Abstract
Rheumatoid meningitis (RM) is a rare condition seen in patients with longstanding rheumatoid arthritis (RA). It can present with a variety of neurological symptoms and is often mistaken for other neurological conditions, especially in the setting of immune suppression in these patients. We present a rare case of RM in an elderly woman with RA that presented with focal neurological symptoms and was eventually diagnosed on brain biopsy. Our case serves to highlight the diagnostic dilemmas faced while evaluating and treating patients presenting with such an exceedingly rare condition and the importance of multidisciplinary collaboration in the management of such complex patients.
Keywords
Cerebrospinal fluid, Rheumatoid arthritis, Rheumatoid meningitis
Abbreviations
RA: Rheumatoid Arthritis; RM: Rheumatoid Meningitis; MRI: Magnetic Resonance Imaging; CT: Computed Tomography; EEG: Electroencephalogram; LP: Lumbar Puncture; CSF: Cerebrospinal Fluid; HSV: Herpes Simplex Virus; WBC: White Blood Cell; RF: Rheumatoid Factor; CCP: Cyclinolytic Citrullinated Peptide
Introduction
Rheumatoid arthritis (RA) is a fairly common condition that presents with systemic involvement including joints and other organ systems. Rheumatoid meningitis (RM), however, is an exceedingly rare condition that is seen in longstanding RA patients. It can present in a variety of different manifestations including focal neurological deficits, stroke like symptoms or mimicking other conditions like cerebral abscesses or malignancies. Diagnosis is challenging and can often be delayed due to rarity of the condition and clinical and radiological mimicking of other diseases, especially