Abstract
This is a high-value care-based quality improvement project that was carried out to decrease inappropriate troponin testing in the emergency department (ED) of a tertiary health institution in the United States with the goal of promoting evidence-based practices, minimizing waste, and enhancing the quality of care.
Keywords
High sensitivity troponin, Myocardial infarction, Myocardial injury, Myocardial ischemia
Abbreviations
ACS: Acute Coronary Syndrome; HST: High Sensitivity Troponin; TT: Troponin Testing; ATT: Appropriate Troponin Testing, ITT: Inappropriate Troponin Testing; ED: Emergency Department
Background
Cardiac Troponin I and T are sensitive biological markers of cardiac Injury with high sensitivity troponin, being the gold standard for measuring myocardial cell Injury [1]. The Joint American College of Cardiology (ACC) / America Heart Association (AHA) task force recommends ordering troponin only if there is clinical suspicion of acute coronary syndrome (ACS) [2].
Inappropriate testing results in unnecessary follow-up investigations, consultations, interventions, inadvertent patient harm (physical and psychological), and increased healthcare costs [3-5]. At our institution, it was observed that many patients who presented to the ED underwent troponin testing even in the absence of clear clinical suspicion for ACS, some of these patients underwent repeat testing that eventually had no clinical relevance in terms of their presentation, definitive care, and outcomes. It however, resulted in overutilization of hospital resources, diagnostic distraction, and increased health care costs. This quality improvement project was conducted to change the narrative by promoting the delivery of high-value, evidence-based care to our patients while minimizing healthcare waste.
Objectives
The objective of this project is firstly to decrease inappropriate troponin ordering in the emergency department. Secondly, to promote compliance with evidence-based guidelines. Thirdly, to decrease overutilization of hospital resources and to ultimately improve patient outcomes.
Figure 1. This Figure depicts the summary of this study which is to promote evidence-based guideline directed troponin testing for evaluation of acute coronary syndrome in the emergency department.
Methods
A retrospective chart review of 1071 patients who underwent high sensitivity troponin (HST) testing during their initial presentation to the ED was performed. Data for three randomly selected months (March, May, and July 2023) was obtained from the hospital pathology laboratory. All the troponin tests (TT) were reviewed to determine their appropriateness. A TT is considered appropriate if it meets any of these two criteria: Firstly, the test was ordered for a patient presenting with clinical or electrocardiographic features that can be attributed to cardiac ischemia (angina or angina equivalent symptoms) in accordance with the joint task force recommendation to order troponin only if there is clinical suspicion of ACS. Secondly, if the TT ordered altered patients’ management in any way or made a difference in the course of patient care. A TT that fulfills at least one of the criteria is considered appropriate while those that do not fulfill any of the criteria are considered inappropriate. Binary (yes/no) data were collected for both research questions.
Results
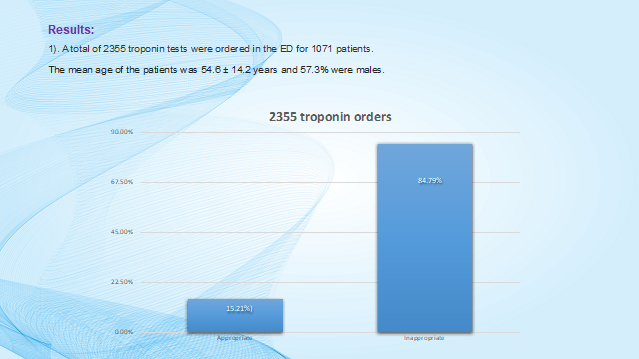
A total of 2355 troponin tests were ordered in the ED for 1071 patients. The mean age of the patients was 54.6 ± 14.2 years and 57.3% were males. 358/2355(15.21%) were considered appropriate while 1997/2355 (84.79%) were considered inappropriate as shown in Figure 2.
Figure 2. As shown in the Figure, more than 80% (84.79%) of the troponin tests were ordered in the absence of clinical suspicion for acute coronary syndrome and those troponin tests were also found not to alter patient management or the course of patient care in any way. On the other hand, approximately 15% (15.21%) of the troponin tests were ordered in the context of patients presenting with symptoms suspicious for acute coronary syndrome and/or were found to ultimately alter patient’s management. Abbreviations: ED: Emergency Department.
