Abstract
Systemic Lupus Erythematosus (SLE) is a devastating disease, which affects several organs and with poor therapeutic options. Cathelicin LL37 is an antimicrobial peptide (AMP) with pleiotropic functions on immune cells and parenchymal cells, which can be implicated in inflammatory pathways and in immune regulation. LL37, a stimulator of both the innate and the adaptive immune responses in psoriasis and related psoriatic arthritis (PsA), can represent a relevant model autoantigen to study the effect of irreversible post-translational modifications (PTM) in SLE, as compared to psoriasis and PsA. Being a relevant SLE antigen too, knowing whether irreversible PTM of a self-antigen play a role in SLE, can help shed light on SLE pathogenic mechanisms that contribute to disease, but remain underscored. This is of particular interest for SLE, a disease in the need of new therapy targets, although the concept necessarily also applies to PsA. For instance, the effect of PTM such as citrullination and carbamylation, usually studied in other diseases, especially in Rheumatoid Arthritis (RA), can shed light on new pathways favored by inflammation dominated by neutrophil infiltration, typical not only of RA, but in fact also present in SLE tissues, and not least, in the skin and joints of psoriasis and PsA, respectively.
Keywords
Systemic lupus erythematosus (SLE), Post-translational modifications (PTM), LL37, antimicrobial peptides (AMP), Neutrophils
Commentary
Systemic Lupus Erythematosus (SLE) is the prototype of Immune-globulin (Ig)-immune-complex driven disease, in which autoantibody-complexes are deposited in tissues and contribute to inflammation [1]. The disease can be very severe and debilitating, and still disposes of poor pharmacological options [1]. SLE pathogenesis is partly understood, but not completely elucidated. Thus, there is a special need to know in deeper details the several pathogenic pathways at work. As for autoimmunity in general, some pathogenic mechanisms can be shared by more than one pathologic condition. Knowing the pathways at work in one disease can help uncover new mechanisms relevant for other diseases.
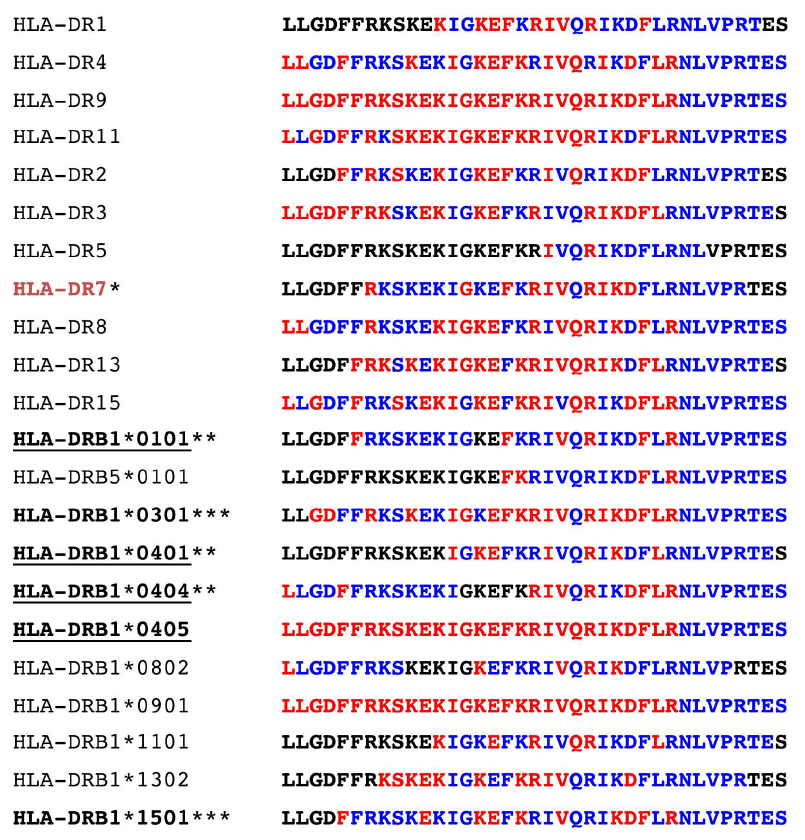
LL37 is an antimicrobial peptide (AMP) highly cationic, as its sequence contains several arginines and lysines [2]. It possesses several effects and regulatory functions and acts as chemotactic factor for neutrophils [3]. In autoimmune settings, almost 13 years ago, it was shown that LL37 is able to convert otherwise “inert” self-DNA in an efficacious trigger of Toll-like receptor (TLR) 9, acting as a “danger signal” and mediating immune amplification via activation of plasmacytoid dendritic cells (pDCs) [4]. Due to the type of structure formed, LL37-DNA complexes are efficient IFN-a inducers [5]. At that time, IFN-A was already known to mediate important effects in psoriasis, favoring psoriatic plaques formation [6]. Therefore, LL37-DNA complexes resulted to be the first identified “missing” trigger of IFN-A in psoriatic skin, followed by other AMP-nucleic acids complexes [4,7,8]. Later, it was demonstrated that LL37 plays an additional stimulatory role in psoriasis, by activating not only pDCs but also other innate immune cell types, as well as T-cells [9-11]. Indeed, LL37 is frequently recognized by T-cells as an autoantigen in psoriasis [11]. LL37 can be easily presented by various HLA-DR alleles, as it appears to possess the so-called “promiscuous binding motifs” suitable for binding to the common HLA-DR alleles (Figure 1).
