Abstract
Trichomonas vaginalis is a common cause of symptomatic vaginitis in women. Trichomoniasis occurs more frequently in people with multiple sexual partners. Women often present with vaginal discharge, painful intercourse, urinary tract infection symptoms, vaginal itching, or pelvic pain. The strawberry cervix is a finding upon physical examination where the cervix has an erythematous, punctate, and papilliform appearance. The strawberry cervix is named because of its superficially similar appearance to a strawberry. As opposed to a more general inflammation of the cervix found in cervicitis, the strawberry cervix appearance is considered to be selectively associated with Trichomoniasis. The clinical image of Trichomonas vaginalis is rarely reported. We present a clinical image of the strawberry cervix in a woman diagnosed to have trichomonas vaginalis.
Keywords
Trichomoniasis, Trichomonas vaginalis, Strawberry cervix, Clinical image
Introduction
Trichomonas vaginalis is a unicellular, anaerobic flagellated protozoan, that inhabits the lower genitourinary tracts of women and men [1]. Around 120 million women worldwide suffer from Trichomonas vaginalis vaginitis every year. The infection is sexually transmitted and is believed to facilitate HIV transmission [2]. The commonest clinical finding of Trichomonas vaginalis is a profuse vaginal discharge with an unpleasant odor. The discharge may be yellow, gray, or green in color and may be frothy in appearance. The vaginal pH is 6 to 7. Vulvar erythema, edema, and pruritus can also be noted. The characteristic erythematous, punctate epithelial papillae or “strawberry” appearance of the cervix is apparent in only 10% of cases [1]. The strawberry cervix is rarely seen during a routine pelvic exam but can be detected during colposcopy. Symptoms are usually worse immediately after menses because of the transient increase in vaginal pH at that time [3].
Case Presentation
A 28 years old para I woman presented with the complaint of offensive yellow and slightly greenish vaginal discharge of 2 weeks duration. She also complained of dull aching lower abdominal pain and dysuria, but no vaginal bleeding, abdominal swelling, or reddish discoloration of urine. She had divorced her former spouse and currently, she is living with a new husband. She has no fever or dyspareunia. She had a history of Sexually transmitted infection (STI) treatment before. On physical examination, vital signs were in the normal range, with no tenderness on the abdominal examination. On speculum examination, the cervix is erythematous with a strawberry appearance (Figures 1 and 2). There was yellowish to slightly greenish malodorous vaginal discharge. Laboratory diagnosis of Trichomonas vaginalis was made via wet mount microscopic examination of vaginal swab. Flagellated and motile protozoa were seen (Figure 3). The complete blood count, urinalysis, and random blood sugar levels were all normal. She was also screened for HIV and found to be non-reactive. Pelvic ultrasound showed normal findings. The patient was given metronidazole 500 mg orally twice daily for 7 days. Her husband was also treated. She came on appointment after 3 months and she reported no symptoms and the cervix appeared normal.

Figure 1. Strawberry cervix (erythematous, punctate hemorrhagic spots in the cervix) and frothy slightly greenish discharge.
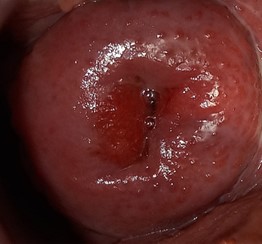
Figure 2. Magnified image of the strawberry cervix.
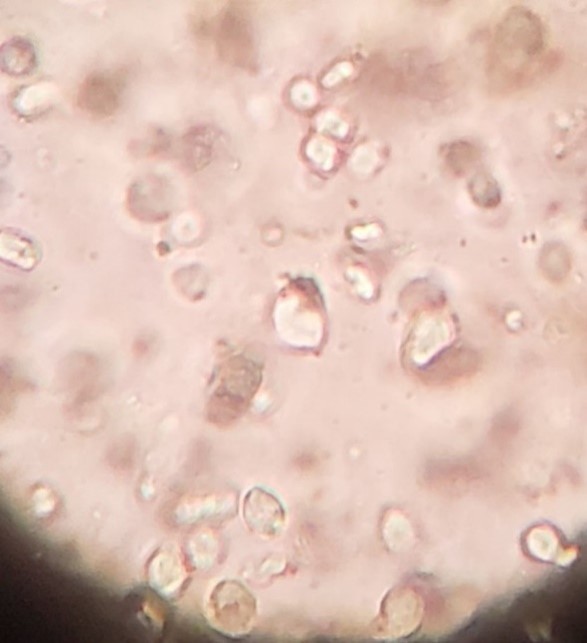
Figure 3. Wet mount microscopy showing flagellated trichomonas vaginalis (static image).
