Abstract
The presence of vasa previa is a rare but serious complication for the fetus due to the occurrence of Benckiser’s hemorrhage. This report presents a clinical case of vasa previa diagnosed antenatally in a spontaneous pregnancy. Performing a transvaginal ultrasound combined with pulsed Doppler in pregnant women with risk factors for placenta previa or low-lying placenta allows diagnosis in nearly 98% of cases. Management of this condition may include preventive corticosteroid therapy between 28 and 32 weeks of gestation, patient bed rest, and prophylactic cesarean section between 34 and 37 weeks.
Keywords
Pregnancy, Transvaginal ultrasound, Vasa previa, Complication, Hemorrhage
Introduction
Vasa previa is the abnormal positioning of an umbilical vessel between the fetal presenting part and the internal cervical os, corresponding to a velamentous insertion on the fetal membranes in the lower uterine segment. Its incidence is estimated at between 0.4 and 0.6 per 1,000 pregnancies [1,2].
Although rupture of this vessel within the area of cervical dilation can occur at any time during pregnancy, it most commonly happens during spontaneous or artificial rupture of the membranes during labor. This complication can lead to severe fetal-origin hemorrhage, known as "Benckiser’s hemorrhage." It constitutes a true "acute exsanguination" of the fetus, resulting in death in 75 to 100% of cases [3].
Prenatal diagnosis is possible and can help improve newborn survival [4,5]. It is therefore essential to raise awareness among healthcare practitioners to enable effective screening of this condition and prevent its complications. We report a case of antenatally diagnosed vasa previa and its management at the maternity ward of the Jeanne Ebori Foundation Mother and Child University Hospital Center (CHUMEFJE) in Libreville.
Case Report
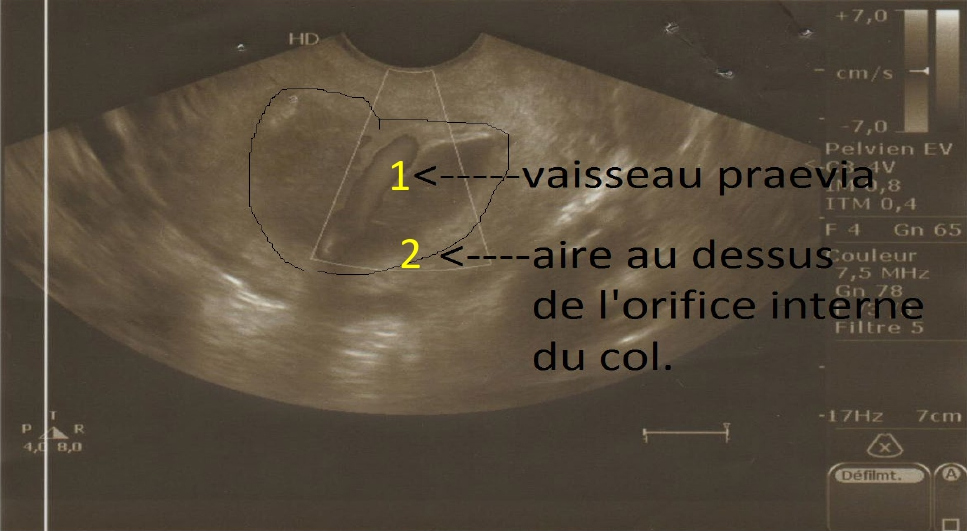
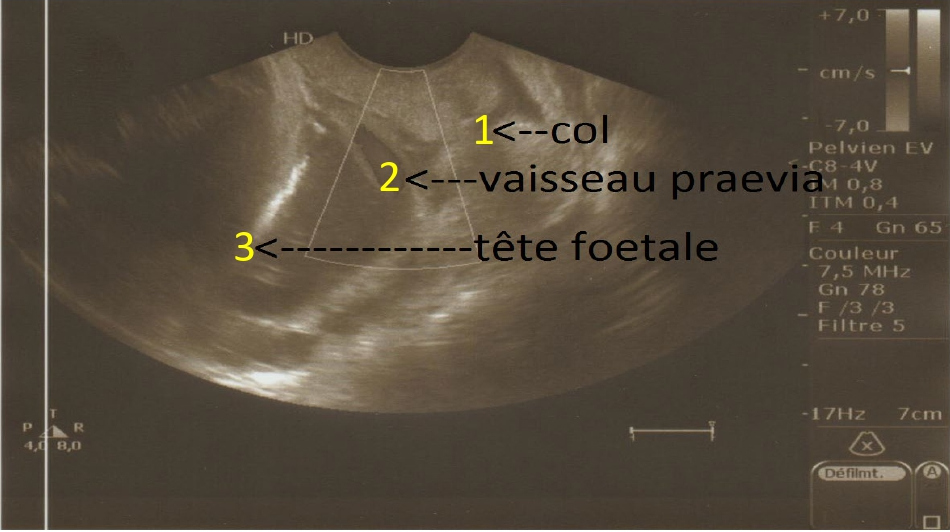
The patient, a 25-year-old woman, gravida 2 para 0, was being followed for a spontaneous singleton pregnancy that had progressed normally. Second-trimester obstetric ultrasound revealed a low-lying posterior placenta, and this placental location was confirmed at 32 weeks of gestation. A transvaginal ultrasound combined with color Doppler was then performed to examine the lower uterine segment. It revealed a vasa previa overlying the internal cervical os (Figures 1 and 2). The patient, informed of the various possible complications and showing no major risk of preterm labor, was placed on home rest. Preventive corticosteroid therapy was administered, and a cesarean section was scheduled at 37 weeks of gestation.
