Abstract
Diabetic foot and ankle reconstruction is a difficult area of surgery in which to achieve ideal outcomes. The goal for a majority of cases in this surgical field is to achieve a plantigrade foot that can function throughout the gait cycle in shoes with or without a brace. There are multiple biomechanical, biochemical, neurological, vascular, infectious, and social factors that can influence the likelihood of achieving those goals. The effect of the Achilles’ tendon on the gait cycle, through its effects on joint function, is the greatest determinant of non-rigid deformity in diabetic feet. In order to improve the chance of a desired outcome, the Achilles tendon should be assessed for any possible pathologies. For many patients, the addition of the simple technique of a percutaneous Achilles’ tendon release to a surgical case is powerful enough to address multiple biomechanical issues and prevent below-knee amputations.
Keywords
Achilles Tendon, Foot and Ankle Surgery, Foot Surgery, Ankle Surgery, diabetic foot, diabetic feet, knee amputations, amputations, amputation,
Introduction
The goal of reconstructive foot and surgery for diabetic foot pathologies is to create a plantigrade foot that is braceable and has low risk of ulcer formation or recurrence. Experienced surgeons are cognizant that foot pathologies are defined in three planes: frontal, transverse and sagittal. The Achilles’ tendon is the chief deforming force in the foot along the sagittal plane [1]. For example, to improve the sagittal plane component in patients with Charcot joint disease midfoot collapse, surgeons will choose to combine their osteotomy and arthrodesis techniques with lengthening of the Achilles’ tendon [2]. In patients with significant contractures in the Achilles’ tendon, the ankle joint cannot proceed beyond ninety degrees, i.e. beyond parallel from the ground [3]. The forefoot must clear the ground in order for the gait cycle to proceed beyond forefoot loading and will utilize the subtalar joint to increase the amount of dorsiflexion the foot can achieve [4]. The abnormal utilization of the subtalar joint places significant strain on intrinsic structures within the foot, from the spring ligament to the plantar fascia.
There is a significant risk of complications in diabetic foot and ankle reconstructive surgery [5]. There is a fivefold increase in post-operative infection risk in diabetic patients versus non-diabetic patients in foot and ankle surgery [6]. Based on review of the relevant literature, reducing the contracture of the Achilles’ tendon that was the pathophysiological basis for the diabetic foot ulcer and osteomyelitis reduces the risk of recurrence and improves the functional outcome of the transmetatarsal amputation [7].
Achilles’ Tendon Structure, Function and Examination
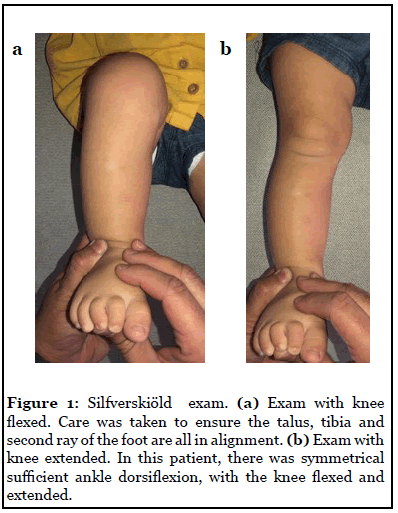
Anatomically, the Achilles’ tendon is formed from the conjoining of aponeurotic fibers from both the gastrocnemius and the soleus muscles [8]. The gastrocnemius originates proximal to the knee joint at the posterior femur, whereas the soleus originates distally to the knee joint at the proximal tibia and fibula [9]. Classically, the Silfverskiöld test is an exam utilized to differentiate the contribution from each muscle toward the clinically observed ankle equinus contractures [10]. The patient is placed in a supine or seated position. The surgeon then manipulates the foot to observe the position of the talar head at maximum foot pronation and maximum supination. During pronation, the talar head should be more prominent medially, as the talo-navicular joint becomes less congruous. During supination the talar head will be lateral to the midline of the foot. The palpability of the talar head as the foot moves from pronation to supination corresponds with the movement of the subtalar joint during the gait cycle. The surgeon will then manipulate the foot so there is equal absence of a palpable talar head, i.e. when the talus is the most congruous at the talonavicular joint. This position is considered to be the “neutral position” of the talus during the gait cycle11. The surgeon should note the midline of the foot, the second metatarsal ray, is typically now in line with the talus and the anterior tibial crest. The foot is then dorsiflexed at the level of the ankle joint to its maximum range of motion, first with the knee extended and then with the knee flexed. Figure 1 demonstrates proper technique in performing the Silfverskiöld test, with emphasis on using two hands.
