Abstract
Introduction: The term Proprioceptive Neuromuscular Facilitation (PNF) was introduced in the 1950s by Dr. Kabat and Mrs. Knott. From the mid-1950s the PNF-concept has been in a progressive development clarifying the use of techniques, performances and clinical applications. The concept of PNF was originally developed by Dr. Kabat and Mrs. Knott for rehabilitation purposes. The International PNF Association (IPNFA) consider themselves to be the official successor of Dr. Kabat and Mrs. Knott.
The PNF-concept evolved towards a comprehensive rehabilitation approach for various indications. There seems to be a misunderstanding about the PNF-concept, it is often seen as a basic stretching regime for wellbeing and general fitness. This has been criticized to avoid a confusion with the PNF-concept as a comprehensive rehabilitation approach.
Purpose: Providing a background with an explanation for the essential elements of the PNF-concept, being a total and comprehensive rehabilitation approach in physiotherapy and rehabilitation. The elements from the PNF-concept facilitate treatment effects in the fields of musculoskeletal and central neurological disorders and indications with a focus on motor learning.
Implications: The clarification of the essential elements from the PNF-concept in various fields of physiotherapy and physical rehabilitation will simplify how to transfer and incorporate the elements from the PNF-concept into individual treatments.
Keywords
PNF, Rehabilitation, Motor learning and motor control, Proprioception, Facilitation, Musculoskeletal, Neurology, Clinical Reasoning
Introduction
The term Proprioceptive Neuromuscular Facilitation (PNF) was introduced in the 1950s after it was first named proprioceptive facilitation by Dr. Kabat and Mrs. Knott [1-3]. The concept of PNF was originally developed by Dr. Kabat and Mrs. Knott for rehabilitation purposes [2]. The works of Dr. Kabat and Mrs. Knott was encouraged by the Kaiser institute in the 1940s [2]. The International PNF Association (IPNFA) consider themselves to be the official successor of Dr. Kabat and Mrs. Knott [4].
From the mid-1950s until today the PNF-concept has been in a progressive development for the use and explanation of techniques, performances and clinical applications [3,5]. From the early start the theories from Sir Charles Sherrington [6,7] have been the rational for facilitation. In the decades following, the theories of motor learning and task specific exercise and training [8,9] have been integrated into the total concept. The PNF-concept evolved towards a comprehensive rehabilitation approach for a variety and diversity of indications [5,10].
Although the PNF-concept is part of the physiotherapy curriculum in many countries [5,10], somehow there seems to be a misunderstanding about the PNF-concept. PNF is often seen as a basic stretching regime for wellbeing and general fitness. This misunderstanding transferred into its own life in modern social media and in research, expressed in sports related studies, such as for example from Bradley et al. [11] and YouTube videos [12].
Even, reviews in the field of PNF have mainly focused on so called ‘PNF stretching’ [13-15]. This has been criticized, since the result is often a confusion with the overall PNF-concept as a comprehensive rehabilitation approach [5].
This narrative provides an educational background, explaining the essential elements of the PNF-concept being a total and comprehensive rehabilitation approach in physiotherapy and rehabilitation in the field of musculoskeletal and central neurological disorders and indications [4,5].
In order to substantiate this educational narrative, a literature search has been executed between December 2021 and June 2022. The databases PubMed, CINAHL, Science Direct and Google Scholar have been used, also the IPNFA website was searched. The search terms included: Proprioceptive Neuromuscular Facilitation, PNF, facilitation techniques, treatment techniques, exercise methods, exercise concepts, treatment methods, treatment concepts, rehabilitation approaches and motor learning. Search terms were used isolated and combined. A standard screening procedure was secured since the author is familiar with the PNF-concept in its therapeutic application and in teaching being a member of the IPNFA. Secondly, the results have been discussed with fellow IPNFA members (although not opting for co-authoring) for eligibility. Similar to the used process in the narrative review from Smedes et al [5], papers were included after screening the title and the abstract upon the following criteria: a) PNF as a concept was a part of the publication. b) Techniques from the PNF-concept were a part of the publication. c) PNF-concept or PNF techniques were a part of the treatments for a specific indication or patient population. d) Facilitation similar to the described PNF basic principles and procedures was a part of the publication. As the literature identified in the search (50 sources) comprised varying levels of evidence (case studies, clinical trials, randomized controlled trials, reviews) and investigated a broad range of PNF applications, quantitative or qualitative systematic review was not feasible. The variety in type of papers and the diversity of the scope of the papers found with the literature search, warranted a narrative type of presentation.
Therefore, first the PNF-concept and its elements are presented and explained. Thereafter, the use of the PNF-concept in various clinical settings is illustrated. Settings such as: rehabilitation focusing on motor learning, rehabilitation in musculoskeletal conditions, in neurological conditions, for vital function conditions and rehabilitation for gait improvement.
Three Main Pillars of the Concept
PNF is defined as a concept and not as a method [3,4], the difference between method and concept has been defined; a method is more rigid and defined as going through pre-defined steps, describing a particular way of “doing” the performance [16], whereas a concept is open to personal adjustments within the framework of the general idea, retained in the mind and based upon reasoning [17].
The PNF-concept is built upon three main pillars: 1) the PNF-philosophy, 2) the PNF-basic principles & procedures (for facilitation) and 3) the PNF-techniques (for treatment) [3,5].