Figure 1. Transvaginal ultrasound with color Doppler at 32 weeks of gestation: visualization of the vasa previa crossing the area above the internal cervical os. 1) Vasa previa, 2) Area above internal cervical os.
Figure 2. Transvaginal ultrasound with color Doppler at 32 weeks of gestation: visualization of the vasa previa between the presenting part and the internal cervical os. 1) Cervix, 2) Vasa previa, 3) Fetal head.
Despite numerous follow-up phone calls, the patient only presented to the CHUMEFJE maternity unit two weeks after her scheduled admission date—that is, at 39 weeks of gestation.
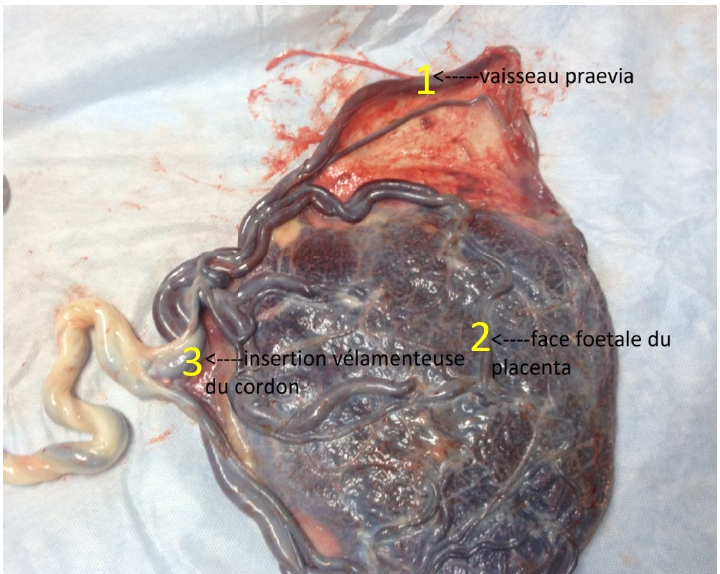
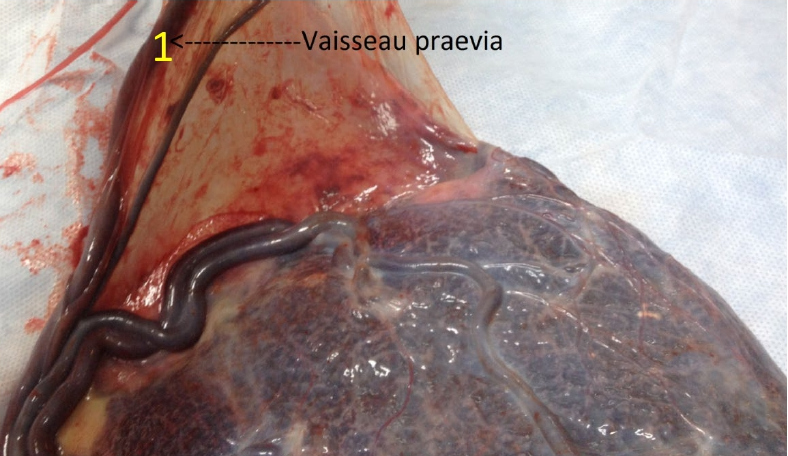
She was in early labor with spontaneous rupture of membranes that had occurred three hours earlier. The fetus was alive, with a heart rate of 140 beats per minute. Speculum examination confirmed the presence of clear amniotic fluid of endocervical origin without metrorrhagia. Vaginal examination revealed a mobile cephalic presentation, a cervix that was 70% effaced and 2 cm dilated. Given the patient’s pregnancy history (vasa previa diagnosed on third-trimester ultrasound), an emergency cesarean section was proposed. The procedure resulted in the birth of a healthy newborn with an Apgar score of 10 at both the 1st and 5th minutes. Macroscopic examination of the placenta revealed a large-caliber vasa previa associated with velamentous insertion of the umbilical cord with vessel ramification over the membranes (Figures 3 and 4). The immediate postoperative course was uneventful.
