Abstract
Background: Hypoplastic internal carotid artery (HICA) is a rare congenital vascular anomaly, typically asymptomatic due to collateral circulation. However, in certain cases, it may present with ischemic stroke.
Case Presentation: We report a 17-year-old male with a history of smoking and illicit drug use who presented with acute left-sided weakness. Imaging revealed an infarct in the right middle cerebral artery territory and a hypoplastic right internal carotid artery.
Conclusion: This case highlights the importance of considering congenital vascular anomalies in young stroke patients and underscores the role of advanced neuroimaging in diagnosis.
Keywords
Acute stroke, Cocaine, Hypoplastic internal carotid artery (HICA)
Introduction
Congenital cerebrovascular anomalies, though rare, can have significant clinical implications, especially in younger patients presenting with stroke. Among these, hypoplastic internal carotid artery (HICA) is an uncommon anomaly with an estimated incidence of 0.01% [1]. These anomalies are classified into agenesis (complete absence), aplasia (absence with a remnant), and hypoplasia (underdevelopment) [2]. HICA is often asymptomatic due to compensatory collateral circulation via the contralateral internal carotid artery and vertebrobasilar system. However, in certain cases, this compensation may be insufficient, leading to ischemic events. The anatomical characteristics of HICA include a narrowed bony carotid canal and reduced vessel diameter, typically identified through advanced imaging modalities.
While most cases are discovered incidentally, symptomatic presentations such as stroke, transient ischemic attacks, or aneurysmal complications have been reported [3]. This case report presents a young male with ischemic stroke secondary to HICA, emphasizing the need for heightened clinical suspicion and thorough radiological evaluation in atypical stroke presentations.
Case Presentation
A 17-year-old adolescent male was admitted to the emergency department presenting sudden-onset weakness in the left arm and leg, along with headache and vomiting over the last 72 hours. There were no seizures, impaired mental status, or speech impairment noted. Neurological examination revealed weakness (power of 0/5 on the Medical Research Council scale), positive Babinski reflex, exaggerated knee and ankle reflexes, sustained ankle clonus on the left side, and evidence of upper motor neuron facial palsy. The rest of the clinical examination was completely unremarkable.
Laboratory investigations, including complete blood count, lipid profile, renal and liver function tests, serum electrolytes, serum calcium, coagulation profile (Table 1), C-reactive protein, and erythrocyte sedimentation rate, all yielded normal results. Cerebrospinal fluid analysis and antinuclear antibodies (ANA) testing were normal and negative, respectively. Ultrasound examinations of the abdomen and pelvis, echocardiography, renal Doppler ultrasound, and carotid Doppler showed no abnormalities.
|
Coagulation profile Test |
Patient |
Normal Range |
|
APTT |
32 seconds |
30 seconds |
|
PT |
14 seconds |
12 seconds |
|
INR |
1 |
1 |
|
TT |
13 |
12–19 sec |
|
Protein C |
85 |
65–135 IU/dl |
|
Protein S |
94 |
60–150% |
|
Fibrinogen |
240 |
200–400 mg/dl |
|
Anti-thrombin III |
94 |
80–130% |
|
Homocysteine |
8 |
<15 mcmol/l |
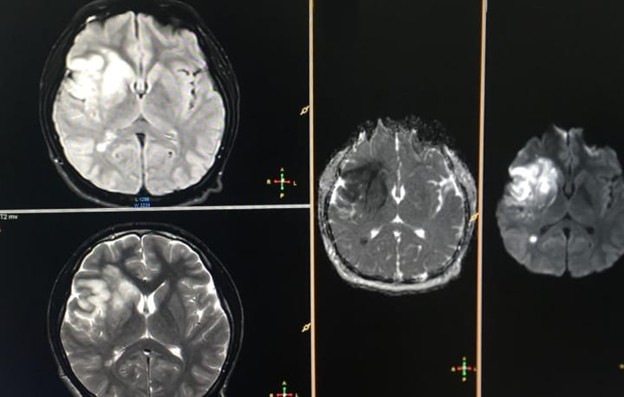
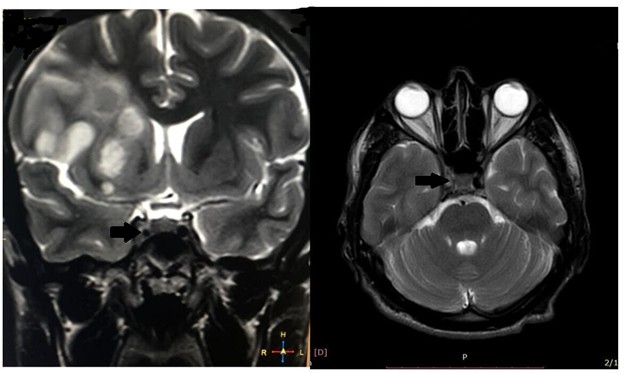
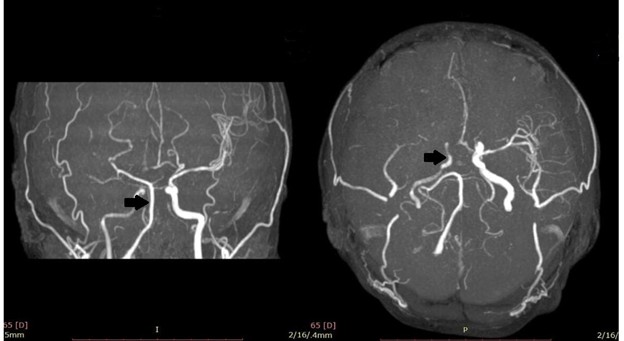