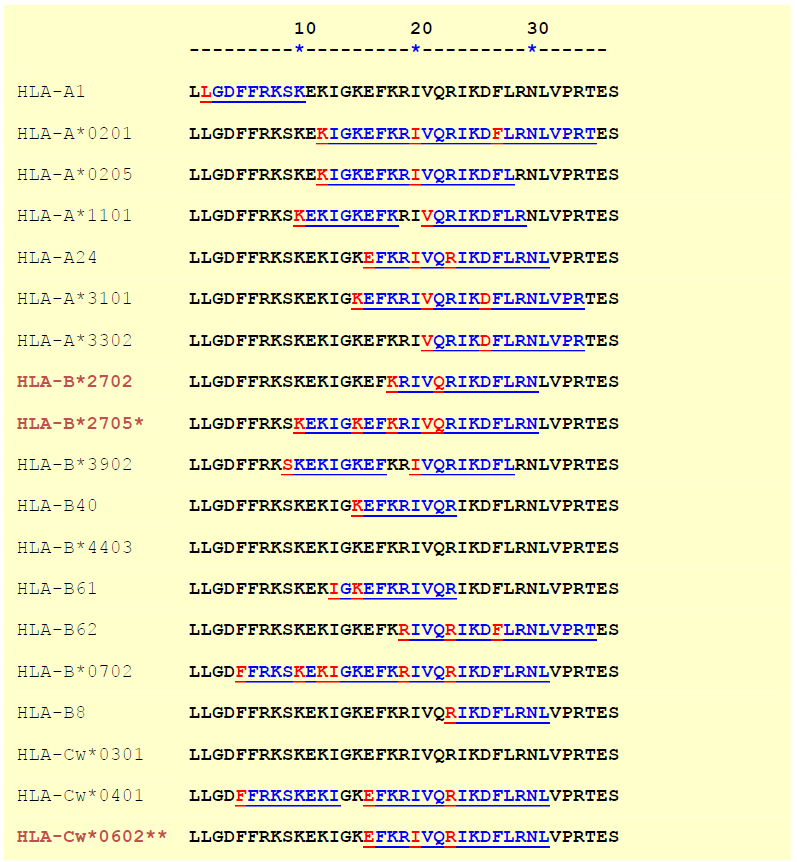
This is also valid in the context of HLA-class I presentation to CD8 T-cells. Several HLA-Class I alleles are likely to bind LL37-derived peptides in different frames. These alleles also include the psoriasis associated HLA-Cw6*02 and the HLA-B27 allele, more prominent in psoriatic disease (PsA), and especially frequent in another seronegative arthritis: Ankylosing spondylitis (AS) (Figure 2) [11-14].
In psoriasis, LL37 is produced in an aberrant manner by keratinocytes, upon triggers such as wounds or infections [15,16]. However, LL37 is also abundantly released by neutrophils [17,18]. Thus, we have reasoned that the mechanisms that allow LL37 to act as danger molecule, as wells as an autoantigen in psoriasis, could be also operative in SLE. In fact, SLE is characterized by a very intense neutrophilic inflammation in the skin and kidney and by a neutrophilic signature [1,19]. LL37 is abundantly released by neutrophils, also during neutrophil extracellular trap (NET) formation, a process characterized by a massive release of cell material, together with nucleic acids [17,18].