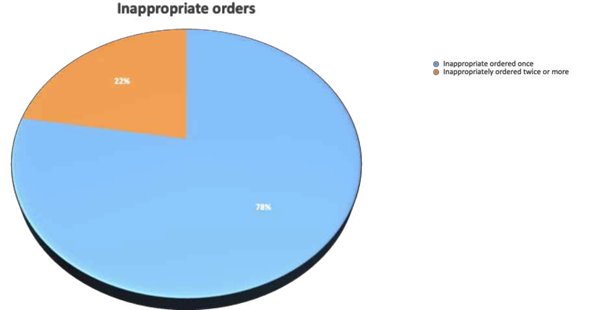
Also, 1549/1997(77.6%) of the inappropriate orders were inappropriately ordered once while 447/1997(22.4%) were inappropriately repeated twice or more (Figure 3).
Figure 3. Pie chart showing inappropriate orders.
The main reasons observed for the inappropriate troponin tests include the following: 1) Triage orders: in which the orders were placed by the triage nurses or triage personnel before a patient is assessed by physicians. 2) Random tick box practice: whereby routine orders that are commonly placed in the ED were simply ticked on the EMR and ordered without tailoring each order towards patient’s specific presentation or complaints. 3) Order sets: it was observed that some order sets including the sepsis order sets, stroke order sets etc. included troponin test which is not clinically indicated. 4) No prior assessment: In this case, physicians immediately place routine orders including troponin once a patient is assigned to them prior to clinically assessing these patients (Figure 4).
Figure 4. Observed reasons for the inappropriate orders.
Table1 showing presenting complaints for which troponin was ordered appropriately and inappropriately.
|
Appropriate |
Inappropriate |
|
Chest pain |
Gastrointestinal bleed |
|
Radiating pain: Jaw, epigastric, left shoulder |
Dysuria |
|
Shortness of breath |
Fever |
|
Altered mental status |
Weakness |
|
Cardiac arrest |
Numbness |
|
Syncope |
Diabetic foot |
|
|
Right upper quadrant pain |
|
|
Diarrhea + vomiting |
|
|
Fall |
|
|
Fracture |
|
|
Abdominal distention |
|
|
Headache |
Table 2 shows diagnosis upon discharge for the appropriate and inappropriate orders.
|
Appropriate |
Inappropriate |
|
Acute coronary syndrome |
Upper GI bleed |
|
Angina |
Sepsis |
|
CHF exacerbation |
Pyelonephritis |
|
COPD |
Stroke |
|
Asthma exacerbation |
Gastroenteritis |
|
Fluid overload (ESRD on dialysis) |
