Keywords
Zebrafish xenograft models, Cancer, CAR-T cells, Tumor, CRISPR
Commentary
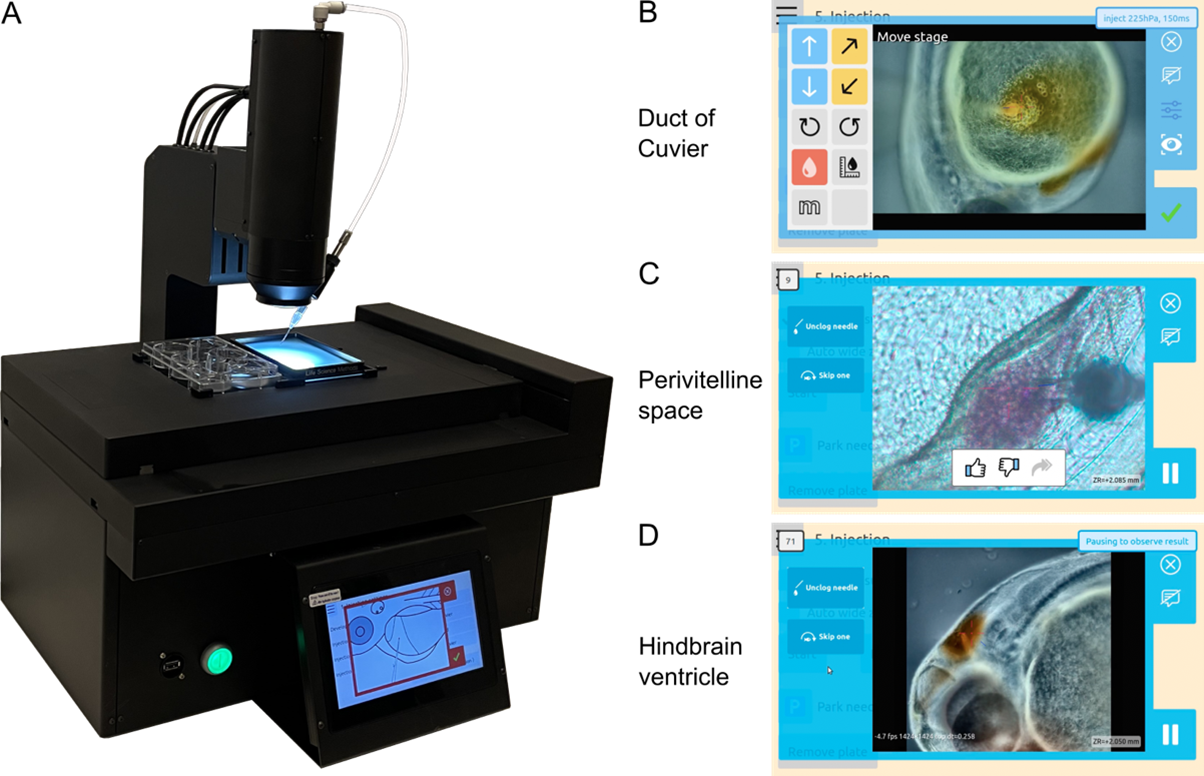
Zebrafish xenograft models have become indispensable in cancer biology for their capacity to recapitulate key aspects of human tumor progression in a live vertebrate system [1,2]. However, widespread adoption has been constrained by the technical demands of microinjection, which require extensive training, result in operator variability, and limit scalability. In our recent study published in npj Biomedical Innovations [3], we presented and validated an automated microinjection system (Figure 1) that significantly reduces operator dependency, increases throughput, and improves reproducibility in zebrafish xenotransplantation.
Figure 1. The automated microinjection system in operation. (A). Photograph of the automated microinjection system for zebrafish larvae (1–5 days post-fertilization). (B-D). Screenshots captured immediately following successful robotic injections, showing phenol red dye or labeled cancer cells delivered into the duct of Cuvier, the perivitelline space, and the hindbrain ventricle.
The system enables automated injections into three commonly used antomical sites—duct of Cuvier (vascular access), perivitelline space (subcutaneous-like), and hindbrain ventricle (orthotopic brain implantation). With adaptive image recognition and machine learning, the robot can autonomously detect larval orientation, align the needle to the optimal angle, identify skin puncture in real time, and deliver cells with precision. A detailed visual overview of the injection process was presented in our previous paper published in npj Biomedical Innovations [3]. The system was validated in multiple laboratories across Europe, including Bioreperia (Sweden), the Centre for Molecular Medicine Norway (Norway), Life Science Methods and Leiden University Medical Center (the Netherlands), and ZeClinics (Spain). Validation involved a broad range of human cancer cell lines (e.g., breast, bladder, and glioma), clinical biopsy samples, and immune effector cells such as tumor-infiltrating lymphocytes (TILs). On average, the results reveal an injection success rate of approximately 60% alongside larval survival rates exceeding 70%. These outcomes are comparable to manual approaches, while the fully automated mode operates at twice the speed.