The intense pro-IFN-a inducer effect of the released LL37-DNA complexes, suggests that LL37 is an important trigger of nucleic acid-sensing receptors, and therefore a significant actor in SLE. Indeed, a typical IFN-a signature characterizes SLE [1]. This idea was reinforced when anti-LL37 antibody reactivity was detected in SLE and shown to correlate with disease activity and IFN-a [17]. Subsequently, it was also shown that LL37-DNA [20], and even LL37-RNA complexes [21], help the maturation of memory B-cells into antibody secreting plasma-cells, suggesting a mechanism that amplifies autoantibody production, independent on T-cell help.
Being LL37 a frequent SLE antibody target [17], and knowing that LL37 was recognized with a consistent frequency by T-cell in half of psoriasis patients [11], it was natural to search for T-cell reactivity to LL37 in SLE and address the possibility that LL37-specific T-cells might concur to the generation and maintenance of anti-LL37 antibodies.
In March 2020, we have published in Scientific Reports, the data on LL37 ability to act as a T-cell autoantigen in SLE [22]. Thus, LL37 is not only an antibody target in SLE, but T-cells specific for the same autoantigen may direct the production of anti-LL37 antibodies with pathogenic functions [22]. Indeed, we have also shown that these SLE-derived anti-LL37-antibodies induced a NET-like cell death of the SLE neutrophils in vitro, whereas LL37- specific T-cells, detected in blood, correlated with anti- LL37 antibodies, as well as with disease activity expressed as Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) [22]. What is the difference between these LL37- specific SLE T-cells and the T-cells described in psoriasis? Unlike psoriasis T-cells, SLE LL37-specific T-cells of SLE can up-regulate T-helper follicular (Thf) cell markers, such as Bcl-6, CXCR5, PD1 and ICOS. In addition, in vitro, they appear to direct the secretion of anti-LL37 antibodies by SLE B-cells. In keeping with the different polarization of LL37-specific T-cells, LL37 antibodies are frequently present in SLE but are only sporadically detected in psoriasis patients [22,23].
There is a consistent piece of scientific literature which concerns the importance of post-translational modifications (PTM) of self-proteins in activating autoreactive T-cells, as it is likely that modified autoantigens do not elicit T-cell tolerance, also because some of these PTM of self-proteins may not be seen by maturing thymocytes in the thymus, during negative selection [24]. Several studies have been performed in Rheumatoid Arthritis (RA), because in this disease there is a high reactivity to citrullinated peptides (anti-citrullinated protein antibodies, ACPA, are indeed considered a disease biomarker) [25]. This reactivity is also present in SLE but is less frequent than in RA [26-27]. However, it is possible that the autoantigens recognized in RA are actually only partially overlapping with those that are recognized in SLE, and perhaps the available standard assays for detection of ACPA are more appropriate for studies in RA than in SLE.
However, LL37 turns out to be a useful model antigen to understand whether permanent PTM, like citrullination, can affect T-cell reactivity in diseases other than RA and, consequently, B-cell reactivity [22,23]. For instance, we first addressed this in arthritis associated with psoriasis, namely psoriatic arthritis (PsA) [23]. Here we detected the presence of autoantibodies to LL37 and to its modified forms. In PsA, we found antibodies to LL37 (especially in the PsA-affected joints). In circulation, we found anti-carbamylated LL37 (anti-carb-LL37) antibodies, correlating with inflammatory parameters and, less frequently, anti cit-LL37 antibodies [23].
However, LL37, for its amino acidic natural composition, can be modified by both citrullination (at arginine residues) and by carbamylation (at leucin/lysine residues) [28,29]. Both PTM are irreversible and similar, as the amino acid citrulline and homocitrulline have a similar structure and change the resulting charge of LL37 in a similar manner [28,29].
LL37 can be modified at all five arginine residues yielding a fully citrullinated LL37 that can lose its DNA binding ability, but still maintains immunogenicity [22,28,29]. In our recent study in Scientific Reports we concentrated our attention on citrullination of LL37, also because it had been shown previously that citrullination can occur in SLE kidney [30]. Moreover, diffuse citrullination is a phenomenon also ascribed to neutrophil death via membranolytic pathways, named Leukotoxic Hypercitrullination, a pathway induced by membrane attack complexes (MAC) [31]. It can therefore be linked to complement activation, present in SLE tissues [32]. For instance, MAC deposition is present in both SLE tissues [33]. Interestingly, LL37 binding to the HLA-DR molecules is preserved in the citrullinated peptide form, suggesting that citrullinated LL37 (cit-LL37) can be presented to T-cells in an efficient manner [22]. Notably, cit-LL37 was able to recall in vitro the response to native LL37, in that after culture with cit-LL37, ex vivo native LL37-specific T-cells could be stained by peptide-MHC-tetramers loaded with native LL37 epitopes [22].