PNF-philosophy
The PNF-philosophy is defined by five components: a) Positive Approach, meaning to set up the patient for success; b) Functional Approach, meaning that all exercises are in connection with a functional task setting; c) Mobilization of Reserves, aiming for a stronger involvement of the targeted body area through the use of stronger body parts; d) Treat the total human being, physically , mentally and emotionally, and e) The use of motor control and motor learning principles [3-5].
The PNF-concept in rehabilitation is meant to teach: movement, contraction and skill, to the patient. Hence, the patient needs to acquire control over external forces and resistances such as gravity and friction. Gravity acting on our own body and body parts but also to materials and objects that we handle. Friction occurs when handling materials and moving ourselves within the mechanical environment. Hence, to learn to control these external forces, patients need to go through a process of motor learning, as in the re-acquisition of previously learned actions in the presence of altered morphology, be it sensory, motor or cognitive impairments [9,18].
PNF-basic principles & procedures
To be able to learn as a patient, we need to provide enhancing circumstances or facilities [18]. Within the PNF-concept this translates into facilitation provided by giving exteroceptive and proprioceptive input to the sensory system in a procedural way, all together the PNF-basic principles & procedures (BPP) (Table 1).
|
Exteroceptive principles of stimuli |
Proprioceptive principles of stimuli |
Procedural stimuli. |
|
Tactile (Lumbrical grip) Verbal or auditive Visual |
Optimal resistance Approximation Traction Elongation Irradiation & reinforcement |
Pattern Timing + Timing for Emphasis Body mechanics Summation |
Most known among (young) physiotherapist, seems to be the PNF-patterns. PNF-patterns mimic movements from sports and activities of daily living (ADL) [3,19,20]. Patterns are however only one of twelve BPP. A pattern (of muscle activation rather than a pattern of movement) is only a procedure in which the proprioceptive stimuli, such as elongation, resistance, approximation and irradiation are delivered while at the same time exteroceptive information is given, e.g. tactile, verbal and /or visual [3,5]. To be able to provide resistance (one of the key features to teach contraction and movement) a tactile stimulus with a specified “lumbrical grip” is necessary [3] (Figure 1). The resistance is given not only by the therapist hands, but rather by the therapist’s position in relation to the patient and his way of moving with the desired pattern of activation defined as “body mechanics” [3,5], and in such a way that the order of muscle activation and the order of movements is addressed towards the patient for the specific task at hand, resulting in a defined “timing” [3,5]. The tactile stimulus can also be delivered in the line of the bones and joints of the extremity. This type of stimulus results in either an approximation (an axial compression through the joints) similar as in weight bearing activities or a traction which is defined as the elongation of a segment perpendicular to the highest point of the arc of the motion [3,5,21] (Figure 2).
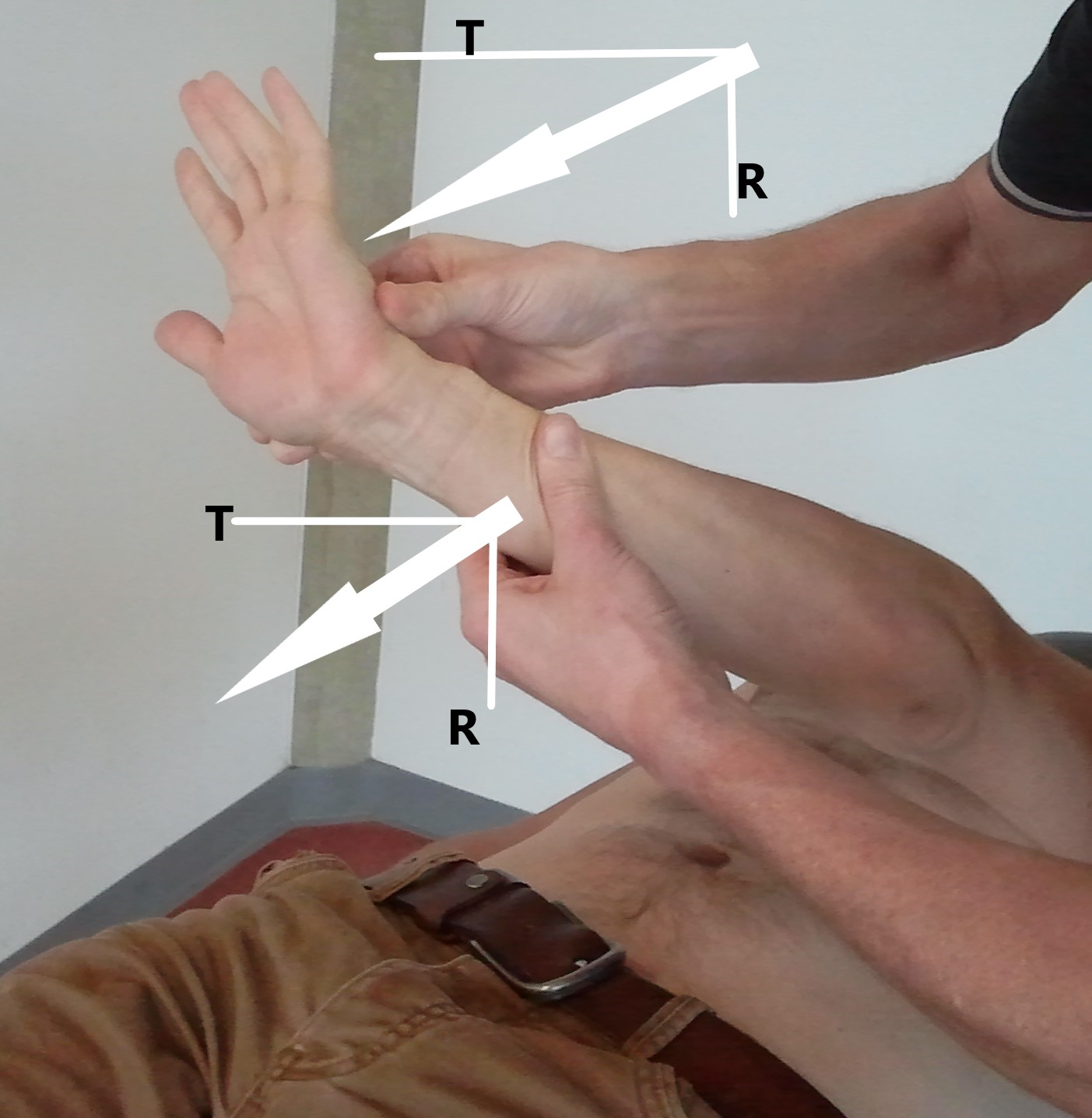
Figure 1. Lumbrical grips. Note the lumbrical hand position in both therapist-hands. Arrows indicating resistance (R) and traction (T).