During knee flexion, the gastrocnemius reduces its influence on the pull of the Achilles’ tendon. During knee extension, both the gastrocnemius and soleus affect the tension of the Achilles’ tendon. Therefore, a patient is considered to have a gastrocnemius-dominant ankle equinus contracture with increased neutral position ankle dorsiflexion during knee flexion and soleus-dominant ankle equinus with decreased neutral ankle dorsiflexion with knee flexion. If there is reduced capacity for ankle dorsiflexion range of motion with the knee both extended and flexed, the patient is diagnosed with combined gastrocnemius-soleus equinus. The purpose of this exam is to differentiate to the surgeon whether or not an isolated gastrocnemius surgery is sufficient to address the patient’s ankle equinus, or to utilize a procedure that affects the combined contribution from both muscles. There is debate in the literature as to the actual numerical value in degrees of dorsiflexion beyond the foot perpendicular to the long axis of the tibia [3].
The limitation of ankle dorsiflexion caused by ankle equinus results in triplanar deformity. In the sagittal plane, the talus becomes more plantarflexed. In the transverse plane, the metatarsals become more abducted. In the frontal plane, the calcaneus becomes more everted. In patients with adult-onset flexible flatfoot deformities, the medial longitudinal arch collapses and the resultant position abnormalities are all related to the effect of prolonged contracture in the Achilles’ tendon [12].
The diabetic foot patient often presents with osteomyelitis of the first proximal phalanx and often the pathophysiology originates from ankle equinus. In the majority of diabetic first proximal phalanx plantar ulcers, there is an underlying hallux valgus deformity. The international working group on the diabetic foot (IWGDF) recommends in their consensus documents removal of the base of the proximal phalanx for these patients [13]. This technique originally was written by Keller and was used for the treatment of hallux valgus, a traditionally non-diabetes related condition [14]. The cause of the hallux valgus was increased adduction of the first metatarsal at the level of the metatarsal-cuneiform joint. The adduction was promoted by strengthening the pull strength of the tibialis anterior muscle relative to the peroneus longus muscle, as they both insert into the foot at the plantar aspect of the metatarsal-cuneiform joint. The advantage of the tibialis anterior was caused in this setting by an increase in the tendon tension via reduction in the medial longitudinal arch height during weightbearing [15]. The reduced medial arch height is caused by increased plantarflexion of the talus as well as the eversion of the calcaneus. To reduce the risk of recurrence of forefoot ulcers in these patients, therefore, the precipitating pathophysiological factor of the Achilles’ tendon equinus contracture must be addressed [16]. If not, then the continued pull of the Achilles’ tendon will promote progression of the hallux valgus deformity that caused the ulcer.
Ankle Equinus in Foot and Ankle Trauma
The Achilles’ tendon is the chief deforming force in the foot through its ability to forcibly plantarflex the foot during inappropriate moments in the gait cycle. It can also promote forced plantarflexion during trauma cases as well. The Achilles’ tendon vector of force begins at its insertion in the retrocalcaneal area. The pulling action of the tendon forces the calcaneus to plantarflex as well as the talus to adduct, plantarflex and evert via compensation at the subtalar joint [17]. The malposition of the calcaneus and the talus will cause multiple comorbidities in trauma cases [18].