From an immuno-oncology perspective, zebrafish larvae offer a unique immune-permissive window before adaptive immunity matures, enabling transient human immune and tumor cell co-engraftment without host immunosuppression. This allows in vivo investigation of immune evasion mechanisms, cell trafficking, and therapy response in a high-throughput format. As such, zebrafish primary cell line-derived tumor xenograft models have been used to track and quantify functional tumor cytotoxicity by co-implanted CAR-T cells [4], and elucidate novel mechanisms of immune-evasion and inhibition of T-cell mediated cytotoxicity due to IL-33-induced production of proteases by macrophages, that shed T-cell receptors and MHC Class 1 from T-cells and tumor cells respectively [5]. Furthermore, zebrafish patient-derived xenograft models have been established from non-muscle invasive urinary bladder cancer patients and was found to accurately recapitulate patient outcomes to the immune oncology therapy BCG [6].
Moreover, zebrafish xenograft assays are increasingly gaining attention as translational tools for personalized medicine, with growing evidence supporting their predictive value for patient outcomes across various cancer types [7–14]. For example, zebrafish patient-derived xenograft (PDX) models have been shown to rapidly and accurately predict carboplatin resistance and metastatic potential in epithelial ovarian cancer [7,8] within just three days of implantation. These models demonstrated high accuracy and strong concordance with actual patient outcomes. In another study, the zebrafish PDX model accurately predicts individual colorectal cancer patients’ responses of 55 patients to chemotherapy within days, enabling highly personalized and timely treatment decisions with up to 91% accuracy [9]. In addition, the predictive accuracy of the zebrafish PDX models for chemotherapy response has been validated in breast cancer, showing 100% concordance (18 out of 18 cases) with the actual responses of the corresponding patients [10].
Several clinical trials are now underway to assess the predictive validity of zebrafish PDX models across cancer types, including hepato-biliary-pancreatic cancers and gastro-intestinal cancers (NCT03668418), gastric cancer (NCT05616533), colon cancer (NCT06270017), and colorectal liver metastasis (NCT05289076). In these trials, patient tumors are injected into zebrafish larvae, followed by treatment with the same regimen as the patient. The zebrafish's therapeutic response is then compared to the clinical outcome. If successful, these trials could mark a paradigm shift in oncology by offering a rapid, cost-effective, and ethically sustainable alternative to traditional murine PDX models—particularly in situations where patient-derived material is scarce or time-sensitive decisions are needed.
Furthermore, zebrafish xenograft models have emerged as a powerful platform for in vivo drug screening [15,16]. Currently, compound administration is predominantly performed via water immersion, where drugs are dissolved directly into the embryo medium [17]. While this method is simple and scalable, it presents limitations in dose control, uptake variability, and poor solubility of hydrophobic compounds [18]. In this context, microinjection of compounds directly into the zebrafish larvae—for example, into the circulation, or perivitelline space—offers clear advantages. It enables controlled, reproducible dosing, immediate systemic availability, and the ability to deliver compounds with challenging physicochemical properties [18]. This approach is particularly valuable in xenograft studies, where accurate assessment of drug efficacy and toxicity doses is critical.
The throughput of such studies is, however, limited by the need for highly specialized lab personnel and time-consuming (double) injections in each larva. Some attempts have been made to orient and immobilize zebrafish larvae [19, 20] or to design robotic injection systems for yolk [21–23] or heart injections [24]. However, to the best of our knowledge, these approaches have not been thoroughly validated across a variety of biological samples in different laboratories, nor have they been made commercially available. In our recently published npj Biomedical Innovations study, we addressed the challenge of larval orientation by implementing automatic needle rotation based on larval positioning. Moreover, we standardized and automated injections into challenging sites, and validated the method with different cancer cell types and clinical samples across multiple laboratories, enabling such experiments to be performed without extensive training of technicians. Importantly, standardization of operations is key when operating in certified clinical laboratories where test results are used for patient diagnosis or treatment planning. Our automated microinjection system significantly contributes to this aspect by eliminating inter- and intra-operator variation, thereby improving reproducibility and quality of the test results. Indeed, the lack of standardization has been suggested to be a major barrier for implementation of zebrafish tumor xenograft models into clinical practice, an issue for which we are now presenting a solution. This opens the door for functional approaches to personalized medicine using patient-derived xenograft models in a real-time decision making process in the clinics.