Figure 2. Facilitation principles. Note the axial approximation through the spine. Note the resistance against the bilateral arm patterns, left arm: flexion/abduction/external rotation and right arm: flexion/adduction/external rotation, together leading into trunk: extension/left torsion.
Synchronized with the tactile stimuli also verbal and / or visual stimuli should be provided [3,5]. In this way several stimuli together result in a “summation of stimuli” [3]. “Timing” defined as being the order of (visible) movements during a task might be adjusted to focus on the disturbing impairment within a pattern of movement. Therefore, emphasizing the exercises within the pattern of activation towards the weaker or minimized component resulting in a “timing for emphasis” [3,5]. In this way the stronger parts might influence the recruitment for the weaker components, since resisted pattern activity results in activation of synergistic muscles, referred to as “irradiation” [3,5,6,7,22].
Connecting the philosophy with the BPP could be seen in analyzing daily activities such as pulling a zipper to close a jacket, or cutting vegetables in a kitchen. To close a zipper, one hand needs to pull and is active in the pattern flexion / abduction / external rotation with elbow flexion while the other hand holds down the socket and the whole arm will be active in a pattern of extension / abduction / internal rotation with elbow extension and ulnar deviation of the wrist (Figure 3). This is an example of “controlled mobility” [23] defined by a mobile part, overcoming the resistance from gravity and friction from the zipper while having a stabilization at the other side, holding steady the socket.

Figure 3. Closing a zipper. 1: indicating the activity in the (left) arm pattern D2 for flexion / abduction / external rotation with elbow flexion. 2: indicating the activity in the (right) arm pattern D1 for extension / abduction / internal rotation with elbow extension.
In cutting vegetables one hand holds down the vegetable with a muscle activation pattern of extension / adduction / internal rotation with elbow extension while the cutting hand controls the knife with an extension / abduction / internal rotation with elbow extension overcoming the friction from the act of cutting (Figure 4).

Figure 4. Cutting vegetables. 1: indicating the activity in the (left) arm pattern D2 for extension / adduction / internal rotation with elbow extension. 2: indicating the activity in the (right) arm pattern D1 for extension / abduction / internal rotation with elbow extension.
One can analyze in a similar way the bilateral activities from the lower extremities while getting on a bicycle or stepping into a bath tub. The swing leg needs to lift against gravity with a flexion / abduction / internal rotation with knee flexion to avoid kicking into the rear wheel, while the other leg needs to stabilize the bodyweight against gravity with an extension/ abduction/ internal rotation activation (Figure 5).

Figure 5. Getting on a bicycle. Note the large arrow indicating activity in the right leg pattern D2 for flexion / abduction / internal rotation with knee flexion. Note the small arrow indicating the foot active in dorsal flexion and eversion.
PNF-techniques
Ten different PNF-techniques have been developed and defined in the course of the development of the concept in the decades of the last century. Earlier publication might use older names which have been adjusted based upon consensus among the IPNFA-members [4]. The IPNFA defined the following three groups of techniques:
A) Agonistic techniques; characterized by contractions and movements in the targeted direction and muscle groups, which are: 1: Rhythmic Initiation, to provide a learning moment to the patient for the movement; 2: Replication, to provide a learning of position as a result of a movement; 3: Combination of Isotonics, providing learning of the coordination of muscle contraction, concentrically, statically and eccentrically; 4: Stretch at the beginning of range of motion (ROM), to learn the onset of contraction and movement (recruitment); 5: Stretch through ROM, to learn, to acquire and to train muscle contractions through the full range of movement [3,5].
B) Antagonistic techniques; characterized by alternating contractions or co-contractions of the agonists and antagonists, which are 1: Dynamic Reversals, to learn the alternation of contraction between agonists and antagonists to move actively through the ROM in both directions; 2: Stabilizing Reversals, to learn to alternate contractions between agonists and antagonists with the aim to maintain in a position; 3: Rhythmic stabilization, to learn to build a co-contraction with the agonists and antagonists to hold a position [3,5].