Pilon fractures are high injury traumatic injuries resulting from the talus being driven into the tibia by ground reactive forces. The goal of surgical reduction of the tibial pilon fracture is to bring any associated fibula shortening to length, restoring the epiphyseal fragments of the distal tibia and restore continuity between the tibia diaphysis, metaphysis and epiphysis [19]. As this is a high-energy event, the risk of post-traumatic osteoarthritis of the ankle joint is high [20]. Lengthening procedures that allow for increased ankle joint range of motion can reduce the risk of post-traumatic arthritis and increase the likelihood of success with treatment via ankle arthrodesis [21].
Addressing the Achilles Tendon with use of Transmetatarsal Amputation
History of previous lower extremity amputation is one of the strongest risk factors for progression to belowknee amputation [22]. Therefore, consideration towards improving the outcomes of transmetatarsal amputations are essential to prevent this outcome. Non-surgical approaches with accommodative shoe gear that reduces forefoot stress and strain can reduce post-transmetatarsal amputation risk of progress to below-knee amputation.
The utilization of percutaneous Achilles’ tendon lengthening as an adjunct procedure to transmetatarsal amputation reduces the risk of re-ulceration to the forefoot [23]. By reducing forefoot pressure through decreased Achilles’ tendon action, surgeons can reduce the initial pathophysiological mechanism of injury that precluded the transmetatarsal amputation to address a diabetic forefoot wound [7]. Figure 2 demonstrates a clinical exam utilizing percutaneous Achilles’ tendon lengthening to address a forefoot ulcer recurrence following a transmetatarsal amputation.

Surgical Approaches to Equinus
Many different surgical approaches for correction of equinus deformity have been described. In a broadview, there are two procedures to address the posterior musculotendinous complex: gastrocnemius recession and Achilles’ tendon lengthening. These operative releases improve contracture based on degree and etiology of the equinus deformity. These procedures often are categorized into anatomic approaches of the triceps surae tendoachilles complex and have been further described in open, endoscopic, and percutaneous techniques. Appropriate selection of procedure requires thorough physical examination of the patient to elucidate the underlying etiology and degree of deformity, as well as evaluation of patient profile. The influence of the gastrocnemius-soleus complex is determined with use of the Silfverskiöld test to differentiate the presence of isolated gastrocnemius contracture.
Gastrocnemius recessions have been described in various anatomic regions of the posterior calf. They commonly share a goal with release of the gastrocnemius tendon to functionally improve or restore normal length allowing for dorsiflexion of the ankle with the knee extended. The proximal most procedure includes fasciotomy of the medial head of the gastrocnemius muscle, awareness of muscular innervation should be considered in this procedure. The intramuscular lengthening of the gastrocnemius muscle in the proximal portion of the calf is performed through a medial approach between the soleus and gastrocnemius muscles which truly isolates the lengthening of the gastrocnemius muscle only (Baumann procedure), care should be taken to avoid the saphenous vein. A superficial gastrocnemius-soleus recession including intramuscular lengthening of the soleus has also been described. This includes a chevron inverted V cut (Vulpius procedure) or tongue-in-groove U cut (Baker procedure) into the conjoined tendon with the groove portion located proximally. The distal gastrocnemius tenotomy performed approximately 3 cm proximal to the gastrocnemius-soleus aponeurosis has been described, where the plane between the gastrocnemius and soleus have been separated, followed by transverse sectioning of the gastrocnemius aponeurosis allowing for the gastrocnemius tendon to retract proximally and then sutured to the soleus muscle and intact fascia (Strayer procedure) [24].
Open release of just the aponeurosis of the gastrocnemius muscle which avoids the tendon has also been described [25]. The complication rates vary depending on study: open gastrocnemius recession have been reported to range from 0-38%, and endoscopic gastrocnemius recession have been reported from 0-12.7% [26]. Open gastrocnemius recessions are known to often report higher incidence of infection, dehiscence, neurovascular compromise and cosmetic outcome leading to patient dissatisfaction. A new and promising minimally invasive approach has been described that utilizes ultrasound guidance, eliminating many potential complications, only reporting incidence of hematoma/seroma [27].
Authors Preferred Surgical Approach: The Modified Percutaneous Triple Hoke Hemi-section of the Achilles’ Tendon
The authors’ preferred method is a modified percutaneous triple Hoke hemi-section of the Achilles’ tendon. This method has the benefits of decreased intraoperative time, relative ease of procedure, minimization of complications, reduced patient recovery time, and high effectiveness on biomechanical influence and resultant pathologies.