Diabetic ketoacidosis |
|
Pneumonia |
Diabetic foot ulcer |
|
Costochondritis |
Ascites requiring paracentesis |
|
Musculoskeletal pain |
ESRD on hemodialysis |
|
Biliary colic |
Elevated troponin* |
|
Cholecystitis |
|
|
Elevated troponin* |
|
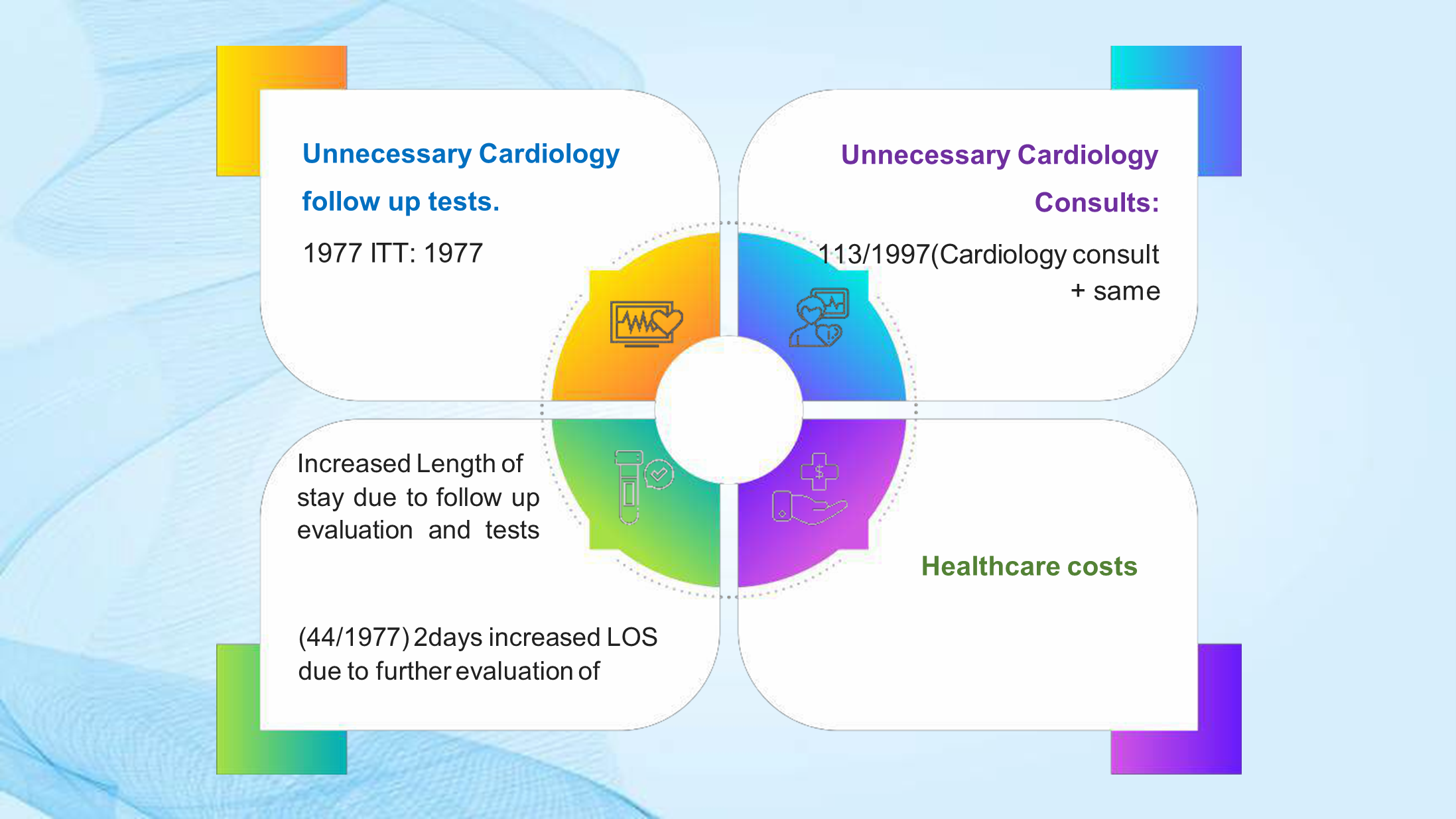
Secondary outcomes resulting from inappropriate troponin testing are presented in Figure 5.
Figure 5. The variables in this Figure highlight the secondary outcomes that resulted from inappropriate troponin testing: 1) Unnecessary follow up tests: Automatically all the patient that had troponin ordered either appropriately or inappropriately were also found to have EKG and CK ordered. This is an automated electronic order set up; hence the more inappropriate troponin test ordered the more unnecessary follow up tests including EKG and CK ordered. 2) Some of the inappropriate tests ordered were positive indicating some underlying chronic myocardial injury which was deduced from patient’s chart review which showed chronically elevated troponin in the absence of clinical symptoms of ACS or EKG changes. 5.7% (113/1977) of the patients with ITT had cardiology consultations which were considered inappropriate consultations since these consults culminated in same day sign offs by the consultants. 3) Some of the patients had increased length of stay of approximately 2 days either arising from waiting for consultants to evaluate patients, needing to trend troponin test or wait for follow up investigation results. 4) The unnecessary troponin test in isolation resulted in hundreds of thousands of health care costs which could even be more significant when additional costs of follow up test, consults and length of stay are incorporated into the cost of care. Abbreviations: ACS: Acute Coronary Syndrome; CK: Creatine Kinase; EKG: Electrocardiogram; ITT: Inappropriate Troponin Testing; LOS: Length of Stay.