C) Relax techniques; characterized by a voluntary contraction and a voluntary relaxation to increase the ROM and flexibility of muscle(groups), which are 1: Hold Relax, to increase the ROM of the targeted muscles after a static contraction; 2: Contract Relax, to increase the ROM and flexibility of the targeted muscles after a small dynamic contraction [3,5] (Table 2).
|
Agonistic techniques |
Objective |
Antagonistic techniques |
Objective |
Relax techniques |
Objective |
|
Rhythmic Initiation |
Motor learning |
Dynamic Reversals |
Strength + Endurance + Tone regulation/ Intermuscular coordination |
Hold Relax |
Range of motion + Pain relieve + Tone regulation |
|
Replication |
Motor control |
Stabilizing Reversals |
Strength + Stability + Intermuscular coordination |
Contract relax |
Range of motion + Tone regulation |
|
Combination of Isotonics |
Strength + Endurance + Intramuscular coordination |
Rhythmic stabilization |
Stability + Intermuscular coordination |
|
|
|
Stretch at the beginning of range of motion |
Recruitment |
|
|
|
|
|
Stretch through range of motion |
Recruitment + Strength |
|
|
|
|
|
+ = improve or increase of the forementioned issue. |
|||||
The PNF-techniques are chosen to address a specific impairment that disturbs the execution of a functional activity or task. The choice of technique is depending on the coordination of muscle activation in functional use, hence an analysis of the task and the involved muscle coordination is required [5].
For example, comparing reaching and placing a book on a shelf versus reaching and pulling a rope to open a sunscreen reveals that the first ADL-task requires the agonistic muscles to lift the arm against gravity. Therefore, a concentric contraction is needed and when lowering the arm, the same agonists need to work eccentrically because of the weight of the arm and the lifted item [24]. For the second ADL-task the same agonists need to lift the arm towards the rope and then when pulling the rope starts, the antagonists need to work in a concentric contraction to pull against the weight of the sunscreen and the friction of the system [24]. Neuromuscular control of reaching requires the synchronization of muscle activation at all the moving joints as well as all the muscles involved in postural stabilization [25]. For these two activities there is clearly a different inter- and intramuscular coordination required. This can be addressed with specific PNF-techniques, the first task with “Combination of Isotonics” the second task with “Dynamic Reversals” (reversal of antagonist) [3,5,26].
The PNF-Concept in Clinical Context
PNF in relation to motor learning
Voss et al. [26] defined PNF as ‘methods of promoting or hastening the response of the neuromuscular mechanism through stimulation of the proprioceptors’. A lasting response of the neuromuscular mechanism is considered to be a motor learning effect [9,18], which is the key component of the PNF philosophy [3,5]. The methods of promoting or hastening the response are defined within the PNF-concept as the PNF basic principles and procedures and PNF techniques [3,26]. Therefore, a conscious and deliberate use of the components from the pillars of the PNF-concept to achieve a motor learning effect can be the start for clinical decision making, once objectives for the treatment have been defined. Edwards et al. [27] stated: “learning of movement and its therapeutic application with patients through teaching is arguably the most central role of physiotherapists”.
The results from several studies provide support to various components from the PNF-concept. Initiation of voluntary movements seems to be enhanced by the three-dimensional patterns of movement as defined in the PNF-concept, resulting in a shorter reaction time for the muscle to be activated and a more efficient movement of the joints compared to neutral positions [28]. According to Moreira et al. [29], PNF-pattern movements generate a greater cortical activity, measured by the absolute power levels in the beta band in the parietal cortex, important for the integration of motor information. Furthermore, in PNF-pattern movements, electrophysiological changes result in an increase of alpha absolute power in the dorsolateral prefrontal cortex and superior parietal cortex [30]. The above-mentioned cortical effects are of interest for motor learning objectives. Nevertheless, motor learning effects are depending on real life tasks in real life environment [8]. Hence, to overcome issues of weakness, tightness and learned non-use, clients need rehabilitation to be effective in optimizing neural reorganization and functional recovery. To promote and achieve motor learning a challenging, engaging and meaningful task training needs to be emphasized [31-33]. Modern PNF has integrated these functional task-oriented environment situations [3,5]. With the task-oriented use of muscle pattern activation, the patient is guided to shift the focus of attention from internal (body oriented) to an external focus (directly related to the aim of the exercise). As muscle strength, motor control and skill increase, the learner’s focus of attention can shift more to external focus [34,35].
These motor learning effects are substantiated in several case reports and single case studies [36-41].
PNF in musculoskeletal rehabilitation
Effects from PNF on muscle strength, muscle size and muscle performance have been described; Kofotolis et al. [42] demonstrated an increase in muscle size after applying PNF resistance exercises. Gabriel et al. [43] explained the effects of resistive exercises and concluded that motor learning theory should be incorporated into strength-training practice. Furthermore, advise is given to use submaximal eccentric contractions when there are issues of muscle pain, detraining or limb immobilisation, and the use of DR techniques within PNF-pattern is advocated since this would be useful to increase the rate of muscletension development in older adults, for example important in preventing falls [43]. The benefits from the above-mentioned effects on muscle function and strength have been explored in specific contexts such as of patients with (chronic) low back pain (CLBP). Areeudomwong and Buttagat [44] demonstrated the effects from PNF based stabilization training in CLBP patients. Similar effects on pain and disability have been reported in CLBP patients after treatment with a specified PNF-based exercise program with explicit use of PNF techniques and facilitation principles [45,46]. Furthermore, three recent reviews have established the benefits from the PNF-Concept in the management of patients suffering from CLBP [47-49].