Studies have demonstrated that the percutaneous triple Hoke hemi-section when compared with traditional open Z lengthening approach has approximately onethird of intraoperative time, fewer complications, and no statistically significant differences in therapeutic effect versus open techniques [28]. This method helps to maintain muscle strength and preserve function relative to traditional open Achilles’ tendon lengthening procedures and minimizes risk of over lengthening. The percutaneous minimally invasive approach is less traumatic and ideal in the populations of diabetics who are susceptible to infections and those with underlying components of peripheral arterial disease.
Surgical criterion must be considered and met, as with any other surgical procedure inappropriate selection of procedure can lead to less than ideal results. The patient is placed on the operative room table with placement of a well-padded pneumatic thigh tourniquet. The patient is then placed in a prone or modified rolled lateral hip (frog leg) position to maximize surgical view of posterior leg, ankle, and foot positioning. Next, topographic anatomic landmarks are drawn including the medial and lateral border and insertion in the calcaneus. Utilizing aseptic technique, the lower extremity is scrubbed, prepared and draped. Next, the decision for placement of initial hemi-section of tendon at insertion of tendon must be considered. Calcaneal positioning must be considered as the biomechanical influence can be exaggerated as a result. If the heel is in varus positioning and further correction of this deformity is not being addressed with additional surgical correction, the first and third cuts are placed on the medial side. When in valgus positioning, the first and third cuts are placed on the lateral sides. The procedure consists of three alternating hemi-incisions (through one half of the tendon), the distal most is made approximately 2.5 cm from the calcaneal insertion, traversing from the center of the tendon to its border. Care is taken to deepen the blade through the tendinous layer only, avoiding surrounding neurovascular and tendon. Adequate sectioning of the tendon is evaluated both visually and manually. The proximal most incision is made just below the musculotendinous junction in the same direction as first. The last hemi-section incision is approximated between the prior incisions and is directed in an alternate manner from center to border. The effect of hemi-section release on ankle dorsiflexion is evaluated intraoperatively with each cut. If optimal dorsiflexion is not obtained, conversion to an open procedure should be considered. The surgical sites are copiously irrigated with normal saline solution. This site may be left open and allow for granulation to occur, however it is the author’s preference to primarily close the cutaneous layer with a non-reactive suture. Dry sterile dressing is then applied, and the patient should be immobilized postoperatively, held in a neutral position with either a splinting or CAM walker boot for a three to four period with an aim for early weightbearing.
Possible Complications in Surgically Addressing Ankle Equinus
Caution must be used to protect and avoid inadvertent injury to surrounding neurovascular structures in all procedures addressing ankle equinus deformity. The sural nerve is a sensory nerve that is formed by the terminal branches of the common fibular and tibial nerves. This structure merits extra precaution due to high anatomic variation as this may be located either deep or superficial to the fascia of the calves, 57.5% and 42.5% respectively [29]. If the result of the Silfverskiöld test reveals Achilles’ tendon tightness, a radiograph should be considered to eliminate possibility of bony block and pseudoequinus. Once these possibilities are ruled out, further consideration of Achilles’ tendon lengthening is recommended. Overcorrection and under-correction may lead to undesired biomechanical influence and poor outcome, and therefore should be avoided. Intraoperative evaluation is imperative for ideal outcome.
Conclusion
The influence of ankle equinus should be considered when evaluating foot deformities or plantar ulcerations. Routine screenings for ankle equinus should be performed on physical examination with focus to identify underlying etiology and degree of deformity. Early provisional treatment including conservative methods (including strengthening and stretching exercises) as well as surgical intervention may help prevent worsening symptomatic pathologies.
Addressing equinus by means of lengthening on the gastrocnemius-soleus-Achilles’ tendon complex in a patient with ankle equinus has influence on biomechanical and pathologic factors and is essential for optimal outcome with complex foot deformities and diabetic foot ulcerations. Complications of these procedures include pain with range of motion, weakness of flexors/ toe off, difficulty utilizing stairs, incision complications, recurrence of equinus deformity and rarely, rupture of the Achilles’ tendon.