Looking ahead, the automated injection platform has potential far beyond oncology. The automated injection system is also suited for operation within enclosed sterile environments such as biosafety cabinets, fume hoods, and biosafety level 3 (BSL-3) laboratories. Its compact design allows the injector module to fit into standard flow hoods, making it an excellent tool for applications that require strict aseptic conditions—such as germ-free studies or microbiota experiments. Manual injection setups are impractical in fume hood environments, as the procedure requires operators to maintain direct visual contact through a microscope, which is incompatible with the spatial constraints and protective barriers of a standard fume hood. These limitations are amplified in BSL-3 labs, where researchers work with high-risk pathogens such as SARS-CoV-2 or Zika virus, and where minimizing human exposure is a critical safety requirement [25]. The remote-control capability of the automated system offers an advantage in these settings: although larvae still need to be manually placed on and removed from the plate, researchers can monitor and operate the injection process from outside the containment area, thereby reducing physical exposure and risk.
The same platform could be adapted for use with one-cell stage zebrafish embryos to enable CRISPR delivery and facilitate gene therapy research. A dedicated robotic system for zebrafish egg injection already exists and has been applied across various applications [26–28]. While the adaptation of the larval injection system for early-stage embryos may not reach the same throughput as the egg-specific system (e.g., one embryo per second), it can offer the advantage of full autonomy. Moreover, integrating capabilities for both early-stage and late-stage embryo injections into a single multifunctional system provides added flexibility and value for researchers working across developmental timepoints. Furthermore, the underlying machine vision and injection technology is not limited to zebrafish, but also for microinjection in other model organisms, such as mosquitos, particularly Anopheles species, which are the natural vectors that transmit malaria, causing Plasmodium parasites to humans [29].
Naturally, the system is not without limitations. The most frequent challenge during microinjection, particularly with large substances such as cancer cells, is needle clogging, a problem that persists also with automation. Moreover, although the robot is capable of operating in a fully automated mode, it still requires operator involvement, including the placement and removal of zebrafish larvae, monitoring of the injection process, and attention to potential needle blockages. Finally, the price of an automated platform (2025 list price €130k) is much higher as compared to conventional manual injection setups. Nevertheless, these limitations are outweighed by the significant advantages of automated injection platforms—offering ease of use, precision, versatility, and scalability across models, developmental stages and species. These are precisely the attributes needed to meet the growing demand for reproducibility and throughput in both academic and translational research settings.
References
2. Xiao J, Glasgow E, Agarwal S. Zebrafish xenografts for drug discovery and personalized medicine. Trends in Cancer. 2020 Jul 1;6(7):569–79.
3. Ding Y, van der Kolk KJ, van der Ent W, Scotto di Mase M, Kowald S, Huizing J, et al. Automated microinjection for zebrafish xenograft models. NPJ Biomedical Innovations. 2025 Apr 23;2(1):13.
4. He X, Yin X, Wu J, Wickström SL, Duo Y, Du Q, et al. Visualization of human T lymphocyte-mediated eradication of cancer cells in vivo. Proceedings of the National Academy of Sciences. 2020 Sep 15;117(37):22910–9.
5. Wu J, Chen Z, Wickström SL, Gao J, He X, Jing X, et al. Interleukin‐33 is a novel immunosuppressor that protects cancer cells from TIL killing by a macrophage‐mediated shedding mechanism. Advanced Science. 2021 Nov;8(21):2101029.
6. Kowald S, Huge Y, Tandiono D, Ali Z, Vazquez-Rodriguez G, Erkstam A, et al. Novel zebrafish patient-derived tumor xenograft methodology for evaluating efficacy of immune-stimulating BCG therapy in urinary bladder cancer. Cells. 2023 Feb 3;12(3):508.
7. Lindahl G, Fjellander S, Selvaraj K, Vildeval M, Ali Z, Almter R, et al. Zebrafish tumour xenograft models: a prognostic approach to epithelial ovarian cancer. NPJ Precision Oncology. 2024 Feb 27;8(1):53.
8. Song F, Yi X, Zheng X, Zhang Z, Zhao L, Shen Y, et al. Zebrafish patient-derived xenograft system for predicting carboplatin resistance and metastasis of ovarian cancer. Drug Resistance Updates. 2025 Jan 1;78:101162.
9. Costa B, Estrada MF, Gomes A, Fernandez LM, Azevedo JM, Póvoa V, et al. Zebrafish Avatar-test forecasts clinical response to chemotherapy in patients with colorectal cancer. Nature Communications. 2024 Jun 5;15(1):4771.
10. Mendes RV, Ribeiro JM, Gouveia H, Rebelo de Almeida C, Castillo-Martin M, Brito MJ, et al. Zebrafish Avatar testing preclinical study predicts chemotherapy response in breast cancer. NPJ Precision Oncology. 2025 Apr 1;9(1):94.