in a setting of immune suppression. We present a case of a woman who presented with focal neurological symptoms in the setting of ongoing treatment for RA and needed extensive evaluation to diagnose her with RM followed by intensive treatment by rheumatology and neurology. Our case showcases the diagnostic challenges faced by clinicians when evaluating a patient with such a presentation and the evaluation offered to confirm a rare diagnosis like this. We hope to increase awareness of this condition to improve diagnostic accuracy and reduce delays in diagnosis due to rarity of this condition.
Case Presentation
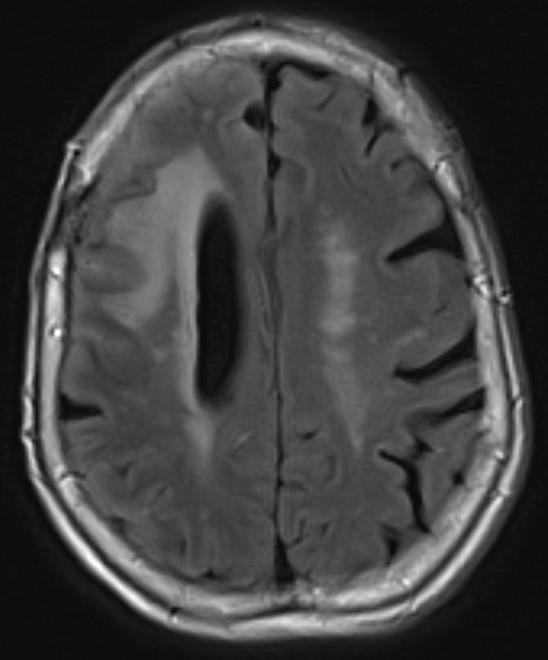
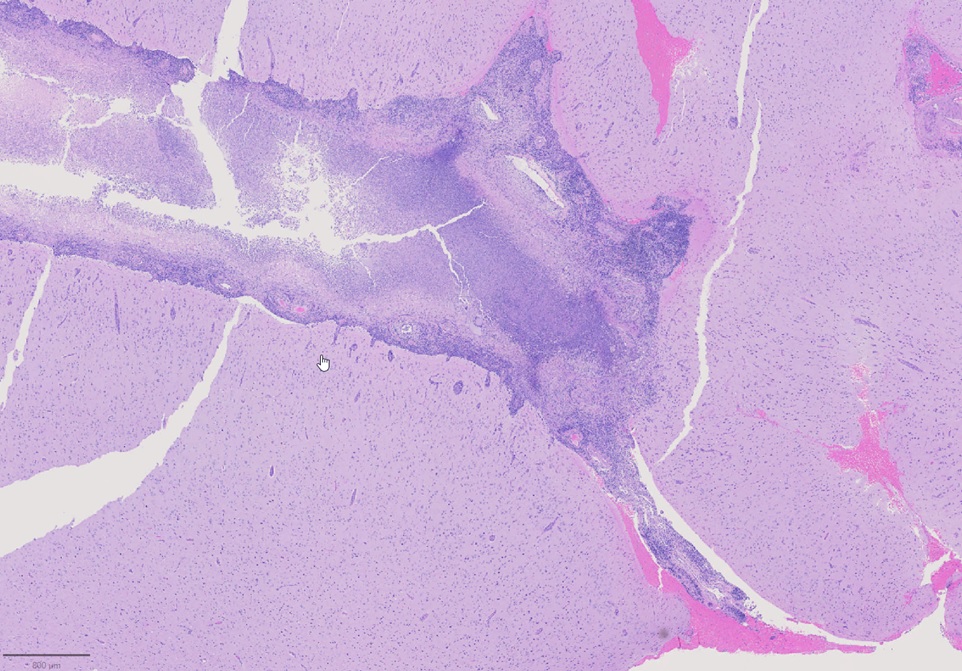
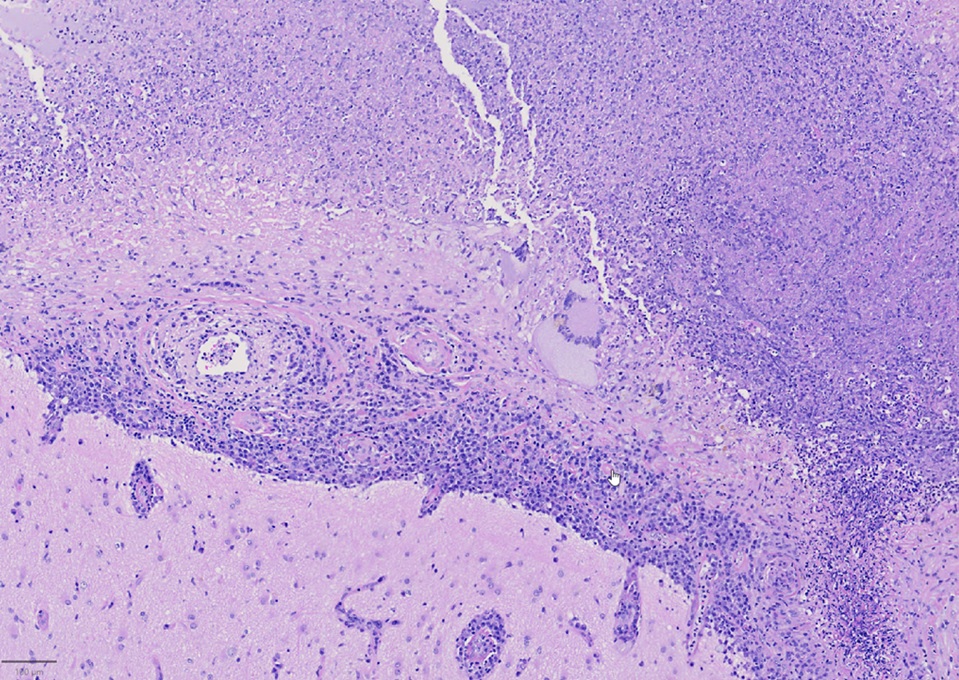
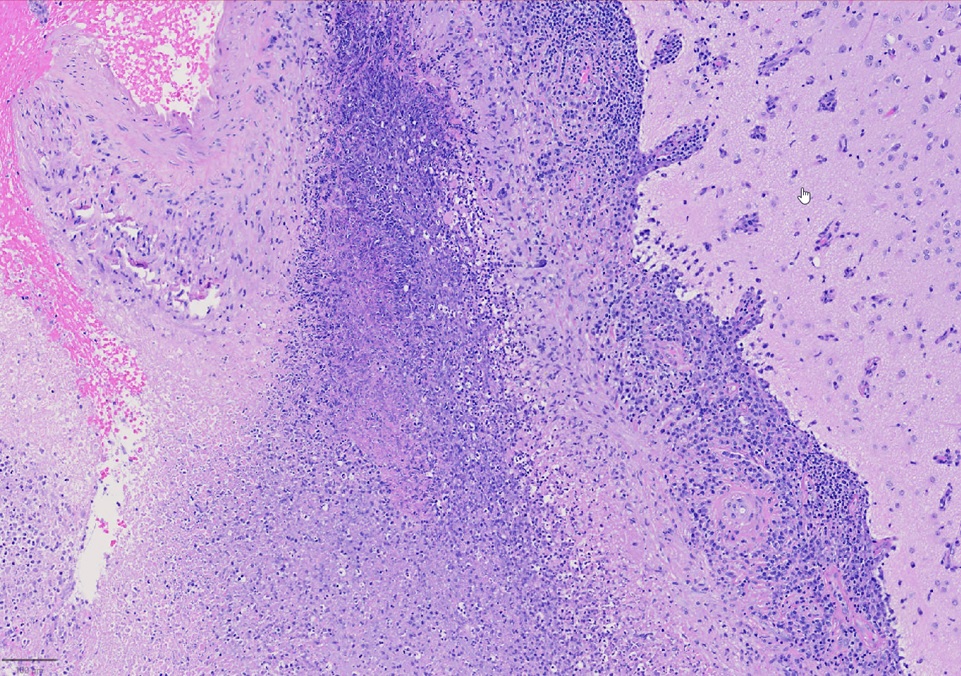
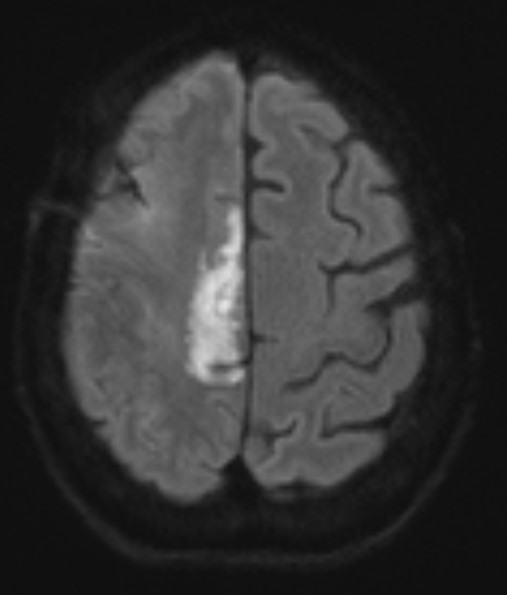
A 79-year-old right handed woman presented to a local hospital with left hemiparesis affecting her upper and lower extremities with mild left facial weakness for the last 2 weeks. She had a longstanding history of RA and had been off immune suppressant therapy for a few months due to improvement in symptoms. She had previously been on methotrexate and adalimumab in the past. She was evaluated with imaging and lumbar puncture (LP) at the time. MRI brain showed a semi-enhancing lesion over the right frontal lobe near the motor cortex with meningeal enhancement (Figure 1). CSF studies showed elevated protein at 65 and pleocytosis with WBC count of 47, 80% lymphocytes. CSF infectious panel was negative, but serum HSV-1 was positive. She reported a cold sore around this time as well. She was treated with broad spectrum antibiotics and