Universal standardization in defining the pathologic condition of ankle equinus as well as standardization of measurement methods may perhaps better elucidate prevalence and provide a consensus in understanding of this condition. Variations may be present in use of goniometer relative to anatomic landmarks and amount of torque applied to obtain measurements, which currently may differ from physicians. This is relevant to both the clinical and surgical setting. It has been reported that most reports of the ankle equinus are observational and anecdotal [30].
More research is needed to reveal further potential benefits of surgically addressing ankle equinus. Our review of literature elucidated that more high-level studies are needed. Future well designed research studies with large participants may provide insight into efficacy and potential preventative benefits of these procedures.
References
2. Ramanujam CL, Zgonis T. Surgical correction of the achilles tendon for diabetic foot ulcerations and Charcot neuroarthropathy. Clinics in Podiatric Medicine and Surgery. 2017 Apr 1;34(2):275-80.
3. Baumbach SF, Braunstein M, Seeliger F, Borgmann L, Böcker W, Polzer H. Ankle dorsiflexion: what is normal? Development of a decision pathway for diagnosing impaired ankle dorsiflexion and M. gastrocnemius tightness. Archives of Orthopaedic and Trauma Surgery. 2016 Sep 1;136(9):1203-11.
4. Wezenbeek E, Willems TM, Mahieu N, Van Caekenberghe I, Witvrouw E, De Clercq D. Is Achilles tendon blood flow related to foot pronation?. Scandinavian Journal of Medicine & Science in Sports. 2017 Dec;27(12):1970-7.
5. Zou RH, Wukich DK. Outcomes of foot and ankle surgery in diabetic patients who have undergone solid organ transplantation. The Journal of Foot and Ankle Surgery. 2015 Jul 1;54(4):577-81.
6. Wukich DK, Lowery NJ, McMillen RL, Frykberg RG. Postoperative infection rates in foot and ankle surgery: a comparison of patients with and without diabetes mellitus.The Journal of Bone and Joint Surgery. 2010 Feb 1;92(2):287-95.
7. Blume P, Salonga C, Garbalosa J, Pierre-Paul D, Key J, Gahtan V, Sumpio BE. Predictors for the healing of transmetatarsal amputations: retrospective study of 91 amputations. Vascular. 2007 Jun 1;15(3):126-33..
8. Doral MN, Alam M, Bozkurt M, Turhan E, Atay OA, Dönmez G, Maffulli N. Functional anatomy of the Achilles tendon. Knee Surgery, Sports Traumatology, Arthroscopy. 2010 May 1;18(5):638-43.
9. Pierre-Jerome C, Moncayo V, Terk MR. MRI of the Achilles tendon: a comprehensive review of the anatomy, biomechanics, and imaging of overuse tendinopathies. Acta Radiologica. 2010 May;51(4):438-54.
10. Young CC, Niedfeldt MW, Morris GA, Eerkes KJ. Clinical examination of the foot and ankle. Primary Care: Clinics in Office Practice. 2005 Mar 1;32(1):105-32.
11. Lee WCC, Lee CKL, Leung AKL, Hutchins SW. Is it important to position foot in subtalar joint neutral position during non weightbearing molding for foot orthoses? Journal of Rehabilitation Research and Development. 2012;49(3):459.
12. Anselmo DS, Thatcher L, Erfle D. Gastrocnemius Recession as an Alternative to Midfoot Arthrodesis for Painful Midfoot Arthritis. The Journal of Foot and Ankle Surgery. 2020 May 30.
13. Armstrong DG, Lavery LA, Vazquez JR, Short B, Kimbriel HR, Nixon BP, Boulton AJ. Clinical efficacy of the first metatarsophalangeal joint arthroplasty as a curative procedure for hallux interphalangeal joint wounds in patients with diabetes. Diabetes Care. 2003 Dec 1;26(12):3284-7.