Since in the past, sign of citrullination were found in SLEaffected kidney, and we detected cit-LL37 in SLE-affected tissues, (skin and kidney), it is highly probable that cit- LL37 concurs to autoimmunity in SLE [22,30]. Some of the cit-LL37 specific T-cells in SLE are indeed crossreactive to the native antigen and T-cells specific for cit- LL37 alone can drive the production of anti-native LL37 antibodies [22].
As mentioned above, LL37 is also a substrate for carbamylation, a reaction that is not directly mediated by enzymes, while citrullination depend on peptidyl arginine deiminase (PAD) enzymes that can be released by activated neutrophils in tissues. However, it has been recently shown that carbamylation can be favored by neutrophil-derived myeloperoxidase (MPO) by catalyzing oxidation of thiocyanate in vitro and in vivo [31-34]. As for citrullination, also carbamylation has been mainly studied in RA [24]. In RA anti-carbamylated proteins antibodies (called anti-car-P antibodies) are often detected. We demonstrated the presence of cit-LL37 SLE affected kidney and skin but we believe that it is likely that carbamylation of LL37 also occurs in SLE, as both MPO and LL37 can be released by activated neutrophils, and during NET-like cell death in SLE tissues [22].
Thus, next steps will be to address whether carbamylation of LL37 also affects B- and T-cell reactivity in SLE. Anticarbamylated peptide antibodies have been detected in SLE [26], and they could be either cross-reactive to the native antigens or to the citrullinated antigens, as shown recently for the RA antibodies, which had to be studied at the clonal level [35]. As mentioned, in PsA we detected the presence of circulating antibodies reacting to carb-LL37, and they correlated with several inflammatory parameters [23]. Although in our study in PsA cit-LL37 directed antibodies did not correlate with disease parameters, anti-cit-LL37 antibodies were also detected and they sporadically appear in psoriasis patients’ blood [22,23]. Notably, inflamed joints are infiltrated with neutrophils and both cit-LL37 and carb-LL37 could be locally produced. Thus, SLE and PsA have in common a neutrophilic inflammation, an autoantigen, and possibly, the same modified autoantigen. It is likely that similar pathogenic mechanisms operate in SLE and PsA. Moreover, it is possible that sign of specific pathways activation in the psoriasis preceding PsA, could be taken as a prognostic marker.
In psoriasis, anti-cit-LL37 specific T-cells were also detected, although at lower extent than in SLE [22]. Possibly, cit-LL37-directed T-cell reactivity (or even carb- LL37 T-cell reactivity) could be more evident in those patients that have a neutrophil infiltrate in their lesioned skin.
Interestingly, anti carb-LL37 antibodies are sporadically present in psoriasis [22,23]. Perhaps an early detection of anti-carbamylated protein antibodies in circulation of psoriasis patients could be a marker of progression to PsA. We are currently addressing whether this occurs in psoriatic disease.
It is interesting that two diseases with a different genetic background share the same autoantigen, and likely the same modification of this autoantigen. However, as for psoriasis [22,23], reactivity could be qualitatively different. We found that SLE and PsA have both significant responses to LL37 in terms of autoantibodies to LL37 but that the magnitude of the antibody response in SLE is significantly higher than in PsA (Frasca L and Lande R, unpublished observations, 2020). It is possible that such antibodies have different properties, due to differential strength of antigen-recognition. But also, T-cells specific to the same antigen may also be qualitatively different. For instance, their polarization and cytokine/chemokines secretion pathways may diverge and concur to activate different pathogenic mechanisms. Alternatively, the two diseases have more in common than what has been previously appreciated. The study of shared autoantigens (like LL37, and possibly many other autoantigens) in different autoimmune/auto-inflammatory diseases such as SLE, PsA, psoriasis and possibly AS, can offer the opportunity to better appreciate the analogies and the divergences of the pathogenic pathways operating in chronic diseases, as well as the role of particular PTM. This knowledge will guide more efficacious therapeutic approaches, while avoiding pharmacological interventions that could be counterproductive.
Sources of Funding
This article was partially supported by the National Psoriasis Foundation, USA, Translational research grant 2019-2021, the “Ricerca Finalizzata” (CO-2013- 02356463), Ministry of Health, Italy, and the FOREUM Foundation, Switzerland.
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contributions
LF wrote the manuscript and RL contributed to writing and editing. Both authors approved the final version.