acyclovir for 2 weeks. Infectious workup was otherwise negative. She did not have much improvement in her symptoms and was presented to our hospital 3 weeks later. Repeat CSF evaluation showed protein of 70 along with pleocytosis of 33 white blood cell (WBC), 75% lymphocytes. She received treatment with extended broad-spectrum antibiotics for 2 weeks. Rheumatological evaluation was negative for other signs of active RA. EEG showed bitemporal slowing with some quasi-periodic activity over the right temporal regions. She had some left arm shaking as well and was placed on levetiracetam for seizure prophylaxis. She did not have much improvement in her symptoms. A brain biopsy was performed which showed histopathological findings consistent with granulomatous inflammation confirming a diagnosis of RM (Figures 2-4). Labs showed highly elevated rheumatoid factor (RF) (>320) and anti-cyclinolytic citrullinated peptide (CCP) antibodies (>250). Rheumatology was consulted again and recommended high dose therapy with intravenous methylprednisolone for 5 days followed by resumption of immune modulating therapy. She developed a small right frontal ischemic stroke as a resultant of vasculitis from RM which caused exacerbation of left lower extremity weakness (Figure 5). She is kept on aspirin 81 mg daily for maintenance therapy for stroke prevention and levetiracetam for seizure prophylaxis along with daily prednisone and rituximab maintenance therapy for management of her RA / RM from rheumatology. She continues to work with physical therapy for her left hemiparesis which has shown some improvement. She sees rheumatology and neurology for continued follow up.
