Abstract
Ogilvie syndrome, also known as “paralytic ileus of the colon,” is characterized by pseudo- obstruction of the colon without any component of mechanical obstruction; and presents as a massively distended abdomen. If left untreated, it carries a high risk of colonic perforation and ischemia leading to death. Ogilvie syndrome usually presents as a post-surgical complication, mainly due to the lack and/or restriction of movement coupled with a possible electrolyte imbalance. In this case, the patient was a non-surgical candidate who presented with a hip fracture after a mechanical fall. Three days post-fall, she developed nausea, abdominal discomfort, and constipation during her hospitalization, which gradually resulted in a massively distended abdomen. The patient was managed conservatively with a nasogastric tube, rectal tube decompression, Metoclopramide, and Magnesium Citrate administration. Abdominal X-rays showed massively dilated bowel loops. An abdominal CT scan showed diffuse dilation of the large bowel without a transition point, suggesting obstruction favoring colonic paralytic ileus. She was discharged to a rehabilitation facility for further physical therapy.
Keywords
Acute dilated colon, Megacolon, Paralytic ileus of colon, Colonic distention, Ogilvie syndrome, Acute colonic pseudo-obstruction
Introduction
Acute colonic pseudo-obstruction (Ogilvie syndrome) is characterized by acute dilatation of the colon without anatomical obstruction [1]. The eponym of this condition is named after the British surgeon, Sir William Heneage Ogilvie, who presented the first case in 1948 [1-12]. Acute colonic pseudo-obstruction usually occurs in hospitalized or nursing home patients in association with severe illness or following surgery in conjunction with a metabolic imbalance or administration of drugs that inhibit colonic motility [2,4]. The most common predisposing conditions are infections, post-surgical complications in patients who have undergone coronary artery bypass grafting, c-section pregnancies, and total joint replacements [2]. The exact pathogenesis of this condition is unknown. However, Ogilvie described it as a result of an imbalance of the enteric nervous system due to acute illness within the background of chronic disease [1-12].
In this case, we present a non-surgical candidate with Ogilvie syndrome who suffered a mechanical fall resulting in a non-displaced closed left hip fracture. The patient subsequently developed OS during the first three days of admission at our hospital. A multidisciplinary team treated the patient. We consulted orthopedic surgery, general surgery, and gastroenterology. A conservative treatment approach consisting of a nasogastric tube on low intermittent suction, a rectal tube, IV fluids, prokinetic agent, Metoclopramide, pain management, anticoagulation prophylaxis, and subsequently physical therapy was agreed upon.
Case Presentation
An 83-year-old Hispanic female with a past medical history of hypertension, diabetes mellitus type two, normal pressure hydrocephalus (dementia, ataxia, urinary incontinence, hydrocephalus), and constipation presented to the emergency department complaining of left leg pain after a mechanical fall. Her home medications included: Aspirin 81 mg, Donepezil (Aricept) 5 mg tab, Escitalopram oxalate (Lexapro) 10 mg, Glipizide (Glucotrol) 10 mg, Meclizine (Antivert) 12.5 mg, Mirabegron (Myrbetriq) 50 mg, and Nifedipine (Nifedipress) 60 mg. The leg pain was rated 7/10 in severity with no radiation. On physical examination, her left leg was externally rotated and abducted. The patient was unable to ambulate or bear weight on the affected extremity. A plain x-ray and CT scan of her pelvis revealed a left acetabular fracture involving the left iliac wing, acetabular wall, and ischiopubic ramus. Our Family Medicine team was consulted, and the decision to admit the patient under inpatient status to manage the pain and hip fracture further. Orthopedic surgery was consulted. Their recommendation was to provide rehabilitation services for physical therapy, occupational therapy, toe-touch weight- bearing, pain control, and follow-up in two weeks at the outpatient clinic.