11. Di Franco G, Usai A, Piccardi M, Cateni P, Palmeri M, Pollina LE, et al. Zebrafish patient-derived xenograft model to predict treatment outcomes of colorectal cancer patients. Biomedicines. 2022 Jun 22;10(7):1474.
12. Usai A, Di Franco G, Piccardi M, Cateni P, Pollina LE, Vivaldi C, et al. Zebrafish patient-derived xenografts identify chemo-response in pancreatic ductal adenocarcinoma patients. Cancers. 2021 Aug 17;13(16):4131.
13. Hua X, Wu X, Xu K, Zhan P, Liu H, Zhang F, et al. Zebrafish patient-derived xenografts accurately and quickly reproduce treatment outcomes in non–small cell lung cancer patients. Experimental Biology and Medicine. 2023 Feb;248(4):361–9.
14. Ali Z, Vildevall M, Rodriguez GV, Tandiono D, Vamvakaris I, Evangelou G, et al. Zebrafish patient-derived xenograft models predict lymph node involvement and treatment outcome in non-small cell lung cancer. Journal of Experimental & Clinical Cancer Research. 2022 Feb 9;41(1):58.
15. Xiao J, Glasgow E, Agarwal S. Zebrafish xenografts for drug discovery and personalized medicine. Trends in Cancer. 2020 Jul 1;6(7):569–79.
16. Haney MG, Moore LH, Blackburn JS. Drug screening of primary patient derived tumor xenografts in zebrafish. Journal of Visualized Experiments: JoVE. 2020 Apr 10(158):10–3791.
17. Dash SN, Patnaik L. Flight for fish in drug discovery: a review of zebrafish-based screening of molecules. Biology Letters. 2023 Aug 2;19(8):20220541.
18. Chaoul V, Dib EY, Bedran J, Khoury C, Shmoury O, Harb F, et al. Assessing drug administration techniques in zebrafish models of neurological disease. International Journal of Molecular Sciences. 2023 Oct 4;24(19):14898.
19. Zhang G, Tong M, Zhuang S, Yu X, Sun W, Lin W, et al. Zebrafish larva orientation and smooth aspiration control for microinjection. IEEE Transactions on Biomedical Engineering. 2020 Jun 4;68(1):47–55.
20. Ellett F, Irimia D. Microstructured devices for optimized microinjection and imaging of zebrafish larvae. Journal of Visualized Experiments: JoVE. 2017 Dec 8(130):56498.
21. Chi Z, Xu Q, Ai N, Ge W. Design and Development of an Automatic Microinjection System for High-Throughput Injection of Zebrafish Larvae. IEEE Transactions on Automation Science and Engineering. 2022;19:3409–18.
22. Guo Z, Ai N, Ge W, Xu Q. Design of an automated robotic microinjection system for batch injection of zebrafish embryos and larvae. Microsystems & Nanoengineering. 2024 Jan 29;10(1):20.
23. Guo X, Zhao A, Zhang Y, Jiang H, Tang L, Lu B, et al. Design and developing a robot-assisted cell batch microinjection system for zebrafish embryo. Microsystems & Nanoengineering. 2025 Feb 20;11(1):29.
24. Qian C, Yu X, Tong M, Zhuang S, Lin W. Visual-guided solutions in automated zebrafish larva heart micro-injection. IEEE Robotics and Automation Letters. 2022 Jan 4;7(2):1395–402.
25. Ragupathy V, Setty MK, Kostov Y, Ge X, Uplekar S, Hewlett I, et al. Non-invasive optical sensor based approaches for monitoring virus culture to minimize BSL3 laboratory entry. Sensors. 2015 Jun 24;15(7):14864–70.
26. Spaink HP, Cui C, Wiweger MI, Jansen HJ, Veneman WJ, Marín-Juez R, et al. Robotic injection of zebrafish embryos for high-throughput screening in disease models. Methods. 2013 Aug 15;62(3):246–54.
27. Habjan E, Ho VQ, Gallant J, Van Stempvoort G, Jim KK, Kuijl C, et al. An anti-tuberculosis compound screen using a zebrafish infection model identifies an aspartyl-tRNA synthetase inhibitor. Disease Models & Mechanisms. 2021 Dec 1;14(12):dmm049145.
28. Del Prado JA, Ding Y, Sonneville JD, Der Kolk KJ, Moreno-Mateos MA, Málaga-Trillo E, et al. Comparing robotic and manual injection methods in zebrafish embryos for high-throughput RNA silencing using CRISPR-RfxCas13d. Biotechniques. 2024 May 24;76(5):185–93.
29. Sato S. Plasmodium—a brief introduction to the parasites causing human malaria and their basic biology. Journal of Physiological Anthropology. 2021 Jan 7;40(1):1.