Figure 1. MRI brain showing right frontal lesion with cerebral edema and meningeal involvement.
Figure 2. Leptomeningeal inflammation and necrosis.
Figure 3. Leptomeningeal inflammation consisting of numerous plasma cells and rare giant cells with extensive necrosis.
Figure 4. Necrotizing granulomatous inflammation (rheumatoid nodule) involving leptomeninges.
Figure 5. Right frontal ischemic stroke in anterior cerebral artery territory from vasculitis related to RM.
Discussion
RA is a fairly common condition generally presenting with polyarthritis and orthopedic symptoms. It is highly uncommon for inflammatory cells to directly interact with the central nervous system in RA including RM [1].
There were 103 studies in all with 130 cases. Adults with an average age of 62 who had RM, whether or not they had previously been diagnosed with RA. A worse prognosis was linked to RA activity and length of disease progression. Transient focal neurological indications (64.6%), systemic symptoms (51.3%), episodic headaches (50.4%), and neuropsychiatric changes (47.7%) were the most frequent clinical presentations. Joint symptoms were only present in 27.4% of instances. Frontoparietal involvement was seen unilaterally or bilaterally on brain magnetic resonance imaging (MRI). Leptomeninges were impacted more frequently (82.88%) than pachymeninges. RF (89.71%), anti-CCP (89.47%), C-reactive protein (82.54%), and erythrocyte sedimentation rate (81.81%) were all shown to be higher in the lab results. Analysis of the cerebrospinal fluid revealed a rise in protein levels (76.14%), pleocytosis (85.19%), and a predominance of mononuclear cells (89.19%). In 72.52% of the patients, a biopsy was done. The primary induction therapy was corticosteroid pulse therapy. 31.17% of patients experienced a relapse of their illness, while 54.54% made a complete recovery [2].
According to Bathon's review, altered mental status, cranial neuropathies, hemiparesis/paraparesis, seizures, and headaches were the most common clinical manifestations of rheumatoid meningitis. Pachymeningitis and leptomeningitis might result from inflammatory rheumatic CNS illness, as in the case of our patient [1]. These individuals typically present with pachymeningitis, which is characterized by headaches and cranial neuropathies brought on by inflammation or dural fibrosis, if the dura tissue is primarily impacted. Mental status changes, abnormal gait, memory loss, depression, seizures, or paresis are more prevalent when the leptomeninges are damaged [3].
Cerebrospinal fluid findings in rheumatoid meningitis are variable and often non diagnostic [3]. Pleocytosis of lymphocytes is not usually present, although it was seen in our patient. Protein levels are commonly found to be higher. However, sampling from locations far from the lesion may result in falsely negative results [3,4]. There are now more precise indicators being found. The presence of RF in CSF is frequently employed as a diagnostic marker since very positive results clearly signify the presence of the disease [4]. TNF-α, IL-1, and IL-6 are among the inflammatory cytokines that are crucial to the pathophysiology of RA. In certain cases, large amounts of these cytokines have been found in the CSF of people who have RM, although it is unclear what these findings mean [4]. MRI with gadolinium enhancement is very helpful. Extraaxial high-intensity lesions that are diffusely or sporadically enhanced in FLAIR and DWI are thought to be signs of RA meningitis.