A non-contrast CT scan initially provided inconclusive results, prompting diffusion-weighted MR brain imaging, revealing an acute middle cerebral artery stroke (Figure 1). Subsequent MRI brain with MR venography demonstrated additional findings, including asymmetrical cavernous sinus and narrowed right internal carotid artery (Figure 2). Consequently, MRA of the carotid vasculature revealed a hypoplastic right internal carotid artery and abnormal appearances of the middle cerebral and anterior cerebral arteries, presenting as a beaded appearance at the petrous (C2), lateral, and cavernous (C4) segments, with collateral filling through the circle of Willis (Figure 3).
Figure1. Axial sections of the brain, including Flair, T2, and ADC/DWI sequences, reveal an acute MCA infarct.
Figure 2. Axial and sagittal T2-weighted image at the level of the cavernous sinuses demonstrates the absence of signal void within the intracavernous segment of the right internal carotid artery (ICA).
Figure 3. MRA showing a hypoplastic right internal carotid artery (ICA) with non-visualization of the M1 and M2 segments of the right middle cerebral artery (MCA).
A comprehensive evaluation systematically ruled out other potential causes of the stroke. A thorough evaluation systematically ruled out several potential causes for the stroke. First, cardiac sources and embolic events were investigated through echocardiography, which revealed no thrombi or other sources of embolism. Additionally, carotid duplex scanning showed normal flow and structure, with no evidence of carotid atherosclerosis. Imaging also did not demonstrate any characteristic stenosis associated with fibromuscular dysplasia. Dissection was ruled out, as there were no signs present in imaging studies. Furthermore, the classic "puff of smoke" appearance characteristic of moyamoya disease was absent. Large vessel vasculitis, including Takayasu and giant cell arteritis, was also excluded based on the patient’s age and normal inflammatory markers. The possibility of cerebral venous sinus thrombosis was not supported by the clinical presentation or imaging results. Other conditions, such as demyelinating diseases and tumors, were ruled out due to normal MRI findings. The coagulation profile was normal. Conversion disorder was considered but deemed unlikely based on the neurological examination and imaging results.
Treatment upon multidisciplinary advice commenced with antiplatelet therapy 75 mg aspirin daily and atorvastatin 20 mg nightly, alongside the initiation of a structured physiotherapy program. Upon reaching day 5 of admission, the patient was discharged with the prescribed medication regimen, advised to continue physiotherapy, and instructed to pursue rehabilitation as an outpatient. Follow-up imaging and monitoring of blood pressure and lipid profile were recommended.
Discussion
Hypoplastic internal carotid artery (HICA) is a rare congenital anomaly, often discovered incidentally due to its typically asymptomatic nature. However, in certain cases, such as the one presented here, HICA may contribute to ischemic stroke, particularly when collateral circulation is insufficient [4]. Symptoms of HICA include headache, seizure, tinnitus, transient ischemic attack, Horner syndrome, aneurysms, or stroke [5]. This case adds to the limited pool of documented symptomatic HICA presentations and underscores the importance of considering vascular anomalies in young stroke patients.
Unilateral HICA is more common than bilateral forms, with the right side being more frequently affected [6,7]. The embryological basis involves regression or underdevelopment of the third aortic arch and dorsal aorta, potentially influenced by mechanical factors such as amniotic band constriction [6,8]. In our patient, the hypoplastic right ICA was associated with absent M1 and M2 segments of the middle cerebral artery, suggesting compromised perfusion and collateral insufficiency. HICA is not directly linked to stroke but is a risk factor, so preventing ischemic events is crucial [9].