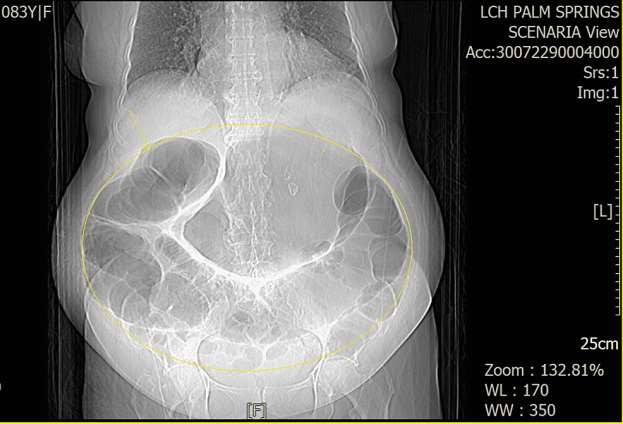
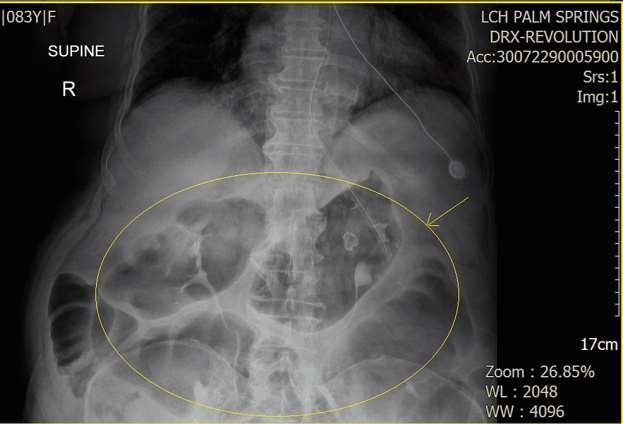
Three days after non-surgical management, the patient started developing abdominal discomfort, nausea, constipation, flatus, and abdominal distention. The abdomen was massively distended on physical examination, tympanic, and diminished bowel sounds. There was no fever or peritoneal signs of ischemia (e.g., guarding, rigidity, rebound tenderness). Laboratory workup revealed no thyroid problems or significant electrolyte abnormalities. An ultrasound of the abdomen was inconclusive due to the severity of the abdominal distention. A KUB showed a dilated stomach, large bowel loops suggesting an ileus pattern, and a demonstration of left acetabular fracture (Figure 1). CT of the abdomen showed diffuse dilation of the stomach and large bowel without transition point to suggest obstruction, favoring colonic ileus (Figure 2).
Figure 1. XR Abdomen KUB. Dilated stomach, loops of the small and large bowel, and demonstration of left acetabular fracture. XR: X-Ray; KUB: Kidney Ureter Bladder.
Figure 2. CT Abdomen Pelvis. Diffuse dilation of the stomach and large bowel without transition point to suggest obstruction. CT: Computerized Tomography.
Based on the clinical setting, risk factors, signs, symptoms, and imaging studies, the patient was diagnosed with Ogilvie syndrome after ruling out complete or partial obstruction, ileus, colonic volvulus, and gastroparesis. The patient’s prognosis was poor due to her inability to ambulate, age, neurological disorder, history of constipation, and severity of the case. The patient was carefully monitored with a series of physical exams, abdominal radiographs, and laboratory studies throughout her stay. Neostigmine being the first-line treatment was considered to aid in the patient’s gastric motility. However, due to the patient’s intermittent bouts of hypertension was treated with Labetalol 10 mg intravenous push every eight hours. We recognized that there was a contraindication between Neostigmine and labetalol due to the possibility of bradycardia. Therefore, pharmacological management with the second-line prokinetic agent was initiated. Treatment included Metoclopramide intravenous push every eight hours, intravenous fluids, Magnesium Citrate, and colonic decompression treatment with nasogastric tube placement at low intermittent suction. In addition, we excluded possible contributing factors by placing the patient on nothing by mouth and discontinuing calcium channel blockers and anticholinergic agents. The next day after minimal symptom resolution, a rectal tube was placed to aid drainage. After 12 hours, the patient had passed a significant amount of stool, and improvement was noted in the subsequent abdominal film (Figure 3). Due to large amounts of gastric content decompression, the patient experienced two episodes of asymptomatic hypokalemia on the third and fourth day of decompression that was subsequently repleted and corrected from a level of 3.0 to 4.0 with a dosage of 40 meq of Potassium Chloride intravenously and by mouth respectively. Complete resolution of symptoms and electrolyte imbalances took seven days. Consequently, the patient was discharged to a rehabilitation facility for her left hip fracture with a follow-up appointment with the orthopedic surgeon in two weeks.
Figure 3. Dilated loops of the large bowel slightly improved when compared to prior. Noted is the nasogastric tube placement with the distal tip and side port below the gastroesophageal junction.