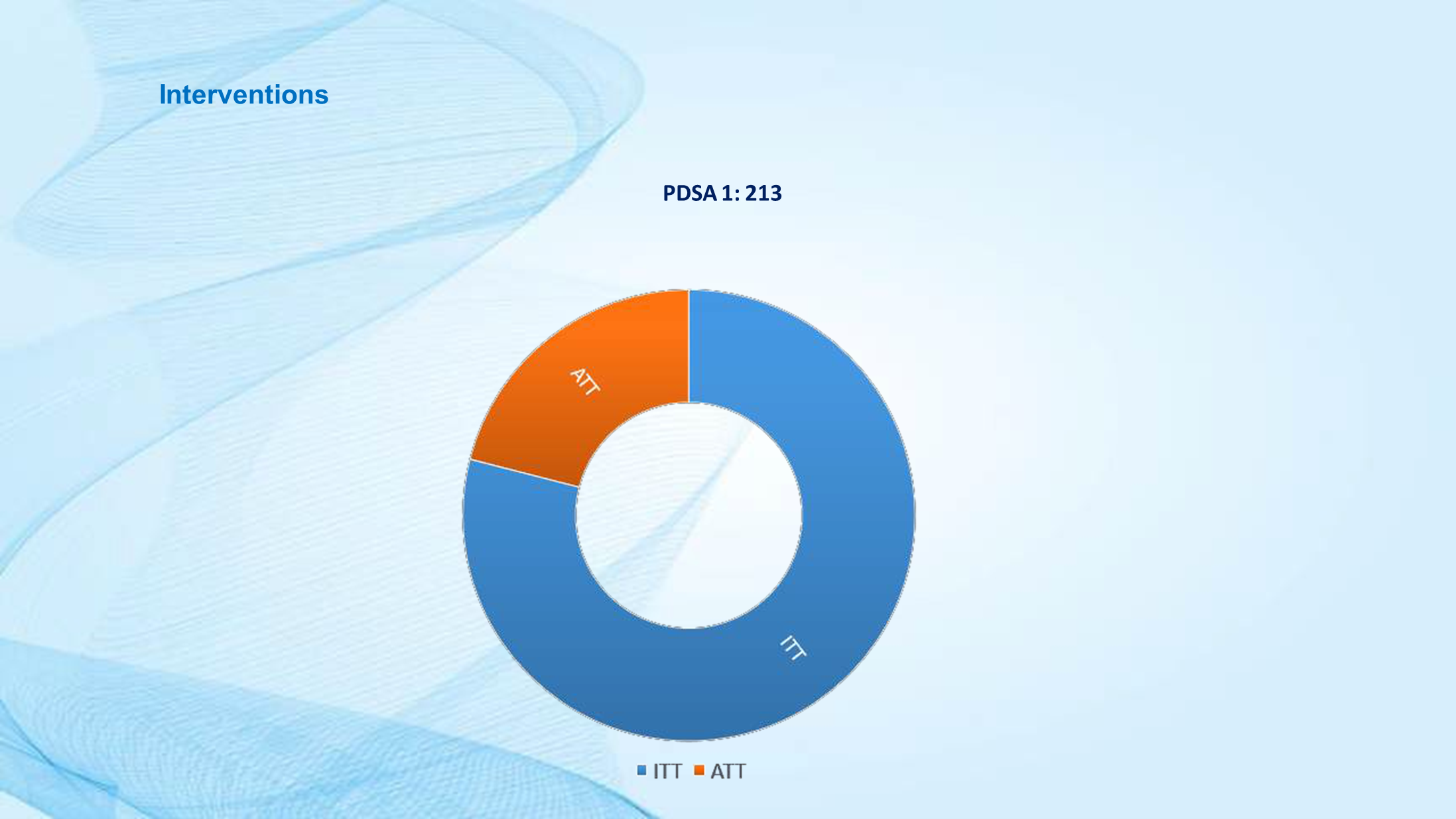
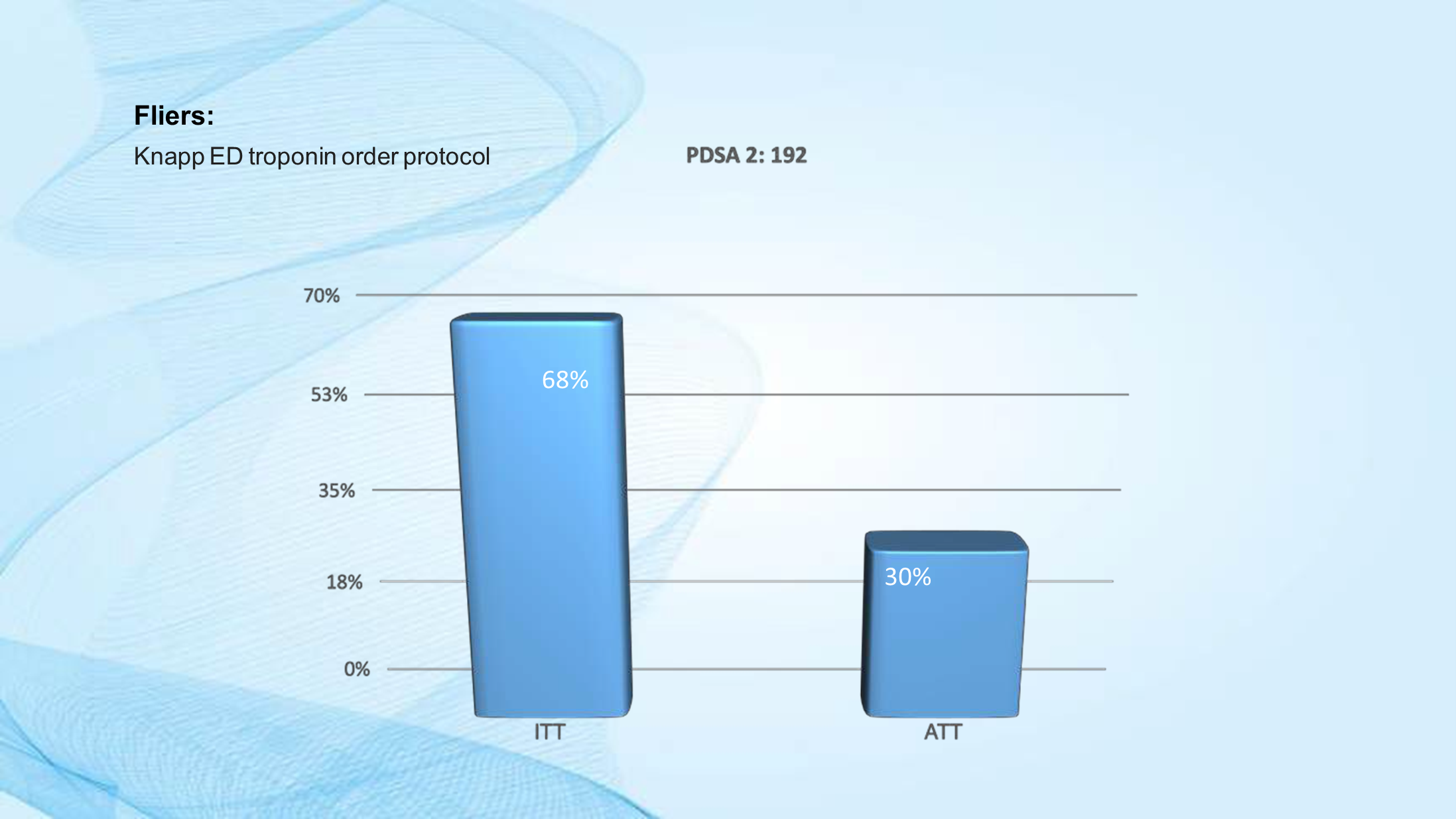
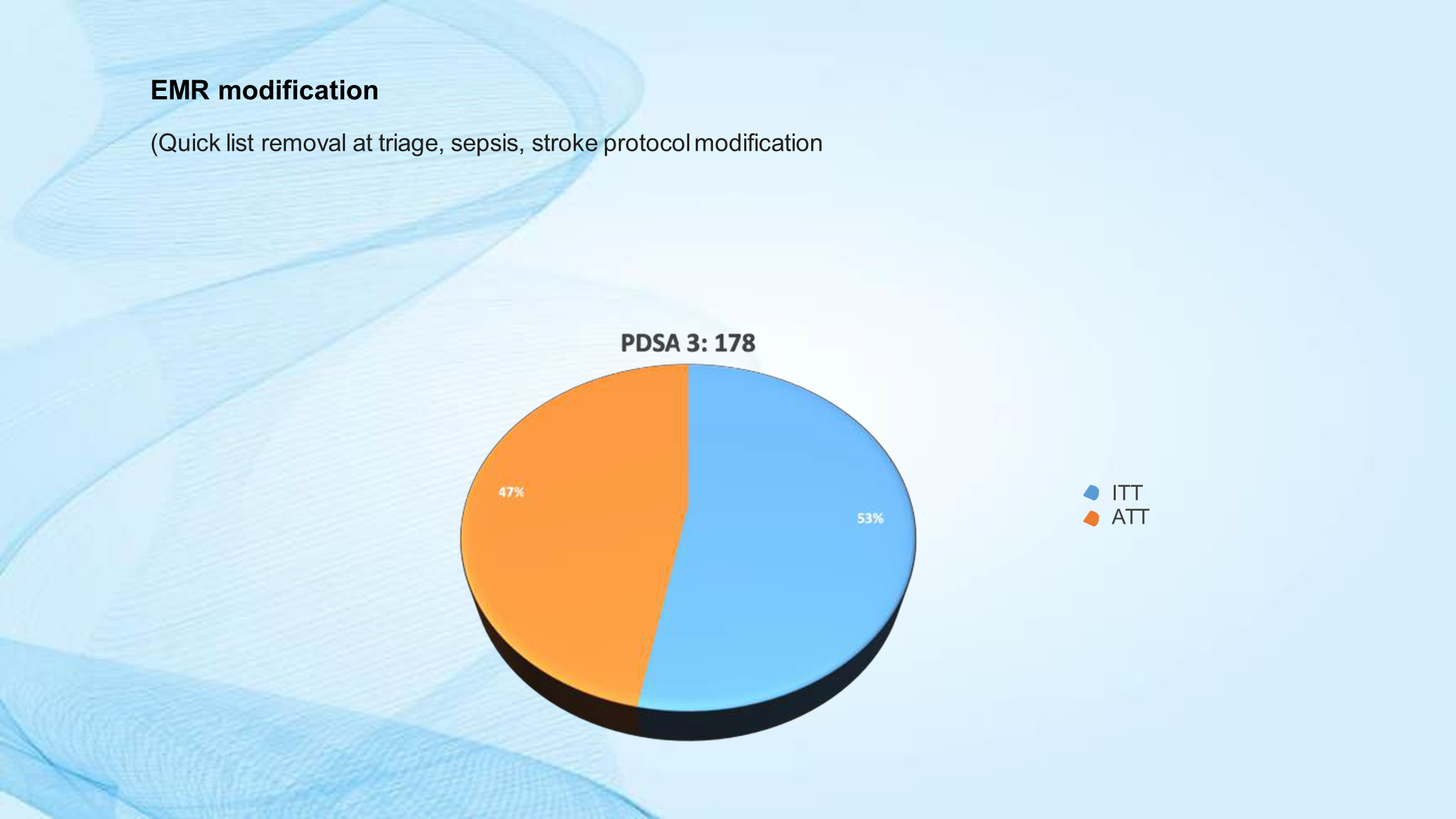
Interventions implemented to decrease inappropriate testing are presented in Figures 6-10.
Figure 6. Education, Presentation, Fliers. The initial intervention done was to educate ER personnel on when to suspect ACS, diagnostic relevance of the troponin tests and current guidelines on troponin testing. This intervention resulted in a modest decrease in ITT from 84.79% to 79%. Abbreviations: ACS: Acute Coronary Syndrome; ATT: Appropriate Troponin Testing; ER: Emergency Room; ITT: Inappropriate Troponin Testing; PDSA: Plan-Do-Study-Act.
Figure 7. The Troponin order algorithm was created to guide ED clinicians, NP, PA on the steps to follow when ACS is suspected. The algorithm is attached in the supplementary material section. This intervention resulted in a modest decrease in ITT from 79% to 68%. Abbreviations: ACS: Acute Coronary Syndrome; ATT: Appropriate Troponin Testing; ED: Emergency Department; ITT: Inappropriate Troponin Testing; NP: Nurse practitioner; PA: Physician Assistant; PDSA: Plan-Do-Study-Act.