When analyzing mobilization techniques from manual therapy with those from PNF, it appears that the reasoning from skeletal arthrokinematics results in a similar exercise when reasoning from muscle activation [50,51]. For example, the lumbar mobilization starting in a side-lying position for “opening” the intervertebral foramen requires a side bending to one side and a contralateral rotation [52,53]. In the same starting position utilizing the scapula pattern “posterior elevation” together with the pelvis pattern “anterior depression”, the muscle activation from the client will result in a similar position of side bending to one side together with a contralateral rotation, and therefore actively opening the intervertebral foramen [50,51]. The later performance benefits from cortical involvement induced by the provided facilitations from resistance and irradiation [28,54]. This is consistent with the findings from de Zoete et al. [55] who concluded in their meta-analysis that spinal manipulations are similar effective as mobilizations and exercise therapy for CLBP, they recommend to combine these intervention techniques in a broader treatment package. Furthermore, PNF rehabilitation has shown to be effective when applied to various complaints in the spine, upper- and lower extremities. For example, Tedla and Sangadala [56] concluded in their meta-analysis, PNF to be superior to conventional physiotherapy for the treatment of adhesive capsulitis. Successful application of the PNF-concept was reported in adjusting the angle of the spine in scoliosis [57], and the treatment of non-specific neck complaints [58]. Also, the successful specific use of the PNF-concept has been described in a case of a total hip replacement while having complex pelvic malformations [41].
PNF in neurological rehabilitation
Functional task training as required in neurorehabilitation, is an integrated approach in the modern PNF-concept [3]. A detailed PNF approach has been proposed as an alternative to constraint induced movement therapy in case a patient is not responsive to this type of forced use to overcome their “learned non-use” behavior [38]. Nevertheless, there is still a lack of research on the effectiveness of the PNF-concept on hand function and dexterity. On the other hand, there is a substantial amount of research demonstrating positive outcomes on balance and gait in patients suffering from a stroke, upon a PNF based treatment. Gunning and Uszinsky [59] concluded in their systematic review that PNF is an effective treatment on gait parameters for patients after stroke. Specifically, effects on gait velocity, cadence and the outcomes on the Wisconsin Gait Scale are substantial and better then in weight supported treadmill training among stroke survivors [60]. Several studies indicate that gait effects can be achieved in patients after stroke by using the PNF pelvis patterns in various starting positions, such as side lying, sitting, stance and during actual gait [61-63]. Furthermore, PNF-based gait training has been shown effective in neurological conditions, such as in Huntington’s and Parkinson’s disease [64,65]. In Parkinson’s disease effects on spatiotemporal gait parameters, such as stride length and gait speed have been established [66].
PNF and vital functions
Pereira [67] concluded that PNF techniques can be safely applied, also to patients with limited cardiac function. Furthermore, beneficial effects on respiratory capacity after bypass surgery has been substantiated [68]. The PNF-concept is able to provide an increase in general fitness and minimizing fatigue in the condition of advanced cancer, as a result from its active comprehensive approach [69].
PNF in gait rehabilitation
Gait parameter, as an expression of activities and participation, is often an objective in rehabilitation common in musculoskeletal, neurological, and vital disease conditions. PNF-based gait training makes use of detailed patterns of muscle activation, since the PNF-patterns mimic functional movements as they appear in ADL and sports [20]. The leg pattern Extension/Abduction/Internal rotation with knee extension (and plantarflexion with eversion in foot and toes) provides the required forces for gait; meaning from the hip: extension for propulsion and abduction to ensure frontal stabilization, and to achieve the push off, an internal rotation in the hip with knee extension and plantarflexion with eversion into the big toe is necessary [3,70,71]. When the stance leg is active as just described, the contra lateral leg needs to be in swing phase, initiated with stabilization from the lower trunk [72]. This requires the frontal stabilization from the pelvis by a couple force provided by the hip abductors from the stance leg and the contra lateral oblique abdominals. This can be achieved with the combination of various patterns: stance-leg pattern in Extension/Abduction/Internal rotation and the contra-lateral pelvis in Anterior Elevation, while at the same time the contra-lateral arm is in Extension/Abduction/Internal rotation together with a scapula Posterior Depression [41].
Besides the use of PNF to improve gait in neurorehabilitation as described in the section “neurological rehabilitation”, PNF can be integrated in the treatment for various musculoskeletal conditions. The application of a specified PNF-program in amputation patients illustrated musculoskeletal effects besides motor learning effects [73-75]. Furthermore, PNF-based gait training has been shown effective after total knee arthroplasty [76]. The total comprehensive approach with a rational from biomechanical forces and integrated task oriented motor learning has been illustrated in a specific case of total hip arthroplasty while having several pelvic malformations [41].
Conclusion
In conclusion one can state that the PNF-concept allows to provide a physical therapy and / or rehabilitation intervention within the ICF categories. The PNF-basic principles and procedures (for facilitation) and the PNF-techniques address impairments from body structures and body functions as well as limited activities. Therapeutic objectives in both mentioned categories within the personal and environmental context can attribute to achieve a higher level of social participation. In short the PNF-concept enhances patients abilities from facilitation to participation.
