSP in otherwise healthy individuals, although further research is clearly required before definitive alterations in current exercise prescription methods for the treatment of FHP and RSP can be recommended.
References
2. Hajibashi, A., Amiri, A., Sarrafzadeh, J., Maroufi, N., Jalae, S.. Effect of kinesiotaping and stretching exercise on forward shoulder angle in females with rounded shoulder posture. Journal of Rehabilitation Sciences & Research 2014, 1(4): 78-83.
3. Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Physical Therapy. 1992 Jun 1;72(6):425-31.
4. Naz A, Bashir MS, Noor R. Prevalance of forward head posture among university students. Rawal Med J. 2018 Apr 1;43(2):260-2.
5. Vakili L, Halabchi F, Mansournia MA, Khami MR, Irandoost S, Alizadeh Z. Prevalence of common postural disorders among academic dental staff. Asian Journal of Sports Medicine. 2016 Jun;7(2).
6. Ramalingam V, Subramaniam A. Prevalence and associated risk factors of forward head posture among university students. Indian Journal of Public Health Research & Development. 2019 Jul;10(7):791-6.
7. Nejati P, Lotfian S, Moezy A, Moezy A, Nejati M. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Medical Journal of the Islamic Republic of Iran. 2014;28:26.
8. Bae WS, Lee KC, Lee DY. The Effects of Dynamic Neuromuscular stabilization Exercise on Forward Head Posture and spine Posture. Medico Legal Update. 2019 Aug 8;19(2):670-5.
9. Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. Journal of Orthopaedic & Sports Physical Therapy. 1999 Oct;29(10):574-86.
10. Kim EK, Kim JS. Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture. Journal of Physical Therapy Science. 2016;28(10):2929-32.
11. Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. British Journal of Sports Medicine. 2010 Apr 1;44(5):300-5.
12. Diab AA, Moustafa IM. The efficacy of forward head correction on nerve root function and pain in cervical spondylotic radiculopathy: a randomized trial. Clinical Rehabilitation. 2012 Apr;26(4):351-61.
13. Moustafa IM, Diab AA. The effect of adding forward head posture corrective exercises in the management of lumbosacral radiculopathy: a randomized controlled study. Journal of Manipulative and Physiological Therapeutics. 2015 Mar 1;38(3):167-78.
14. Haughie LJ, Fiebert IM, Roach KE. Relationship of forward head posture and cervical backward bending to neck pain. Journal of Manual & Manipulative Therapy. 1995 Jan 1;3(3):91-7.
15. Yip CH, Chiu TT, Poon AT. The relationship between head posture and severity and disability of patients with neck pain. Manual Therapy. 2008 Apr 1;13(2):148-54.
16. Mahmoud NF, Hassan KA, Abdelmajeed SF, Moustafa IM, Silva AG. The relationship between forward head posture and neck pain: a systematic review and metaanalysis. Current Reviews in Musculoskeletal Medicine. 2019 Dec;12(4):562-77.
17. Goh JY, O’Leary S, Chow A, Russell T, McPhail S. The relationship between forward head posture and cervical muscle performance in healthy individuals. Physiotherapy. 2015 May 1;101:e461.
18. Dehqan B, Delkhoush CT, Mirmohammadkhani M, Ehsani F. Does forward head posture change subacromial space in active or passive arm elevation?. Journal of Manual & Manipulative Therapy. 2021 Jul 4;29(4):227-34.
19. Lewis JS, Wright C, Green A. Subacromial impingement syndrome: the effect of changing posture on shoulder range of movement. Journal of Orthopaedic & Sports Physical Therapy. 2005 Feb;35(2):72-87.
20. Visscher CM, Huddleston Slater JJ, Lobbezoo F, Naeije M. Kinematics of the human mandible for different head postures. Journal of oral rehabilitation. 2000 Apr;27(4):299-305.
21. Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Manual Therapy. 2013 Feb 1;18(1):65-71.