Figure 3. Placenta: velamentous cord insertion and vasa previa—macroscopic view. 1) Vasa previa, 2) Fetal side of the placenta, 3) Velamentous cord insertion.
Figure 4. Vasa previa — macroscopic view. 1) Vasa previa.
Discussion
The presence of a vessel between the fetal presenting part and the internal os of the gravid uterus is a rare but serious obstetric complication. Its frequency varies between 0.1% and 1% depending on the authors [6–8]. We report 1 case out of 2,700 deliveries (0.03%).
We did not specifically investigate the risk factors for the occurrence of vasa previa. However, nulliparity and the low placental insertion observed in our patient, with a history of intrauterine procedures, velamentous cord insertion, the presence of aberrant cotyledons, and pregnancies resulting from in vitro fertilization (IVF), are identify as risk factors in our study [6,9,10].
In the past, vasa previa was diagnosed clinically by palpating the vessel over the membranes during labor, or by visualizing it during an amnioscopy [11]. This method rarely allows prevention of complications. In the vast majority of cases, the diagnosis was made retrospectively, during placental examination after the occurrence of intrapartum hemorrhage associated with fetal bradycardia or a sinusoidal heart rate pattern [12]. This severe fetal-origin hemorrhage, known as Benckiser’s hemorrhage, results from the rupture of the vasa previa during spontaneous or artificial membrane rupture. During this complication, there’s no pain, and the general condition is kept, while the fetus faces immediate and severe acute hypoxia (hypovolemia) [6].
However, this clinical presentation may be atypical, with hemorrhage occurring some time after membrane rupture. For instance, Regis et al. [3] reported a case where hemorrhage occurred at 5 cm of cervical dilation and 6 hours after membrane rupture. Other authors have also described this delayed hemorrhagic onset [12–14]. Secondary hemorrhage may be explained by progressive enlargement of the rupture site, which subsequently dissects the vasa previa.
Vasa previa can be detected during the antenatal period through a transvaginal ultrasound associated with color and pulsed Doppler as early as the second trimester of pregnancy [4,7 8,15,16]. This examination has a specificity of 99% and allows visualization in the lower uterine segment of linear or tubular structures near the internal cervical os, situated between the presenting part and the lower segment. Color and pulsed Doppler reveal vascular flow [7,10,16]. Numerous guidelines agree on the necessity of this imaging as early as the second trimester of pregnancy, specifying both the placental insertion site and the umbilical cord insertion point [17,18]. Thus, in any case of low-lying or previa placenta, discovered on suprapubic ultra sound, a transvaginal ultrasound combined with color and pulsed Doppler will be essential to screen for vasa previa [5,7,8].
Antenatal diagnosis of vasa previa significantly improves neonatal outcomes. In fact, in the study by Oyelese et al. [19], which analyzed 155 cases of vasa previa, the neonatal survival rate was 97% among patients with antenatal diagnosis, compared to 44% without it; the neonatal blood transfusion rate was 3.4% versus 58%. Other studies support these findings [13,14]. This discovery before labor allows to anticipate hemorrhagic complications of vasa previa and neonatal prognosis.
Once the diagnosis is established, several authors recommend placing the patient on bed rest to prevent the onset of labor or any premature rupture of membranes before term [12,20]. A cesarean section is then scheduled once fetal maturity is deemed sufficient—either spontaneously based on gestational age or following the administration of preventive corticosteroid therapy [4,7,12,19,20]. In our context, patients often resist planned cesarean sections. This stems from a general fear of surgery.
In the event of premature rupture of membranes, an immediate cesarean section must be performed, even in the absence of hemorrhage, which may be delayed [12,20].
Conclusion
Although rare, the presence of vasa previa is highly risk for the fetus. Antenatal diagnosis can be made using transvaginal ultrasound combined with pulsed Doppler focused on the lower uterine segment and the internal cervical os. Management involves performing a planned cesarean section before the onset of labor and prior to any premature rupture of membranes.