Figure 8. EMR modification: Specific modifications were made on our EMR including removal of troponin from the quick list order set that are commonly ordered at triage, troponin was also removed from the sepsis and stroke order sets. This resulted in the reduction of ITT from 68% to 53%. Abbreviations: ATT: Appropriate Troponin Testing; EMR: Electronic Medical Record; ITT: Inappropriate Troponin Testing; PDSA: Plan-Do-Study-Act.
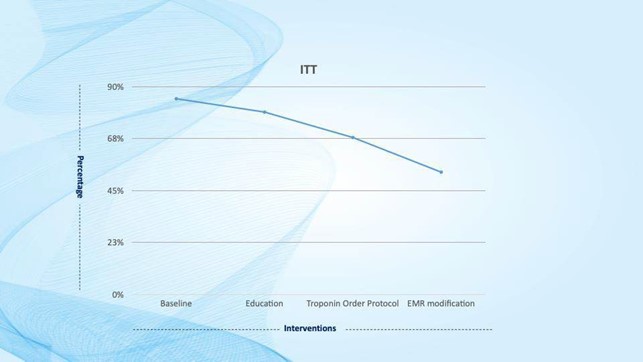
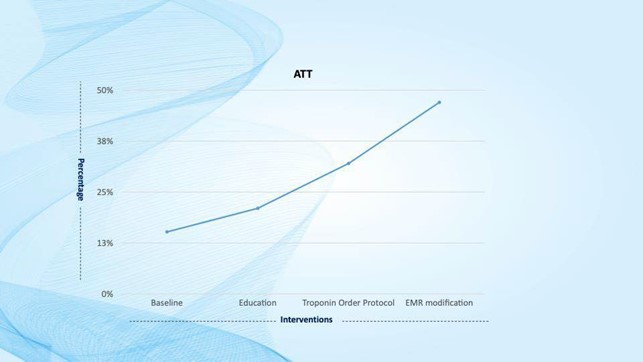
Figure 9. Decreasing inappropriate troponin order trend over three months after implementation of the interventions. Abbreviations: EMR: Electronic Medical Record; ITT: Inappropriate Troponin Testing.
Figure 10. Increasing appropriate troponin order trend over three Months after implementation of the Interventions (Over the subsequent three months (Figures 8 and 9) showed a gradual increase in ATT from 15.2% preintervention to 43% post intervention and a decrease in ITT from 84.79% preintervention to 53% post intervention). Abbreviations: ATT: Appropriate Troponin Testing; EMR: Electronic Medical Record; ITT: Inappropriate Troponin Testing.
Conclusion
Troponin should be ordered only if there is clinical suspicion of acute coronary syndrome. It should not be used as a discriminative tool for reaching diagnostic conclusions in the absence of an appropriate clinical history or examination. Inappropriate testing results in additional workups, overdiagnosis, unnecessary consultations and treatments, risk of patient harm (physical and psychological), increased length of stay, and health care costs. This is a call for Institutions to create and implement a testing strategy or protocol that meets their local needs while incorporating updated guidelines.
References
2. Kontos MC, de Lemos JA, Deitelzweig SB, Diercks DB, Gore MO, et al. 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the emergency department: a report of the American College of Cardiology solution set oversight committee. Journal of the American College of Cardiology. 2022 Nov 15;80(20):1925-60.
3. Koch C, Roberts K, Petruccelli C, Morgan DJ. The frequency of unnecessary testing in hospitalized patients. The American Journal of Medicine. 2018 May 1;131(5):500-3.
4. Alrusaiyes MF, Qureshi MA. Appropriateness of troponin testing in emergency department at a tertiary care hospital in Saudi Arabia. Saudi Medical Journal. 2022 May;43(5):526-9.
5. Ehteshami Afshar A, Sabharwal MS, Casso Dominguez AA, Dianati Maleki N, Tamis-Holland JE, El Hayek G, et al. Troponin Testing in the Emergency Setting: Analysis of Appropriateness. Circulation: Cardiovascular Quality and Outcomes. 2015 May;8(suppl_2):A279.