Declaration of Interest
The author is involved in post graduate education (courses) for physiotherapists as a representative of the International PNF Association (IPNFA).
Funding
I confirm that this work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
2. Sandel ME. Dr. Herman Kabat: Neuroscience in Translation ... From Bench to Bedside. PM R. 2013;5:453-61.
3. Beckers D, Buck M. PNF in practice. 5th ed. Berlin: Springer; 2021.
4. International Proprioceptive Neuromuscular Facilitation Association [Internet]. [cited 2022 June 24]. Available from: http://www.ipnfa.org.
5. Smedes F, Heidmann M, Schäfer C, Fischer N, Stępień A. The proprioceptive neuromuscular facilitation-concept; the state of the evidence, a narrative review. Phys Ther Rev. 2016;21:17-31.
6. Sherrington CS. The integrative action of the nervous system. New Haven, (CT): Yale University Press; 1906.
7. Sherrington CS. The integrative action of the nervous system. New Haven, (CT): Yale University Press; 1947.
8. Carr JH, Rb Shepheard RB. The Changing Face of Neurological Rehabilitation. Rev Bras Fisioter. 2006;10:147-56.
9. Shumway-Cook A, Woollacott MH. Motor Control Translating research into clinical practice. 5th ed. Philadelphia (PA): Wolters Kluwer; 2017.
10. Westwater-Wood S, Adams N, Kerry R. The use of proprioceptive neuromuscular facilitation in physiotherapy practice. Phys Ther Rev. 2010;15:23-8.
11. Bradley PS, Olsen PD, Portas MD. The effect of static, ballistic and PNF stretching on vertical jump performance. J Strength Cond Res. 2007;21(1):223-226.
12. Walker B. PNF stretching- video [internet]. [cited 2022 June 24]. Available from: https://www.youtube.com/watch?v=q5r83Obl2gk.
13. Sharman MJ, Cresswell AG, Riek S. Proprioceptive neuromuscular facilitation stretching: Mechanisms and clinical implications. Sport Med. 2006;36:929-39.
14. Weerapong P, Hume PA., Kolt GS. Stretching: Mechanisms and Benefits for Sport Performance and Injury Prevention. Phys Ther Rev. 2004;9:189-206.
15. Hindle KB, Whitcomb TJ, Briggs WO, Hong J. Proprioceptive Neuromuscular Facilitation (PNF): Its Mechanisms and Effects on Range of Motion and Muscular Function. J Hum Kinet. 2012;31:105-13.
16. Oxford Advanced Learner's Dictionary [internet]: Definition of Method by Oxford dictionary [cited 2022 June 24] Available from: https://www.oxfordlearnersdictionaries.com
17. Merriam Webster Dictionary [internet]:Definition of Concept by Merriam-Webster [cited 2022 June 24] Available from: https://www.merriam-webster.com/dictionary
18. Kleynen M, Beurskens A, Olijve H, Kamphuis J, Braun S. Application of motor learning in neurorehabilitation: a framework for health-care professionals. Physiother Theory Pract. 2020;36:1-20.
19. McMullen J, Uhl TL. A Kinetic Chain Approach for Shoulder Rehabilitation. J Athl Train. 2000;35:329-37.
20. Myers JB, Lephart SM. The Role of the Sensorimotor System in the Athletic Shoulder. J Athl Train. 2000;35:351-63.
21. Johnson GS, Johnson VS. The application of the principles and procedures of PNF for the care of lumbar spinal instabilities. J Man Manip Ther. 2002;10(2):83-105.
22. de Oliveira KCR, Sande de Souza LAP, Emilio MM, da Cunha LF, Lorena DM, Bertoncello D. Overflow using proprioceptive neuromuscular facilitation in post-stroke hemiplegics: A preliminary study. J Bodyw Mov Ther. 2019;23:399-404.
23. O'Sullivan SB. Strategies to Improve Motor Function. In: O'Sullivan SB, Schmitz TJ, Fulk GD. Physical Rehabilitation 6th ed. Philadelphia (PA) USA: FA Davis Company; 2014, p. 399-401
24. Knudson D. Fundamentals of Biomechanics 2nd ed. New York (NY): Springer Science+Business Media;2007.
25. McCrea PH, Eng JJ, Hodgson AJ. Biomechanics of reaching: Clinical implications for individuals with acquired brain injury. Disabil Rehabil. 2002;24:534-41.
26. Voss DE, Jonta MK, Meyers BJ. Proprioceptive neuromuscular facilitation – patterns and techniques. 3rd ed. New York (NY): Harper & Row publishers; 1985.
27. Edwards I, Jones M, Hillier S. The interpretation of experience and its relationship to body movement: A clinical reasoning perspective. Man Ther. 2006;11:2-10.
28. Shimura K, Kasai T. Effects of proprioceptive neuromuscular facilitation on the initiation of voluntary movement and motor evoked potentials in upper limb muscles. Hum Mov Sci. 2002;21:101-13.
29. Moreira R, Lial L, Teles Monteiro MG, Aragão A, Santos David L, et al. Diagonal movement of the upper limb produces greater adaptive plasticity than sagittal plane flexion in the shoulder. Neurosci Lett. 2017;643:8-15.
