Abstract
Undifferentiated embryonal sarcoma of the liver (UESL) is an uncommon malignant neoplasm in the pediatric population, accounting for a small fraction of primary hepatic tumors but associated with an aggressive clinical course and poor prognosis. Surgical resection remains the mainstay of treatment; however, extended hepatectomy can leave patients with limited functional reserve and predispose them to hepatic failure, making liver transplantation (LT) a therapeutic alternative in selected cases.
We present the case of a 7-year-old female patient with UESL who initially underwent extended right hepatectomy. Despite an adequate immediate postoperative outcome, she subsequently developed progressive hepatic dysfunction and complications related to portal hypertension. Due to clinical deterioration and absence of curative options, the patient was listed for LT and successfully underwent transplantation using the classical split-liver technique. The postoperative course was favorable, with early weaning from vasoactive and ventilatory support, prompt recovery of oral intake, and hospital discharge on postoperative day ten. At present follow-up, she remains clinically stable with preserved graft function under immunosuppressive therapy.
This case highlights the role of LT as a life-saving option in pediatric patients with hepatic sarcomas who are not candidates for complete resection or who develop liver failure after major hepatectomy. Moreover, it emphasizes the importance of careful donor–recipient selection, specialized surgical expertise, and multidisciplinary follow-up to optimize outcomes in this challenging setting.
Keywords
Liver neoplasms, Liver transplantation, Hepatectomy, Sarcoma, Surgical procedures, Operative, Tissue transplantation, Liver regeneration
Abbreviations
eRL: Extended Right Lobes; GRWR: Graft to Recipient Weight Ratio; LT: Liver Transplant; UESL: Undifferentiated Embryonal Sarcoma of the Liver
Introduction
Pediatric liver transplant (LT) has been a fundamental pillar in the management of end-stage hepatic failure since its beginnings. In 1963, Thomas Sartzl performed the first attempt in a pediatric patient, a 3-year-old with biliary atresia. The indications for a liver transplant in children share many similarities with those of adults, and they include both acute and chronic liver diseases, hepatic neoplasias and genetically derived metabolic disorders that affect liver function [1]. Moreover, these indications vary by age group: in infants and children under 2 years of age, the leading cause is biliary atresia; in children aged 1 to 5 years, cholestatic diseases are the most common causes; and in adolescents aged 11 to 17 years, non-cholestatic cirrhosis and metabolic disorders with hepatic involvement predominate [2]. Among the malignant liver neoplasms, hepatic sarcomas make up a rare but clinically significant category, characterized by its aggressive biological behavior. The term “undifferentiated embryonal sarcoma of the liver” was first introduced in 1978 by Stocker and Ishak to describe a group of mesenchymal liver tumors that were lacking specific histological differentiation [3], it peaks in incidence between the ages of 6 and 10 years and has no predilection for sex, ethnic group or race. Despite its low incidence (1 per 1,000,000 inhabitants per year), it remains clinically significant due to its aggressiveness and rapid progression, making it a possible indication for liver transplant [2].
In general, liver transplant in the pediatric population, regardless of its etiology, has demonstrated favorable outcomes, with survival rates of approximately 85% at 10 years, as a result of a comprehensive medical management of those patients [4]. In the context of split liver transplant, called the classical technique, consists in dividing the liver from a cadaveric donor into two functional segments: a left lateral lobe graft (segments II and III), usually allocated to a pediatric recipient, and an extended right lobe graft (segments I and IV-VIII), generally used for an adult recipient. This technique allows for an increase in the number of available organs and a reduction in waitlist mortality; however, it requires a detailed anatomical evaluation of the donor and a high level of surgical expertise [1] as perioperative complications can still occur despite advanced care. Among the main complications are biliary alterations, such as stenosis or leaks at anastomosis sites, which are more common with split grafts, with rates close to 18% compared to the 7% observed in whole liver grafts. Moreover, portal vein thrombosis is also more frequent, especially in patients with small grafts, with reported rates above 14%. Other documented complications include intra-abdominal bleeding, primary graft dysfunction, and in some cases, small for size syndrome or, on the other hand, large for size syndrome in pediatric patients. Additionally, the risk of retransplantation is also found to be slightly increased in patients who receive split grafts, especially extended right lobes (eRL), due to greater technical complexity, longer cold ischemia times, and increased reconstructive requirements [1].