Histopathological findings eventually determine the diagnosis. In Bathon's assessment, 17 out of 19 victims had RM diagnosed after postmortem. An open brain biopsy was used to make the diagnosis in two cases. Meninges that had swollen nodules or plaques were frequently seen during a physical examination. Rheumatoid nodules, generalized meningeal inflammation, and vasculitis were three aberrant patterns that emerged through microscopic pathological analysis. The majority of the findings (68%) were nodules, which shared histological similarities with subcutaneous rheumatoid nodules. Nodules were seen in the choroid plexus (15%) and the cerebral meninges (92%). The spinal meninges were affected in two patients. The spinal cord or brain parenchyma had no nodules. In 63% of instances, it was discovered that the leptomeninges or pachymeninges had non-specific inflammatory infiltrates with mononuclear cells, primarily plasma cells, and less commonly necrosis and multinucleated giant cells. It is unclear why invading inflammatory cells prefer the meninges—in particular, the dura—to the brain parenchyma. Although brain parenchyma is not a large component of the dura, autoimmune reactions to collagen may be a factor [1]. In 37% of instances, vasculitis was found to have affected the meninges, spinal cord parenchyma, and the brain, as seen in our patient. Lymphocytes and plasma cells were present in the infiltrates of vessel walls. According to the authors, CNS rheumatoid nodules could be regarded as unique to CNS rheumatoid illness. The presence of plasma cells may help to identify CNS rheumatoid illness from other connective tissue disorders like systemic lupus erythematosus (SLE) or Sjögren syndrome in cases of non-specific chronic inflammatory infiltration by vasculitis or meningitis. Rheumatoid nodules are the most typical autopsy findings in people with RA. It is a non-specific inflammatory infiltrate among individuals with biopsy-diagnosed conditions, perhaps as a result of insufficient tissue sample [1,5].
Rheumatoid meningitis cannot be effectively treated according to any set rules. Corticosteroids combined with azathioprine, methotrexate, and cyclophosphamide have been advised [3-5]. With only corticosteroids, improvements have been made. This shows that immunosuppressants may not always be necessary during the treatment's induction phase, but they may be needed to taper or stop using corticosteroids in order to prevent any potential long-term side effects [6].
Difficulties in clinical diagnosis of RM are manifold and many of these are illustrated by our case. Symptomatology often overlaps with many other conditions, like infectious or inflammatory encephalitides, as stated in Tables 1 and 2. The presenting symptoms are not isolated to RM and can be seen in a variety of conditions. Clinical and radiological overlap with other conditions is the norm, rather than the exception [1,5]. The pre-existing use of immune modulating therapy for RA often favors clinical evaluations focused on infectious etiologies in immune suppressed patients and associated complications. The workup and empirical treatment with antibiotics for presumed or coexisting opportunistic infections often complicates the clinical picture and delays diagnosis due to the exhaustive approaches required in the evaluation of infectious encephalitides, especially in the immune suppressed setting [7]. Our patient was treated with antivirals at first after positive HSV tests in the serum that happened to be red herrings, illustrative of this point. CSF and radiological findings were fairly nonspecific and hardly suggestive of RM. The brain biopsy was performed only after failure of other therapies and extensive discussions with the patient, rheumatology and neurosurgery about the potential risks and benefits; a finding that strongly highlights the clinical difficulty and diagnostic dilemma seen in such cases contributing to diagnostic delay and additional morbidity seen in patients with RM. The presence of leptomeningeal enhancement with ischemic strokes or other signs of inflammation also raises the possibility of lymphoproliferative disorders or malignancies like lymphomas which manifest with similar presentations and duration of symptoms. CSF and radiological findings can often overlap with RM [8]. The possibility of lymphomas often raises sufficient concerns about the empirical use of steroids or immune suppressive therapies masking these conditions, delaying their use, and resulting in increased morbidity in RM patients as well.