30. Lial L, Moreira R, Correia L, Aragão A, Santos David L, Coertjens M, et al. Proprioceptive neuromuscular facilitation increases alpha absolute power in the dorsolateral prefrontal cortex and superior parietal cortex. Somatosens Mot Res. 2017;34:204-12.
31. Brach JS, VanSwearingen JM, Gil A, Nadkarni NK, Kriska A, Cham R, et al. Program to improve mobility in aging (PRIMA) study: Methods and rationale of a task-oriented motor learning exercise program. Contemp Clin Trials. 2020;89:105912.
32. Rozevink SG, Hijmans JM, Horstink KA, van der Sluis CK. Effectiveness of task-specific training using assistive devices and task-specific usual care on upper limb performance after stroke: a systematic review and meta-analysis. Disabil Rehabil Assist Technol. 2021;0:1-14.
33. Liepert J, Uhde I, Gräf S, Leidner O, Weiller C. Motor cortex plasticity during forced-use therapy in stroke patients: a preliminary study. J Neurol. 2001;248:315-21.
34. Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ. 2010;44(1):75-84.
35. Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychon Bull Rev. 2016;23:1382-414.
36. Lee BK. Influence of the proprioceptive neuromuscular facilitation exercise programs on idiopathic scoliosis patient in the early 20s in terms of curves and balancing abilities: single case study. J Exerc Rehabil. 2016;12:567-74.
37. Cayco CS, Gorgon EJR, Lazaro RT. Effects of proprioceptive neuromuscular facilitation on balance, strength, and mobility of an older adult with chronic stroke: A case report. J Bodyw Mov Ther. 2017;21:767-74.
38. Smedes F, Giacometti da Silva L. Motor learning with the PNF-concept, an alternative to constrained induced movement therapy in a patient after a stroke; a case report. J Bodyw Mov Ther. 2019;23:622-7.
39. Peteraitis T, Smedes F. Scapula Motor Control Training with Proprioceptive Neuromuscular Facilitation in Chronic Subacromial Impingement Syndrome: A case report. J Bodyw Mov Ther. 2020;24(3):165-171.
40. Jeanbart K, Tanner-Bräm C. Mobilization of the neurodynamic system using proprioceptive neuromuscular facilitation decreases pain and increases mobility in lower extremities and Spine-A case report. J Bodyw Mov Ther. 2021;27:682-91.
41. Smedes F, Heidmann M, Keogh J. PNF- based Gait Rehabilitation-training after a Total Hip Arthroplasty in congenital pelvic malformation; A case report. Physiother Theory Pract. 2021;00:1-10.
42. Kofotolis N, Vrabas IS, Vamvakoudis E, Papanikolaou a, Mandroukas K. Proprioceptive neuromuscular facilitation training induced alterations in muscle fibre type and cross sectional area. Br J Sports Med. 2005;39:e11.
43. Gabriel DA, Kamen G, Frost G. Neural Adaptations to Resistive Exercise Mechanisms and Recommendations for Training Practices. 2006;36:133-49.
44. Areeudomwong P, Buttagat V. Comparison of core stabilisation exercise and proprioceptive neuromuscular facilitation training on pain-related and neuromuscular response outcomes for chronic low back pain: A randomised controlled trial. Malaysian J Med Sci. 2019;26:77-89.
45. Kofotolis N, Kellis E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain. Phys Ther. 2006;86:1001-12.
46. Mavromoustakos S, Beneka A, Malliou V, Adamidis A, Kellis E, Kagiaoglou A, et al. Effects of a 6-week Proprioceptive Neuromuscular Facilitation Intervention on pain and disability in individuals with chronic low back pain. J Phys Act Nutr Rehabil. 2015:2421-7824.
47. Anggiat L, Susy N, Manurung A, Wilson J, Manik H. Proprioceptive neuromuscular facilitation approach for low back pain: A review study. Int J Sport Exerc Health Res. 2022;6(2):81-7.
48. Arcanjo FL, Martins JVP, Moté P, Leporace G, Oliveira DA de, Sousa CS de, et al. Proprioceptive neuromuscular facilitation training reduces pain and disability in individuals with chronic low back pain: A systematic review and meta-analysis. Complement Ther Clin Pract. 2022;46:101505.
49. Suresh V, Karthikbabu S, Prem V. Proprioceptive Neuromuscular Facilitation in Chronic Low Back and Neck Pain and Disability: A Systematic Review and Meta-analysis. Phys Prac and Res. 2022; Pre press:1-16.
50. Smedes F. Breed denken in de fysiotherapie, Op zoek naar overeenkomsten [A wider perspective on physiotherapy a search for similarities]. Fysiopraxis 2004:34-37.
51. Smedes F. Connections between PNF and MT. Poster presented at: IFOMPT conference: 2008 Jun 8-13; Rotterdam, the Netherlands.
52. Maitland G, Hengevelde E, Banks K. English K. Maitland’s Vertebral Manipulation. 7th ed. Edinburgh, London: Elsevier, Butterworth Heineman; 2005.
53. Olson KA, Manual Physical Therapy of the Spine. 2nd ed. St Louis (MO): Elsevier; 2016
54. Abreu R, Lopes AA, Sousa ASP, Pereira S, Castro MP. Force irradiation effects during upper limb diagonal exercises on contralateral muscle activation. J Electromyogr Kinesiol. 2015;25:292-7.