22. Koseki T, Kakizaki F, Hayashi S, Nishida N, Itoh M. Effect of forward head posture on thoracic shape and respiratory function. Journal of Physical Therapy Science. 2019;31(1):63-8.
23. Savadatti R, Gaude GS. Effect of forward shoulder posture on forced vital capacity-A co-relational study. Indian Journal of Physical Therapy and Occupational Therapy. 2011 Apr 1;5(2):119-23.
24. Kapreli E, Vourazanis E, Billis E, Oldham JA, Strimpakos N. Respiratory dysfunction in chronic neck pain patients. A pilot study. Cephalalgia. 2009 Jul;29(7):701-10.
25. Han J, Park S, Kim Y, Choi Y, Lyu H. Effects of forward head posture on forced vital capacity and respiratory muscles activity. Journal of Physical Therapy Science. 2016;28(1):128-31.
26. Kang JI, Jeong DK, Choi H. Correlation between pulmonary functions and respiratory muscle activity in patients with forward head posture. Journal of Physical Therapy Science. 2018;30(1):132-5.
27. Beyranvand R, Mirnasouri R, Mollahoseini S, Mostofi S. The functional stability of the upper limbs in healthy and rounded shoulder gymnasts. Science of Gymnastics Journal. 2017 Sep 1;9(3):279-90.
28. Kang JH, Park RY, Lee SJ, Kim JY, Yoon SR, Jung KI. The effect of the forward head posture on postural balance in long time computer based worker. Annals of Rehabilitation Medicine. 2012 Feb;36(1):98-104.
29. Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Physical Therapy. 2000 Mar 1;80(3):276-91.
30. Kang DY. Deep cervical flexor training with a pressure biofeedback unit is an effective method for maintaining neck mobility and muscular endurance in college students with forward head posture. Journal of Physical Therapy Science. 2015;27(10):3207-10.
31. Weon JH, Oh JS, Cynn HS, Kim YW, Kwon OY, Yi CH. Influence of forward head posture on scapular upward rotators during isometric shoulder flexion. Journal of Bodywork and Movement Therapies. 2010 Oct 1;14(4):367-74.
32. McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. Journal of Orthopaedic & Sports Physical Therapy. 1998 Feb;27(2):125-33.
33. Darnell MW. A proposed chronology of events for forward head posture. Journal of Craniomandibular Practice. 1983 Sep 1;1(4):49-54.
34. Passero PL, Wyman BS, Bell JW, Hirschey SA, Schlosser WS. Temporomandibular joint dysfunction syndrome: a clinical report. Physical Therapy. 1985 Aug 1;65(8):1203-7.
35. Lee WY, Okeson JP, Lindroth J. The relationship between forward head posture and temporomandibular disorders. Journal of Orofacial Pain. 1995 Apr 1;9(2):161-7.
36. Smith KF. The thoracic outlet syndrome: a protocol of treatment. Journal of Orthopaedic & Sports Physical Therapy. 1979 Oct 1;1(2):89-99.
37. Hooper TL, Denton J, McGalliard MK, Brismée JM, Sizer PS. Thoracic outlet syndrome: a controversial clinical condition. Part 1: anatomy, and clinical examination/ diagnosis. Journal of Manual & Manipulative Therapy. 2010 Jun 1;18(2):74-83.
38. Silva AG, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI. Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Archives of Physical Medicine and Rehabilitation. 2009 Apr 1;90(4):669-74.
39. Lee MH, Chu M. Correlations between Craniovertebral Angle (CVA) and cardiorespiratory function in young adults. Journal of the Korean Society of Physical Medicine. 2014;9(1):107-13.
40. Myer GD, Brent JL, Ford KR, Hewett TE. Realtime assessment and neuromuscular training feedback techniques to prevent ACL injury in female athletes. Strength and Conditioning Journal. 2011 Jun 1;33(3):21-35.
41. Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact ACL injuries: mechanisms and risk factors. The Journal of the American Academy of Orthopaedic Surgeons. 2010 Sep;18(9):520-7.