|
Category of Conditions |
List of Conditions |
|---|---|
|
Vascular |
Primary CNS Vasculitis CNS Vasculitis Secondary to systemic vasculitis Antiphospholipid Syndrome |
|
Infectious |
Bacterial Meningitis – especially from recurrent foci like endocarditis, Lyme disease Viral Meningitis – recurrent HSV, adenoviruses Cerebral Abscess Fungal meningitis – histoplasmosis, etc. |
|
Inflammatory |
Autoimmune Encephalitis Multiple Sclerosis (Balo’s, etc) Acute Disseminating Encephalomyelitis (ADEM) Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) Drug induced Vasculitis / Vasospasm |
|
Malignant |
Glioma / Glioblastoma Cerebral metastases CNS / Systemic Lymphoma Histiocytosis |
|
Category of Conditions |
List of Conditions |
|---|---|
|
Vascular |
Recurrent ischemic stroke with hemorrhagic transformation Embolic strokes from infective endocarditis with hemorrhage Antiphospholipid Syndrome |
|
Infectious |
Bacterial Meningitis – especially from recurrent foci like endocarditis, Lyme disease Viral Meningitis – recurrent HSV, adenoviruses Cerebral Abscess Fungal meningitis – histoplasmosis, etc. |
|
Inflammatory |
Autoimmune Encephalitis Multiple Sclerosis (Balo’s, etc) Acute Disseminating Encephalomyelitis (ADEM) Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) Drug induced Vasculitis / Vasospasm |
|
Malignant |
Glioma / Glioblastoma Cerebral metastases CNS / Systemic Lymphoma Histiocytosis |
|
Congenital |
Cortical Dysplasia |
Morbidity and mortality from RM have often been high, often due to delays in diagnosis, lack of clear diagnostic criteria on clinical, radiological testing, the need for histopathological confirmation to prove the diagnosis, and the lack of consensus guidelines to establish the best lines of treatment [9]. Average survival after presentation from RM averaged around 4 years after presentation, but this has been improving due to better treatment guidelines and earlier implementation of brain biopsies to prove the diagnosis. Steroids remain the mainstay of therapy but there has been great improvement in morbidity and mortality with the additional use of immune therapies like rituximab or cyclophosphamide. TNF alpha inhibitors, often used in RA, have not shown to have great efficacy in RM. Increasing awareness, better consensus about treatment guidelines, faster use of biopsies and greater collaboration amongst multidisciplinary experts from rheumatology, neurology and other allied fields have greatly improved mortality over the years [9]. Morbidity often occurs due to misdiagnosis, the use of wrong or unrequired empirical therapies, delays in diagnosis or treatment and longer duration to performing a biopsy to conclusively prove the diagnosis [7,8]. Post mortem confirmation of diagnoses used to be the norm, but are thankfully fewer these days due to greater awareness of the condition and faster approaches by treating experts [9].
Multidisciplinary care is the norm, rather than the exception when it comes to treating these patients. Hospital internists represent the first line of attack when it comes to managing these patients, by first treating them and offering initial evaluations and empirical treatments for the more commonly seen types of encephalitides. Their monitoring of such patients to identify newer or unusual deficits of complications and recognition of failure of response to therapy is paramount in driving the clinical reasoning process to look for other less common conditions like RM. Moreover, they also help exclude other opportunistic infections and greatly expedite the process of arriving at the correct diagnosis. Neurologists are often involved in the care of these patients at an early stage, for management and diagnosis of various neurological symptoms and their probable etiologies. Neurological insight is imperative to look for unusual or uncommon clinical or radiological features that may hint towards the presence of uncommon conditions like RM, rather than garden variety infectious encephalitides. Neurological acumen is also essential to discern the lack of adequate responsiveness to empirical therapies and expedite the process of identification and confirmation of RM. Rheumatology forms the cornerstone in management of this condition. Many patients have pre-existing diagnoses of RA and are often on immune modulating therapy for the condition already. Rheumatological insight and supervision is essential in evaluating these patients to confirm the diagnosis and initiating and maintaining adequate therapies to achieve disease remission. They also remain as the primary drivers of therapy by ensuring correct and adequate dosages of immune modulating therapies for these patients. Infectious disease experts also form an important contributing team to ensure that opportunistic infections are ruled out as red herrings or treated adequately to enable better diagnosis of the underlying RM in the setting of immune suppression. Their input is valuable in ensuring that the correct infections are excluded appropriately, based on the clinical setting at presentation. Last but not least, neurosurgery and pathology have a major role to play in performing the brain biopsy and histopathological study of the biopsy samples to ensure clinical confirmation of the diagnosis in a timely and safe manner. Multidisciplinary collaboration thus greatly improves timeliness, accuracy, and safety of treatment of these patients, resulting in improved patient outcomes and reduced morbidity and mortality statistics in these cases [4,5,9].