Lastly, it’s essential to emphasize the importance of strict donor and recipient selection, the involvement of experienced surgical teams in this technique, and close multidisciplinary follow-up tailored to the patient’s underlying condition.
Case Report
A 7-year-old female (born in 2003) with the diagnosis of undifferentiated liver sarcoma, confirmed by biopsy in May 2010 and extended right hepatectomy also in May of that same year. Twenty days later, she presented with elevated transaminases, and treatment with rehabilitation via ERCP was chosen. Adjuvant therapy was subsequently administered (ifosfamide, doxorubicin), and the port catheter was removed in June 2016. She then presented with transaminitis in May 2017 and was scheduled for a new liver biopsy, which reported a hepatic hemangioma that resolved spontaneously. Later, she developed biliary tract dilation secondary to hypertrophy of the caudate lobe, which was successfully treated endoscopically. Subsequently, in August 2019, she presented with upper gastrointestinal bleeding of variceal type and liver failure only due to portal hypertension, with a MELD score of 6 points. Therefore, it was decided to list her for a transplant protocol. A liver transplant using the classical technique was performed in March 2020, with good clinical progress, showing a peak in transaminases of 600 on postoperative day 1, discontinuation of vasopressors and ventilatory support on the same day, initiation of oral intake on postoperative day 3, and discharge on postoperative day 10, presenting only with dehiscence of the surgical wound at the skin level, which later developed into a granuloma.
She is currently under follow-up by our Transplant Unit with adequate graft function, on immunosuppression with tacrolimus, and presents a small incisional hernia of 2 cm, which will be repaired electively.
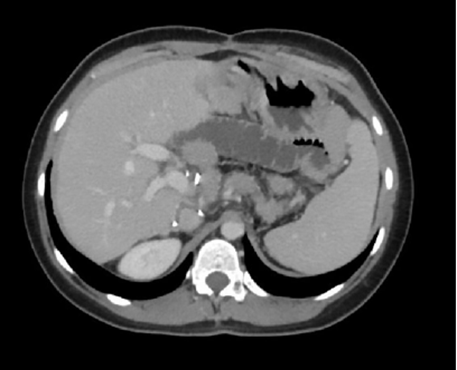
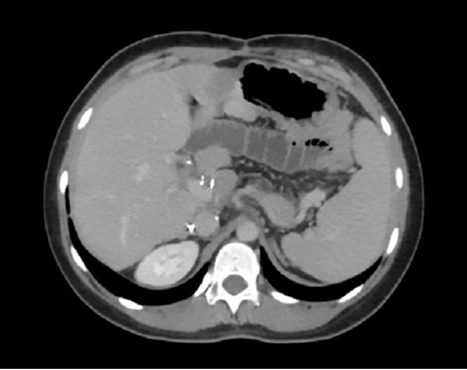
A B
Figures 1. A. and B. Contrast-enhanced abdominal computed tomography in the portal phase, corresponding to post–liver transplant follow-up studies.
Discussion
Long-term follow-up of pediatric patients who have undergone liver transplantation (LT) is essential to ensure graft stability and optimize their clinical outcomes as they grow and go through different stages of development. In most cases, these procedures are performed in children under five years of age [5], making the role of parents or caregivers crucial in managing treatment, working closely with a multidisciplinary team specialized in pediatric transplantation. However, as these children transition into adolescence and young adulthood, the responsibility for self-care gradually shifts to them, posing new challenges in treatment adherence and in the prevention of complications [6].