Acknowledgements
Not applicable. Only the authors listed on the manuscript contributed towards this article.
References
2. Zanetti M. Cathelicidins, multifunctional peptides of the innate immunity. Journal of Leukocyte Biology. 2004 Jan;75(1):39-48.
3. Yang D, Chen Q, Schmidt AP, Anderson GM, Wang JM, Wooters J, et al. LL-37, the neutrophil granule–and epithelial cell–derived cathelicidin, utilizes formyl peptide receptor–like 1 (FPRL1) as a receptor to chemoattract human peripheral blood neutrophils, monocytes, and T cells. The Journal of Experimental Medicine. 2000 Oct 2;192(7):1069-74.
4. Lande R, Gregorio J, Facchinetti V, Chatterjee B, Wang YH, Homey B, et al. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 2007 Oct;449(7162):564-9.
5. Schmidt NW, Jin F, Lande R, Curk T, Xian W, Lee C, et al. Liquid-crystalline ordering of antimicrobial peptide–DNA complexes controls TLR9 activation. Nature Materials. 2015 Jul;14(7):696-700.
6. Nestle FO, Conrad C, Tun-Kyi A, Homey B, Gombert M, Boyman O, et al. Plasmacytoid predendritic cells initiate psoriasis through interferon-a production. The Journal of Experimental Medicine. 2005 Jul 4;202(1):135-43.
7. Tewary P, de la Rosa G, Sharma N, Rodriguez LG, Tarasov SG, Howard OZ, et al. ß-Defensin 2 and 3 promote the uptake of self or CpG DNA, enhance IFN-a production by human plasmacytoid dendritic cells, and promote inflammation. The Journal of Immunology. 2013 Jul 15;191(2):865-74.
8. Lande R, Chamilos G, Ganguly D, Demaria O, Frasca L, Durr S, et al. Cationic antimicrobial peptides in psoriatic skin cooperate to break innate tolerance to self-DNA. European Journal of Immunology. 2015 Jan;45(1):203-13.
9. Ganguly D, Chamilos G, Lande R, Gregorio J, Meller S, Facchinetti V, et al. Self-RNA–antimicrobial peptide complexes activate human dendritic cells through TLR7 and TLR8. Journal of Experimental Medicine. 2009 Aug 31;206(9):1983-94.
10. Chamilos G, Gregorio J, Meller S, Lande R, Kontoyiannis DP, Modlin RL, et al. Cytosolic sensing of extracellular self-DNA transported into monocytes by the antimicrobial peptide LL37. Blood, The Journal of the American Society of Hematology. 2012 Nov 1;120(18):3699-707.
11. Lande R, Botti E, Jandus C, Dojcinovic D, Fanelli G, Conrad C, et al. The antimicrobial peptide LL37 is a T-cell autoantigen in psoriasis. Nature Communications. 2014 Dec 3;5(1):1-6.
12. Chen L, Tsai TF. HLA-Cw6 and psoriasis. British Journal of Dermatology. 2018 Apr;178(4):854-62.
13. MacLean IL, Iqball S, Woo P, Keat AC, Hughes RA, Kingsleyj G, et al. HLA-B27 subtypes in the spondarthropathies. Clinical & Experimental Immunology. 1993 Feb;91(2):214-9.
14. Winchester R, Giles J, Jadon D, Haroon M, McHugh N, FitzGerald O. Implications of the diversity of class I HLA associations in psoriatic arthritis. Clinical Immunology. 2016 Nov 1;172:29-33.
15. Harder J, Schröder JM. Psoriatic scales: a promising source for the isolation of human skin-derived antimicrobial proteins. Journal of Leukocyte Biology. 2005 Apr;77(4):476-86.
16. Korman NJ. Management of psoriasis as a systemic disease: what is the evidence?. British Journal of Dermatology. 2020 Apr;182(4):840-8.
17. Lande R, Ganguly D, Facchinetti V, Frasca L, Conrad C, Gregorio J, et al. Neutrophils activate plasmacytoid dendritic cells by releasing self-DNA-peptide complexes in systemic lupus erythematosus. Sci Transl Med. 2011 Mar 9;3(73):73ra19.
18. Herster F, Bittner Z, Archer NK, Dickhöfer S, Eisel D, Eigenbrod T, et al. Neutrophil extracellular trap-associated RNA and LL37 enable self-amplifying inflammation in psoriasis. Nature communications. 2020 Jan 8;11(1):1-3.