55. de Zoete A, Rubinstein SM, de Boer MR, Ostelo R, Underwood M, Hayden JA, et al. The effect of spinal manipulative therapy on pain relief and function in patients with chronic low back pain: an individual participant data meta-analysis. Physiother (United Kingdom). 2021;112:121-34.
56. Tedla JS, Sangadala DR. Proprioceptive neuromuscular facilitation techniques in adhesive capsulitis: A systematic review and meta-analysis. J Musculoskelet Neuronal Interact. 2019;19:482-91.
57. Stepień A, Fabian K, Graff K, Podgurniak M, Wit A. An immediate effect of PNF specific mobilization on the angle of trunk rotation and the Trunk-Pelvis-Hip Angle range of motion in adolescent girls with double idiopathic scoliosis-a pilot study. Scoliosis Spinal Disord. 2017;12:1-10.
58. Maicki T, Bilski J, Szczygiel E, Trąbka R. PNF and manual therapy treatment results of patients with cervical spine osteoarthritis. J Back Musculoskelet Rehabil. 2017;30:1095-101.
59. Gunning E, Uszynski MK. Effectiveness of the Proprioceptive Neuromuscular Facilitation Method on Gait Parameters in Patients With Stroke: A Systematic Review. Arch Phys Med Rehabil. 2019;100(5):980-986.
60. Stephenson JB, Maitland ME, Beckstead JW, Anemaet WK. Locomotor Training on a Treadmill Compared With PNF Training in Adults With Chronic Stroke. Technol Innov. 2014;15:325-32.
61. Khanal D, Singaravelan RM, Khatri SM. Effectiveness of Pelvic Proprioceptive Neuromuscular Facilitation Technique on Facilitation of Trunk Movement in Hemiparetic Stroke Patients. 2013;3:29-37.
62. Ribeiro TS, de Sousa e Silva EMG, Sousa Silva WH, de Alencar Caldas VV, Silva DLA, Costa Cavalcanti FA, et al. Effects of a training program based on the Proprioceptive Neuromuscular Facilitation method on post-stroke motor recovery: A preliminary study. J Bodyw Mov Ther. 2014;18:526-32.
63. Sharma V, Kaur J. Effect of core strengthening with pelvic proprioceptive neuromuscular facilitation on trunk, balance, gait, and function in chronic stroke. J Exerc Rehabil. 2017;13:200-5.
64. Mirek E, Chwala W, Longawa K, Rudzinska M, Adamkiewicz P, Szczudlik A. Przydatnosc trójwymiarowej analizy lokomocji dla usprawniania ruchowego metoda PNF chorych na chorobe Parkinsona. Neurol Neurochir Pol. 2003(supl.5):89-102
65. Mirek E, Filip M, Banaszkiewicz K, Rudzińska M, Szymura J, Pasiut S, et al. The effects of physiotherapy with PNF concept on gait and balance of patients with Huntington's disease – pilot study. Neurol Neurochir Pol. 2015;49:354-7.
66. Alexandre de Assis IS, Luvizutto GJ, Bruno ACM, Sande de Souza LAP. The Proprioceptive Neuromuscular Facilitation Concept in Parkinson Disease: A Systematic Review and Meta-Analysis. J Chiropr Med. 2020;19:181-7.
67. Pereira MP. Proprioceptive neuromuscular facilitation does not increase blood pressure of healthy elderly women. Physiother Theory Pract. 2012;28:412-6.
68. Bujar-Misztal M, Chciałowski A. Influence of proprioceptive neuromuscular facilitation on lung function in patients after coronary artery bypass graft surgery. Adv Exp Med Biol. 2018;1116:11-17.
69. Pyszora A, Budzyński J, Wójcik A, Prokop A, Krajnik M. Physiotherapy programme reduces fatigue in patients with advanced cancer receiving palliative care: randomized controlled trial. Support Care Cancer. 2017;25:2899-908.
70. Lacquaniti F, Ivanenko YP, Zago M. Patterned control of human locomotion. J Physiol. 2012;590:2189-99.
71. Youdas JW, Adams KE, Bertucci JE, Brooks KJ, Steiner MM, Hollman JH. Magnitudes of gluteus medius muscle activation during standing hip joint movements in spiral-diagonal patterns using elastic tubing resistance. Physiother Theory Pract. 2015;31:410-7.
72. Perry J. Gait analysis normal and pathological function. Thorofare (NJ): Slack Incorporated; 1992.
73. 73. Yigiter K, Sener G, Erbahceci F, BayarK, Ülger ÖG, Akodogan S. A comparison of traditional prosthetic training versus PNF resistive gait training with trans-femoral amputees. Prosthet Orthot Int. 2002;26:213-7.
74. Sahay P, Prasad SK, Answer S, Lenka PK, Kumar R. Efficacy of proprioceptive neuromuscular facilitation techniques versus traditional prosthetic training for improving ambulatory function in transtibial amputees. Hong Kong Physiother J. 2014;32:28-34.
75. Anjum H, Amjad I, Malik AN. Effectiveness of proprioceptive neuromuscular facilitation techniques as compared to traditional strength training in gait training among transtibial amputees. J Coll Physicians Surg Pakistan. 2016;26:503-6.
76. Jaczewska-Bogacka J, Stolarczyk A. Improvement in Gait Pattern After Knee Arthroplasty Followed by Proprioceptive Neuromuscular Facilitation Physiotherapy. Adv Exp Med Biol. 2018;1096:1-9.