The maintenance of a functional graft largely depends on adherence to the therapeutic regimen, an especially critical aspect in the adolescent population, where non-adherence rates have been documented to range between 35% and 50%. This lack of compliance has serious consequences, including graft deterioration and decreased patient survival. Despite these risks, transplantation continues to represent a viable and highly effective therapeutic option, particularly for patients who have a strong support network and adequate medical follow-up [6].
There is a considerable percentage of young adult transplant recipients who experience adverse outcomes after transitioning to an adult hepatology care unit, with mortality rates between 24% and 28% in the first five years and a loss of follow up in up to 15% of patients, which highlights the importance of effective strategies for education, emotional support, and continuous monitoring to improve long-term survival and quality of life in these patients [6].
Additionally, recent studies have confirmed that anatomic resection remains the treatment of choice for large tumor’s such as UESL (Undifferentiated Embryonal Sarcoma of the Liver), and that liver transplantation can be considered a viable alternative when complete resection is not possible or when recurrences occur [7,8]. Despite its low incidence, UESL accounts for up to 13% of primary liver tumors in the pediatric age group, and its diagnosis is often delayed due to nonspecific clinical and imaging presentations [8,9]. Moreover, the use of advanced technological tools, such as computer-assisted three-dimensional reconstruction, has improved surgical planning and facilitated complete resection in complex cases of UESL, which enhances oncologic outcomes and lowers recurrence rates [9]. Therefore, individualization of surgical treatment is essential, considering tumor volume, its relationship with vascular structures, and the functional hepatic reserve of the pediatric patient.
On the other hand, split-liver transplantation represents a viable surgical technique when an adequate proportion between graft volume and recipient weight is ensured. The graft-to-recipient weight ratio (GRWR) is a key parameter for preventing small-for-size syndrome. Although a minimum value of 1.0% (equivalent to 10 mL/kg) has traditionally been established, some studies have reported successful outcomes with values ranging between 0.86% and 1.9% in adults receiving split-liver grafts [10,11]. Furthermore, a Chinese series of 22 adults who underwent full-right/full-left split-liver transplantation documented GRWR values between 1.16% and 1.65%, with favorable outcomes and no reported cases of primary graft dysfunction or need for retransplantation during hospitalization [12]. These findings support the safe use of grafts with proportions below 1.2%, down to at least a GRWR of 1.16%, as long as the graft has adequate structural and functional quality and there is careful donor-recipient selection. In the present case, the use of a graft via the classical technique was sufficient to meet the patient's metabolic needs without developing complications related to graft size [12].
Likewise, several studies have shown that split-liver transplantation, especially using the classical technique (which assigns a left lateral graft to a pediatric recipient and an extended right graft to an adult), has graft and patient survival rates comparable to those of whole-liver transplant. In the pediatric population, this type of technique, along with living donor liver transplant, has significantly reduced waitlist mortality, decreasing it from up to 40% to less than 10% in infants, without affecting long-term graft function [1]. Data from the Collaborative Transplant Study indicates that 5-year graft survival in children transplanted with split grafts reaches 80% in centers with extensive experience [1]. In adults, although higher rates of perioperative complications (particularly biliary and thrombotic) were reported in early stages, current evidence shows that, with proper donor and recipient selection, graft and patient survival at 1, 5, and 10 years remains around 80%, comparable to outcomes obtained with whole-liver grafts [10,11]. In a British cohort, extended right grafts achieved 79% graft survival at 10 years, while left lateral grafts used in pediatric recipients achieved patient survival rates close to 90% [11,12]. These results support the use of split-liver transplantation as a safe and effective alternative, without compromising clinical outcomes in either population.
Conclusion
Liver transplant in pediatric patients with rare neoplasias such as undifferentiated embryonal sarcoma of the liver offers complete medical and surgical management; however, the application of advanced surgical techniques such as split transplantations and a multidisciplinary follow-up has made it possible to achieve favorable survival rates. Despite the inherent complexity of these procedures and the risk of postoperative complications, transplantation remains a viable and effective therapeutic alternative to improve the prognosis and quality of life in these patients.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this case report.