HICA has been associated with various neurological syndromes, including PHACE syndrome, moyamoya disease, and fibromuscular dysplasia [6,10]. These associations highlight the need for comprehensive evaluation when such anomalies are detected. Moreover, the condition is often underdiagnosed due to its silent course and reliance on advanced imaging modalities. Non-invasive techniques such as magnetic resonance angiography (MRA) and computed tomography angiography (CTA) have largely replaced catheter angiography, offering safer and more accessible diagnostic options [6,11].
Whitley et al. conducted a systematic review of congenital internal carotid artery hypoplasia, summarizing clinical presentations, imaging standards, and management strategies. Their findings emphasize the importance of early recognition, especially in patients undergoing neurosurgical or endovascular procedures, where anatomical variations may influence outcomes [6].
Management of HICA focuses on mitigating cerebrovascular risk through antiplatelet therapy, statins, and lifestyle modification. In symptomatic cases, long-term follow-up with imaging and monitoring of vascular risk factors is essential. Although surgical or endovascular interventions are rarely indicated for HICA itself, awareness of the anomaly is critical during planning for unrelated vascular procedures [12].
This case contributes to the growing recognition of HICA as a potential stroke risk factor in young patients. It reinforces the need for thorough vascular imaging in atypical stroke presentations and supports the inclusion of congenital anomalies in differential diagnoses.
Conclusion
Hypoplastic internal carotid artery is a rare but clinically significant vascular anomaly that may contribute to ischemic stroke in young individuals. This case underscores the importance of considering congenital vascular variants in the differential diagnosis of adolescent stroke. Early recognition through advanced imaging and proactive management of modifiable risk factors are essential for preventing recurrent cerebrovascular events. Further research is warranted to explore long-term outcomes and optimal surveillance strategies in patients with HICA.
Ethics Approval
Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent
This case report is exempt from our institution’s Institutional Review Board. Informed consent was obtained before collecting data, explaining the publication of neuroimaging and medical history without revealing the patient's identity.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Acknowledgment
We acknowledge the cooperation of the Medical D ward, Khyber Teaching Hospital, Peshawar, faculty.
Funding
None.
Conflict of Interest
Authors have no conflict of interest.
References
2. Lie TA, Hage J. Congenital anomalies of the carotid arteries. Plastic and Reconstructive Surgery. 1968 Sep 1;42(3):283.
3. Dawson AG, Wilson A, Maskova J, Murray AD, Reid JM, Kuhan G. Hypoplastic internal carotid artery stenosis with a low-lying carotid bifurcation causing cerebral ischemia. J Vasc Surg. 2012 Nov;56(5):1416–8.
4. Zink WE, Komotar RJ, Meyers PM. Internal carotid aplasia/hypoplasia and intracranial saccular aneurysms: series of three new cases and systematic review of the literature. J Neuroimaging. 2007 Apr;17(2):141–7.
5. Kaya O, Yilmaz C, Gulek B, Soker G, Cikman G, Inan I, et al. An important clue in the sonographic diagnosis of internal carotid artery agenesis: ipsilateral common carotid artery hypoplasia. Case Rep Radiol. 2014;2014:516456.
6. Whitley H, Zazay A, Skalický P, Malík J, Charvát F, Beneš V, et al. Congenital internal carotid artery hypoplasia: A systematic review. Neuroradiol J. 2023 Feb;36(1):5–16.
7. Ide C, De Coene B, Mailleux P, Baudrez V, Ossemann M, Trigaux JP. Hypoplasia of the internal carotid artery: a noninvasive diagnosis. Eur Radiol. 2000;10(12):1865–70.
8. Suri S, Lee WA, Park T, Lev S, Ramanathan AK. Congenital hypoplasia of the internal carotid artery: a short review. Brain Disord Ther. 2020;9:264.
9. Akdemir Aktaş H, Farımaz M, Fırat A, Göçmen R. Rare congenital anomalies of the internal carotid artery: anatomic and radiologic aspects of three cases and review of the literature. Surg Radiol Anat. 2020 Nov;42(11):1363–70.
10. Mežvinska P, Brokāns A, Pavlovičs S, Dravnieks M, Platkājis A, Balodis A. A Silent Threat: Internal Carotid Artery Hypoplasia and Its Role in Basilar Artery Aneurysm Formation-A Case Study. Diagnostics (Basel). 2025 Mar 19;15(6):774.
11. Rothwell PM. For severe carotid stenosis found on ultrasound, further arterial evaluation prior to carotid endarterectomy is unnecessary: the argument against. Stroke. 2003 Jul;34(7):1817–9.
12. Georgiadi E, Papavasileiou G, Sfyroeras GS. Bilateral hypoplasia of the internal carotid artery and ectasia of the internal jugular vein. J Vasc Surg Cases Innov Tech. 2023 Aug 18;9(4):101252.