14. Finestone AS, Tamir E, Ron G, Wiser I, Agar G. Surgical offloading procedures for diabetic foot ulcers compared to best non-surgical treatment: a study protocol for a randomized controlled trial. Journal of Foot and Ankle Research. 2018 Dec 1;11(1):6.
15. Johnson CH, Christensen JC. Biomechanics of the first ray part V: The effect of equinus deformity: A 3-dimensional kinematic study on a cadaver model. The Journal of Foot and Ankle Surgery. 2005 Mar 1;44(2):114- 20.
16. Colen LB, Kim CJ, Grant WP, Yeh JT, Hind B. Achilles tendon lengthening: friend or foe in the diabetic foot?. Plastic and reconstructive surgery. 2013 Jan 1;131(1):37e-43e.
17. Sangeorzan A, Sangeorzan B. Subtalar Joint Biomechanics: From Normal to Pathologic. Foot and Ankle Clinics. 2018 Jul 3;23(3):341-52.
18. Benirschke SK, Kramer PA. Gastrocnemius or Achilles Lengthening at Time of Trauma Fixation. Foot and ankle clinics. 2017 Mar 1;22(1):117-24.
19. Dujardin F, Abdulmutalib H, Tobenas AC. Total fractures of the tibial pilon. Orthopaedics & Traumatology: Surgery & Research. 2014 Feb 1;100(1):S65-74.
20. Beaman DN, Gellman R. Fracture reduction and primary ankle arthrodesis: a reliable approach for severely comminuted tibial pilon fracture. Clinical Orthopaedics and Related Research®. 2014 Dec 1;472(12):3823-34.
21. Li Y, He J, Hu Y. Comparison of the Efficiency and Safety of Total Ankle Replacement and Ankle Arthrodesis in the Treatment of Osteoarthritis: An Updated Systematic Review and Meta-analysis. Orthopaedic Surgery. 2020 Apr;12(2):372-7.
22. Pemayun TG, Naibaho RM, Novitasari D, Amin N, Minuljo TT. Risk factors for lower extremity amputation in patients with diabetic foot ulcers: a hospital-based case–control study. Diabetic Foot & Ankle. 2015 Jan 1;6(1):29629.
23. Pollard J, Hamilton GA, Rush SM, Ford LA. Mortality and morbidity after transmetatarsal amputation: retrospective review of 101 cases. The Journal of Foot and Ankle Surgery. 2006 Mar 1;45(2):91-7.
24. Firth GB, McMullan M, Chin T, Ma F, Selber P, Eizenberg N, Wolfe R, Graham HK. Lengthening of the gastrocnemius-soleus complex: an anatomical and biomechanical study in human cadavers.The Journal of Bone and Joint Surgery. 2013 Aug 21;95(16):1489-96.
25. Tellisi N, Elliott AJ. Gastrocnemius apneourosis recession: a modified technique. Foot & Ankle International. 2008 Dec;29(12):1232-4.
26. Harris III RC, Strannigan KL, Piraino J. Comparison of the complication incidence in open versus endoscopic gastrocnemius recession: a retrospective medical record review. The Journal of Foot and Ankle Surgery. 2018 Jul 1;57(4):747-52.
27. Villanueva M, Iborra Á, Rodríguez G, Sanz-Ruiz P. Ultrasound-guided gastrocnemius recession: a new ultra–minimally invasive surgical technique. BMC musculoskeletal disorders. 2016 Dec;17(1):1-9.
28. Lin Y, Cao J, Zhang C, Yang L, Duan X. Modified Percutaneous Achilles Tendon Lengthening by Triple Hemisection for Achilles Tendon Contracture. BioMed Research International. 2019 Nov 7;2019.
29. Anderson JG, Bohay DR, Eller EB, Witt BL. Gastrocnemius recession. Foot and Ankle Clinics. 2014 Dec 1;19(4):767-86.
30. DiGiovanni CW, Langer P. The role of isolated gastrocnemius and combined Achilles contractures in the flatfoot. Foot and Ankle Clinics. 2007 Jun 1;12(2):363-79.