Funding Statement
The authors received no financial support for this research.
Copyright and Permissions
The authors retain copyright of this article. This work is distributed under the terms of the Creative Commons Attribution License. The authors are responsible for obtaining permission for any copyrighted material used.
References
2. Ibáñez Pradas V, Cortés Cerisuelo M, Montalvá Orón E. Pediatric liver transplantation. Cir Pediatr. 2022 Jan 1;35(1):1–9.
3. Putra J, Ornvold K. Undifferentiated embryonal sarcoma of the liver: a concise review. Arch Pathol Lab Med. 2015;139(2):269–73.
4. Elmokattaf R, Aljumaa A, Alani M, Aljumaa J, Latta N, Basha HA, et al. Characterization of emergency department visits in pediatric patients within the first year of liver transplantation: ten years' experience in tertiary care center. BMC Emerg Med. 2025;25(1):76.
5. Meirelles Júnior RF, Salvalaggio P, Rezende MB, Evangelista AS, Guardia BD, Matielo CE, et al. Liver transplantation: history, outcomes and perspectives. Einstein (Sao Paulo). 2015;13(1):149–52.
6. Kosmach-Park B, Coyne B, Gupta N, Mazariegos G. Bridging the Gap: A Review of Pediatric to Adult Transition of Care in Liver Transplantation. Pediatr Transplant. 2025;29(1):e14900.
7. Lin WY, Wu KH, Chen CY, Guo BC, Chang YJ, Lin MJ, et al. Treatment of undifferentiated embryonal sarcoma of the liver in children. Cancers (Basel). 2024;16(5):897.
8. Bahador A, Forooghi M, Shahriarirad R, Geramizadeh B, Ataollahi M, Kamran H. A large undifferentiated sarcoma of the liver in a 13-year-old girl treated with anatomical resection: a case report and review of the literature. BMC Gastroenterol. 2022;22(1):2.
9. Xiu W, Li T, Liu J, Zhang J, Wang J, Wang F, et al. Undifferentiated embryonal sarcoma of the liver in children: our experience in four difficult cases and three-dimensional practical exploration. World J Surg Oncol. 2024;22(1):222.
10. Battula NR, Platto M, Anbarasan R, Perera MT, Ong E, Roll GR, et al. Intention to Split Policy: A Successful Strategy in a Combined Pediatric and Adult Liver Transplant Center. Ann Surg. 2017 May;265(5):1009–15.
11. Liu H, Li R, Fu J, He Q, Li J. Technical Skills Required in Split Liver Transplantation. Ann Transplant. 2016 Jul 1;21:408–15.
12. Ding L, Yu X, Zhang R, Qian J, Zhang W, Wu Q, et al. Full-Right Full-Left Split Liver Transplantation for Two Adult Recipients: A Single-Center Experience in China. J Clin Med. 2023 May 31;12(11):3782.
13. Stanton BF. Pediatric Critical Care Medicine. Pediatr Clin North Am. 2017;64(5):xv–xvi.
14. Halliday N, Westbrook RH. Liver transplantation: need, indications, patient selection and pre-transplant care. Br J Hosp Med (Lond). 2017 May 2;78(5):252–9.
15. Trotter JF. Liver transplantation around the world. Curr Opin Organ Transplant. 2017 Apr;22(2):123–7.
16. Ziogas IA, Zamora IJ, Lovvorn Iii HN, Bailey CE, Alexopoulos SP. Undifferentiated Embryonal Sarcoma of the Liver in Children Versus Adults: A National Cancer Database Analysis. Cancers (Basel). 2021 Jun 11;13(12):2918.
17. Babu BI, Bigam DL, Gilmour SM, Dajani KZ, Shapiro AM, Kneteman NM. Liver transplantation in locally unresectable, undifferentiated embryonal cell sarcoma. Transplant Direct. 2021;7(2):e654.