Discussion
Trichomoniasis is the third most common cause of vaginal discharge syndrome in Ethiopia preceded only by bacterial vaginosis (Gardnerella vaginalis) and candidiasis [4]. Although many women are asymptomatic, more than 50% of women with Trichomonas vaginalis infection have vaginal discharge. About 50% of symptomatic women report vulval itching. On examination, vulval erythema and edema may be noted. On speculum examination, a discharge of variable color can be seen in the vagina – classically described as yellow or greenish and may be frothy. The vaginal walls may be erythematous. The cervix may have punctate hemorrhages, giving rise to what has been referred to as the “strawberry cervix”. If the surface of the cervix becomes irritated and blanketed with small red dots, it’s known as the strawberry cervix. The red dots are tiny capillary hemorrhages (punctate hemorrhages). Although this finding is uncommon, it is highly indicative of trichomoniasis [1,5]. A ‘strawberry cervix’, which is seen in 2% of women with trichomoniasis, strongly indicates this diagnosis whereas the other clinical features are not specific to Trichomonas vaginalis infection [6,7].
Trichomonas vaginalis has historically been diagnosed by performing wet mount microscopy. Although it is not the gold standard technique for diagnosing trichomoniasis, a wet mount is frequently used because it is quick, inexpensive, and easy to perform. However, to have a good chance of successfully identifying the motile trichomonads, the slide should be read within 10 minutes of the collection since trichomonads quickly lose their motility [5]. Nucleic acid amplification tests (NAATs) have the highest sensitivity of all diagnostic methods to detect Trichomonas vaginalis [5,8].
The first line treatment is Metronidazole 2 grams, orally, in a single dose or Metronidazole 400 mg or 500 mg, twice daily for 7 days and the effective substitutes are tinidazole 2 grams orally, single dose or Tinidazole 500 mg orally, twice daily for 5 days [5]. Because metronidazole causes modest side effects such as epigastric pain, nausea, vomiting, diarrhea, and constipation, the patient must be reassured, and if symptoms are accentuated, other alternative medications should be provided. Concurrent treatment of all sex partners is vital for preventing reinfections. Among sexually active persons, the best way to prevent genital trichomoniasis is through consistent and correct use of condoms [9].
Conclusion
A clinician discovering a strawberry appearance on the cervix would have a high suspicion of Trichomonas infection. Though it is uncommon to find this typical finding of Trichomonas vaginalis, it is always better to do a speculum examination and to do vaginal discharge analysis to early identify and treat trichomoniasis.
List of Abbreviations
HIV: Human Immunodeficiency Virus; HPV: Human Papilloma Virus; NAAT: Nucleic Acid Amplification Test; pH: Potential of Hydrogen; STI: Sexually Transmitted Infection.
Declarations
Consent was taken from the client to take images.
References
2. Prevention CfDCa. Sexually Transmitted Infections Treatment Guidelines, 2021. 2021;70.
3. Forna F, Gülmezoglu AM, Group CID. Interventions for treating trichomoniasis in women. Cochrane Database of Systematic Reviews. 1996;2019(5).
4. Health FDRoEMo. National guidelines for the management of sexually transmitted infections using syndromic approach. 2015.
5. WHO. Guidelines for the management of symptomatic sexually transmitted infections: World Health Organization; 2021.
6. Lewis D. Trichomoniasis. Medicine. 2014;42(7):369-71.
7. Vatanshenassan M, Rezaie S, Mohebali M, Niromand N, Kazemi B, Babaei Z, et al. Trichomonas vaginalis: investigation of a novel diagnostic method in urine samples using cysteine proteinase 4 gene and PCR technique. Experimental Parasitology. 2010;126(2):187-90.
8. Fichorova R, Fraga J, Rappelli P, Fiori PL. Trichomonas vaginalis infection in symbiosis with Trichomonasvirus and Mycoplasma. Research in Microbiology. 2017;168(9-10):882-91.
9. Hazra A, Collison MW, Davis AM. CDC sexually transmitted infections treatment guidelines, 2021. JAMA. 2022;327(9):870-1.