References
2. Nohuz E, Boulay E, Gallot D, Lemery D, Vendittelli F. Can we perform a prenatal diagnosis of vasa previa to improve its obstetrical and neonatal outcomes? J Gynecol Obstet Hum Reprod. 2017 Apr;46(4):373–77.
3. Régis C, Mubiayi ND, Devisme L, Subtil D. Hémorragie de Benckiser: grave et inévitable? [Benckiser's hemorrhage: severe and inevitable?]. J Gynecol Obstet Biol Reprod (Paris). 2006 Sep;35(5 Pt 1):517–21.
4. Matsuzaki S, Kimura T. Vasa Previa. N Engl J Med. 2019 Jan 17;380(3):274.
5. Ruiter L, Kok N, Limpens J, Derks JB, de Graaf IM, Mol BW, et al. Systematic review of accuracy of ultrasound in the diagnosis of vasa previa. Ultrasound Obstet Gynecol. 2015 May;45(5):516–22.
6. Yang M, Zheng Y, Li M, Li W, Li X, Zhang X, et al. Clinical features of velamentous umbilical cord insertion and vasa previa: A retrospective analysis based on 501 cases. Medicine (Baltimore). 2020 Dec 18;99(51):e23166.
7. Oyelese Y, Javinani A, Gudanowski B, Krispin E, Rebarber A, Akolekar R, et al. Vasa previa in singleton pregnancies: diagnosis and clinical management based on an international expert consensus. Am J Obstet Gynecol. 2024 Dec;231(6):638.e1-638.e24.
8. Coleman G, Venables H. Is ultrasound screening for vasa praevia clinically justified and a financially viable screening test? A literature review. Ultrasound. 2018 Feb;26(1):6–15.
9. Society of Maternal-Fetal (SMFM) Publications Committee; Sinkey RG, Odibo AO, Dashe JS. #37: Diagnosis and management of vasa previa. Am J Obstet Gynecol. 2015 Nov;213(5):615–9.
10. Bronsteen R, Whitten A, Balasubramanian M, Lee W, Lorenz R, Redman M, et al. Vasa previa: clinical presentations, outcomes, and implications for management. Obstet Gynecol. 2013 Aug;122(2 Pt 1):352–57.
11. GINGOTTI M, GANDOUR A, MOXHON E. Diagnostic d'un vaisseau prævia par l'amnioscopie: intérêt de l'accouchement programmé: a propos d'un cas. Revue française de gynécologie et d'obstétrique. 1992;87(2):87–9.
12. Ismail KI, Hannigan A, O'Donoghue K, Cotter A. Abnormal placental cord insertion and adverse pregnancy outcomes: a systematic review and meta-analysis. Syst Rev. 2017 Dec 6;6(1):242.
13. Ebbing C, Johnsen SL, Albrechtsen S, Sunde ID, Vekseth C, Rasmussen S. Velamentous or marginal cord insertion and the risk of spontaneous preterm birth, prelabor rupture of the membranes, and anomalous cord length, a population-based study. Acta Obstet Gynecol Scand. 2017 Jan;96(1):78–85.
14. Zhang W, Oyelese Y, Javinani A, Shamshirsaz A, Akolekar R. The potential impact of universal screening for vasa previa in the prevention of stillbirths. J Perinat Med. 2024 Sep 9;52(9):939–45.
15. Chanu SM, Dasari P, T C, Pegu B, T R. Prenatal Ultrasound Diagnosis of Vasa Previa With Careful Intraoperative Management: A Case Report. Cureus. 2024 Mar 5;16(3):e55578.
16. Ward S, Sun Z, Maresse S. Current practice of placental cord insertion documentation in Australia - A sonographer survey. Australas J Ultrasound Med. 2023 Jul 26;26(3):157–68.
17. Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, et al. ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol. 2013 Jan;41(1):102–13.
18. Li XZ, Wang H, Song J, Liu Y, Lin YQ, Sun ZX. Ultrasonographic diagnosis of intussusception in children: a systematic review and meta‐analysis. J Ultrasound Med. 2021 Jun;40(6):1077–84.
19. Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, Tovbin Y, et al. Vasa previa: the impact of prenatal diagnosis on outcomes. Obstet Gynecol. 2004 May;103(5 Pt 1):937–42.
20. Bohîlțea RE, Cîrstoiu MM, Ciuvica AI, Munteanu O, Bodean O, Voicu D, et al. Velamentous insertion of umbilical cord with vasa praevia: case series and literature review. J Med Life.2016;9(2):126–9.