19. Bennett L, Palucka AK, Arce E, Cantrell V, Borvak J, Banchereau J, et al. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. Journal of Experimental Medicine. 2003 Mar 17;197(6):711-23.
20. Gestermann N, Di Domizio J, Lande R, Demaria O, Frasca L, Feldmeyer L, et al. Netting neutrophils activate autoreactive B cells in lupus. The Journal of Immunology. 2018 May 15;200(10):3364-71.
21. Lande R, Mennella A, Palazzo R, Pietraforte I, Stefanantoni K, Iannace N, et al. Anti-CXCL4 Antibody Reactivity Is Present in Systemic Sclerosis (SSc) and Correlates with the SSc Type I Interferon Signature. International Journal of Molecular Sciences. 2020 Jan;21(14):5102.
22. Lande R, Palazzo R, Gestermann N, Jandus C, Falchi M, Spadaro F, et al. Native/citrullinated LL37-specific T-cells help autoantibody production in Systemic Lupus Erythematosus. Scientific Reports. 2020 Apr 3;10(1):1-4.
23. Frasca L, Palazzo R, Chimenti MS, Alivernini S, Tolusso B, Bui L, et al. Anti-LL37 antibodies are present in psoriatic arthritis (PsA) patients: new biomarkers in PsA. Frontiers in Immunology. 2018 Sep 12;9:1936.
24. Doyle HA, Mamula MJ. Posttranslational modifications of self-antigens. Annals of the New York Academy of Sciences. 2005 Jun;1050(1):1-9.
25. Pruijn GJ. Citrullination and carbamylation in the pathophysiology of rheumatoid arthritis. Frontiers in immunology. 2015 Apr 27;6:192.
26. Ceccarelli F, Perricone C, Colasanti T, Massaro L, Cipriano E, Pendolino M, et al. Anti-carbamylated protein antibodies as a new biomarker of erosive joint damage in systemic lupus erythematosus. Arthritis research & therapy. 2018 Dec;20(1):126.
27. Wang Y, Liu H, Fu Y, Kao W, Ji Y, Liu X, et al. Novel biomarkers containing citrullinated peptides for diagnosis of systemic lupus erythematosus using protein microarrays. Clin. Exp. Rheumatol. 2019 Feb 15;6:929- 36.
28. Koro C, Hellvard A, Delaleu N, Binder V, Scavenius C, Bergum B, et al. Carbamylated LL-37 as a modulator of the immune response. Innate Immunity. 2016 Apr;22(3):218- 29.
29. Wong A, Bryzek D, Dobosz E, Scavenius C, Svoboda P, Rapala-Kozik M, et al. A novel biological role for PADs: Citrullination of cathelicidin LL-37 controls the immunostimulatory potential of cell-free DNA. Journal of Immunology (Baltimore, Md.: 1950). 2018 Apr 1;200(7):2327.
30. Bollain-y-Goytia JJ, Ramirez-Sandoval R, Daza L, Esparza E, Barbosa O, Ramirez D, et al. Widespread expression of inducible NOS and citrulline in lupus nephritis tissues. Inflammation Research. 2009 Feb 1;58(2):61-6.
31. Konig MF, Andrade F. A critical reappraisal of neutrophil extracellular traps and NETosis mimics based on differential requirements for protein citrullination. Frontiers in Immunology. 2016 Nov 4;7:461.
32. Botto M, Kirschfink M, Macor P, Pickering MC, Würzner R, Tedesco F. Complement in human diseases: lessons from complement deficiencies. Molecular Immunology. 2009 Sep 1;46(14):2774-83.
33. Wang S, Wu M, Chiriboga L, Zeck B, Belmont HM. Membrane attack complex (mac) deposition in lupus nephritis is associated with hypertension and poor clinical response to treatment. In: Seminars in arthritis and rheumatism, WB Saunders; 2018 Oct 1 (Vol. 48, No. 2, pp. 256-262).
34. Delporte C, Boudjeltia KZ, Furtmüller PG, Maki RA, Dieu M, Noyon C, et al. Myeloperoxidase-catalyzed oxidation of cyanide to cyanate: A potential carbamylation route involved in the formation of atherosclerotic plaques?. Journal of Biological Chemistry. 2018 Apr 27;293(17):6374-86.
35. Kissel T, Reijm S, Slot LM, Cavallari M, Wortel CM, Vergroesen RD, et al. Antibodies and B cells recognising citrullinated proteins display a broad cross-reactivity towards other post-translational modifications. Annals of the Rheumatic Diseases. 2020 Apr 1;79(4):472-80.