42. Di Stasi SL, Snyder-Mackler L. The effects of neuromuscular training on the gait patterns of ACLdeficient men and women. Clinical Biomechanics. 2012 May 1;27(4):360-5.
43. Dwyer MK, Lewis CL, Hanmer AW, McCarthy JC. Do neuromuscular alterations exist for patients with acetabular labral tears during function? Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016 Jun 1;32(6):1045-52.
44. Garrison JC, Arnold A, Macko MJ, Conway JE. Baseball players diagnosed with ulnar collateral ligament tears demonstrate decreased balance compared to healthy controls. Journal of Orthopaedic & Sports Physical Therapy. 2013 Oct;43(10):752-8.
45. Hung YJ. Neuromuscular control and rehabilitation of the unstable ankle. World Journal of Orthopaedics. 2015 Jun 18;6(5):434-8.
46. Liu-Ambrose T, Taunton JE, MacIntyre D, McConkey P, Khan KM. The effects of proprioceptive or strength training on the neuromuscular function of the ACL reconstructed knee: a randomized clinical trial. Scandinavian Journal of Medicine & Science in Sports. 2003 Apr;13(2):115-23.
47. Owoeye OB, Palacios-Derflingher LM, Emery CA. Prevention of ankle sprain injuries in youth soccer and basketball: effectiveness of a neuromuscular training program and examining risk factors. Clinical Journal of Sport Medicine. 2018 Jul 1;28(4):325-31.
48. Read PJ, Oliver JL, Croix MB, Myer GD, Lloyd RS. Neuromuscular risk factors for knee and ankle ligament injuries in male youth soccer players. Sports Medicine. 2016 Aug;46(8):1059-66.
49. Szczygiel E, Sieradzki B, Masłoń A, Golec J, Czechowska D, Węglarz K, et al. Assessing the impact of certain exercises on the spatial head posture. International Journal of Occupational Medicine and Environmental Health. 2019 Feb 27;32(1):43-51.
50. Kim S, Jung J, Kim N. The effects of McKenzie exercise on forward head posture and respiratory function. The Journal of Korean Physical Therapy. 2019;31(6):351-7.
51. Moustafa IM, Diab AA, Hegazy F, Harrison DE. Does improvement towards a normal cervical sagittal configuration aid in the management of cervical myofascial pain syndrome: a 1-year randomized controlled trial. BMC Musculoskeletal Disorders. 2018 Dec;19(1):1-3.
52. Szczygiel E, Blaut J, Zielonka-Pycka K, Tomaszewski K, Golec J, Czechowska D, et al. The impact of deep muscle training on the quality of posture and breathing. Journal of Motor Behaviour. 2018 Mar 4;50(2):219-27.
53. Bae WS, Lee KC, Lee DY. The Effects of Dynamic Neuromuscular stabilization Exercise on Forward Head Posture and spine Posture. Medico Legal Update. 2019 Aug 8;19(2):670-5.
54. Birinci T, Mustafaoglu R, Mutlu EK, Ozdincler AR. Stretching exercises combined with ischemic compression in pectoralis minor muscle with latent trigger points: A single-blind, randomized, controlled pilot trial. Complementary Therapies in Clinical Practice. 2020 Feb 1;38:101080.
55. Do Youn Lee CW, Sung YB, Kim K, Lee HY. Changes in rounded shoulder posture and forward head posture according to exercise methods. Journal of Physical Therapy Science. 2017 Oct;29(10):1824-7.
56. Myer GD, Faigenbaum AD, Ford KR, Best TM, Bergeron MF, Hewett TE. When to initiate integrative neuromuscular training to reduce sports-related injuries in youth? Current Sports Medicine Reports. 2011 May;10(3):155-66.
57. Hewett TE, Ford KR, Xu YY, Khoury J, Myer GD. Effectiveness of neuromuscular training based on the neuromuscular risk profile. The American Journal of Sports Medicine. 2017 Jul;45(9):2142-7.
58. Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: prospective biomechanicalepidemiologic study. The American Journal of Sports Medicine. 2007 Jul;35(7):1123-30.
59. Cho J, Lee E, Lee S. Upper cervical and upper thoracic spine mobilization versus deep cervical flexors exercise in individuals with forward head posture: A randomized clinical trial investigating their effectiveness. Journal of Back and Musculoskeletal Rehabilitation. 2019 Jan 1;32(4):595-602.
60. Fathollahnejad K, Letafatkar A, Hadadnezhad M. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: a six-week intervention with a one-month follow-up study. BMC Musculoskeletal Disorders. 2019 Dec;20(1):1-8.
61. Shiravi S, Letafatkar A, Bertozzi L, Pillastrini P, Khaleghi Tazji M. Efficacy of abdominal control feedback and scapula stabilization exercises in participants with forward head, round shoulder postures and neck movement impairment. Sports Health. 2019 May;11(3):272-9.
62. Karimian R, Rahnama N, Ghasemi G, Lenjannejadian S. Photogrammetric Analysis of Upper Cross Syndrome among Teachers and the Effects of National Academy of Sports Medicine Exercises with Ergonomic Intervention on the Syndrome. Journal of Research in Health Sciences. 2019;19(3):e00450.
63. Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial. Journal of Manual & Manipulative Therapy. 2005 Jul 1;13(3):163-76.
64. Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. British Journal of Sports Medicine. 2010 Apr 1;44(5):376- 81.
65. Najafi M, Behpoor N. The effects of a selective corrective program on the scapula and shoulder joint posture in girls with rounded shoulder. Journal of Exercise Science and Medicine. 2013 Feb 19;4(2):31-47.
66. Benis R, Bonato M, Torre AL. Elite female basketball players’ body-weight neuromuscular training and performance on the Y-balance test. Journal of Athletic Training. 2016 Sep;51(9):688-95.
67. O’Driscoll J, Kerin F, Delahunt E. Effect of a 6-week dynamic neuromuscular training programme on ankle joint function: a case report. Sports Medicine, Arthroscopy, Rehabilitation, Therapy & Technology. 2011 Dec;3(1):1-7.
68. Myer GD, Ford KR, PALUMBO OP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. The Journal of Strength & Conditioning Research. 2005 Feb 1;19(1):51-60.
69. Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects onACL injury risk factors in” high-risk” versus” low-risk” athletes. BMC Musculoskeletal Disorders. 2007 Dec;8(1):1-7.
70. McLeod TC, Armstrong T, Miller M, Sauers JL. Balance improvements in female high school basketball players after a 6-week neuromuscular-training program. Journal of Sport Rehabilitation. 2009 Nov 1;18(4):465-81.
71. Wingfield K. Neuromuscular training to prevent knee injuries in adolescent female soccer players. Clinical Journal of Sport Medicine. 2013 Sep 1;23(5):407-8.
72. Pasanen K, Parkkari J, Pasanen M, Hiilloskorpi H, Mäkinen T, Järvinen M, et al. Neuromuscular training and the risk of leg injuries in female floorball players: Cluster Randomised Controlled Study. BMJ. 2008 Jul 1;337(7661), a295.
73. Hornbeck K, Peterson A. Neuromuscular training program reduces knee injuries among adolescent female soccer players. The Journal of Pediatrics. 2012 Nov 1;161(5):970-1.
74. Kerry C. Reliability of measuring natural head posture using the craniovertebral angle. Irish Ergonomics Review. 2003;37-41.
75. Singla D, Veqar Z, Hussain ME. Photogrammetric assessment of upper body posture using postural angles: a literature review. Journal of Chiropractic Medicine. 2017 Jun 1;16(2):131-8.
76. Borstad JD. Resting position variables at the shoulder: evidence to support a posture-impairment association. Physical Therapy. 2006 Apr 1;86(4):549-57.