Conclusion
RM remains an exceedingly rare condition with fewer than 150 patients described in the medical literature. It can manifest with myriad manifestations including meningoencephalitis, focal neurological deficits and can mimic many other conditions clinically and radiologically. It must be borne in mind while evaluating any patient with RA who presents with focal neurological deficits, especially if they show an atypical presentation or limited improvement with treatment of neurological symptoms. Exclusion of CNS infections is paramount, given the immune suppression in such patients. A brain biopsy remains the definitive diagnostic technique and must be considered without delay in such patients. Early consultation by rheumatology to aid in diagnosis and treatment would greatly expedite the process and improve outcomes resulting in limited morbidity and mortality. More awareness of this condition amongst clinicians would greatly facilitate better understanding and improved diagnosis and management of this rare condition. Multidisciplinary management of such patients by neurologists, rheumatologists, and neurosurgeons should be the norm to enable greatest quality of care.
Conflicts of Interest
The authors deny any conflicts of interest in this study.
Funding
There was no funding involved in the publication of this case report.
Ethical Guidelines
The authors report conformation with all accepted ethical guidelines for research in the publication of this case report. The patient and her family consented to the utilization of their data for the publication of this report.
Author Contributions
AS diagnosed and treated the patient and was involved in research and the writing of this manuscript and supervision of AR. AR was involved in research and writing of this manuscript as well. Both authors read and approved the final draft of the manuscript prior to publication. The authors are grateful to Jessica Bekker MD, Dept. of Pathology, SSM Hospital, Madison, WI for providing excellent quality histopathological images for publication in this case report.
References
2. Villa E, Sarquis T, de Grazia J, Núñez R, Alarcón P, Villegas R, et al. Rheumatoid meningitis: A systematic review and meta-analysis. European Journal of Neurology. 2021 Sep;28(9):3201-10.
3. Kupersmith MJ, Martin V, Heller G, Shah A, Mitnick HJ. Idiopathic hypertrophic pachymeningitis. Neurology. 2004 Mar 9;62(5):686-94.
4. Kato T, Hoshi K, Sekijima Y, Matsuda M, Hashimoto T, Otani M, Suzuki A, Ikeda S. Rheumatoid meningitis: an autopsy report and review of the literature. Clinical Rheumatology. 2003 Dec;22(6):475-80.
5. Jones SE, Belsley NA, McLoud TC, Mullins ME. Rheumatoid meningitis: radiologic and pathologic correlation. AJR American Journal of Roentgenology. 2006 Apr;186(4):1181-3.
6. Shimada K, Matsui T, Kawakami M, Hayakawa H, Futami H, Michishita K, et al. Diffuse chronic leptomeningitis with seropositive rheumatoid arthritis: report of a case successfully treated as rheumatoid leptomeningitis. Modern Rheumatology. 2009;19(5):556-62.
7. Dagra A, Lyerly M, Lucke-Wold B. Encephalitis and Meningitis: Indications for Intervention. Clinical Research (Westerville). 2023;4(1):8.
8. Nguyen A, Nguyen A, Dada OT, Desai PD, Ricci JC, Godbole NB, et al. Leptomeningeal Metastasis: A Review of the Pathophysiology, Diagnostic Methodology, and Therapeutic Landscape. Current Oncology. 2023 Jun 19;30(6):5906-31.
9. Pellerin D, Wodkowski M, Guiot MC, AlDhukair H, Blotsky A, Karamchandani J, et al. Rheumatoid Meningitis Presenting With Acute Parkinsonism and Protracted Non-convulsive Seizures: An Unusual Case Presentation and Review of Treatment Strategies. Frontiers in Neurology. 2019 Feb 27;10:163.