Discussion
Acute colonic pseudo-obstruction, also known as Ogilvie syndrome, is characterized by massive dilation of the colon without mechanical obstruction [3]. This condition develops in hospitalized and bed-ridden patients in association with severe health conditions or after surgery in conjunction with a metabolic derangement or drugs that inhibit colonic motility [2]. Cesarean section and hip surgery are the most common surgical procedures associated with acute colonic pseudo-obstruction [2,5]. The pathophysiology is unknown. It is believed that interruption of the parasympathetic fibers from S2 to S4 leaves an atonic distal colon and a functional proximal obstruction [2,5].
The clinical presentation of OS occurs in elderly patients who have multiple medical conditions, as seen in this patient. Typically, it presents after trauma or as a complication of surgery [2,5]. Symptoms of abdominal pain, distention, nausea, and vomiting are common. On a physical exam, significant abdominal distention with tympany is evident. Also, bowel sounds may be absent. Acute colonic pseudo-obstruction can lead to bowel ischemia, colonic perforation, and death [3]. The risk of colonic perforation increases when the cecal diameter exceeds 10 to 12 cm and the distention has been present for more than six days [2]. The criterion for diagnosis is the diameter of the colon on abdominal films. However, there is no consensus regarding the minimum diameter required for the diagnosis [3]. The duration of abdominal dilation is more important than the diameter of the colon [6,7].
Recognition of this condition is critical to reducing the mortality rate as a result of colonic perforation. Ogilvie syndrome is managed by conservative medical therapy. Conservative management involves correcting electrolyte imbalances, discontinuing opiates, nasogastric tube decompression, and correcting fluid imbalances. Attempts to increase patient ambulation if possible also increase the success rate of conservative management. This effort should be continued for up to 48 to 72 hours as long as the patient is stable and has no peritoneal signs or diameter of bowel increase. This conservative approach has a success rate as high as 70% and an overall mortality rate of 14% [8]. In stable patients who did not improve with colonic decompression, medical therapy with cholinergic stimulation (Neostigmine) is recommended in a cardiac-monitored setting [8]. Also, pharmacologic agents such as Erythromycin, Cisapride, and Metoclopramide can aid by increasing colonic motility [10]. In patients treated with Neostigmine, the median time to response was four minutes, making Neostigmine superior to placebo [11]. The stimulation of the parasympathetic nervous system can cause profound bradycardia. As a result, when utilizing this treatment approach, Atropine must be available to counter its adverse effects. Neostigmine provided a 91% initial clinical response in a double-blinded study compared with a placebo [9].
In patients who are unresponsive to pharmacotherapy, the next step is to reduce colonic decompression with endoscopy. There is evidence that performing colonoscopic decompression before Neostigmine may shorten the length of stay [2]. This decompression technique applies to younger patients without cardiac disease. If conservative management, pharmacotherapy, and endoscopy fail to achieve resolution, then surgical procedures may be needed [4]. Overall, the best patient outcome is when we recognize OS in a timely manner and treat it with an anticholinesterase inhibitor such as Neostigmine. Clinical improvement after a prokinetic agent or Neostigmine supports the theory that pseudo-obstruction is caused by parasympathetic dysfunction.
Conclusions
Acute colonic pseudo-obstruction (Ogilvie syndrome) is a potentially unpleasant and even fatal pathophysiologic process. It is common in debilitated, hospitalized, and elderly patients with multiple comorbidities. OS typically affects post-surgical candidates. In this atypical case, a pre-surgical candidate also developed acute colonic pseudo-obstruction, prompting physicians to include this diagnosis in their differential. Conservative management is generally successful, and it is considered preferable over more invasive surgical therapies. When such measures fail, Neostigmine is the treatment of choice, and it has a high success rate when administered in a cardiac setting. When the patient has a contraindication to Neostigmine, other pharmacologic agents such as Erythromycin, Cisapride, and Metoclopramide can reduce the risk of peritonitis, colonic perforation, and mortality.
Authors’ Contributions
All authors participated in the management of this patient, conceived the idea of the case report, and participated in the drafting of the study.
Acknowledgment
Dr. Miguel Diaz, MD, Program Director & Faculty, Department of Family Medicine, Larkin Community Hospital Palm Springs Campus, for his amazing teaching that constantly inspires us to broaden our medical knowledge, as well as the patient for consenting to allow us to publish this report.
Competing Interests
All authors in this case report declare that they have no competing interests.
References
2. Chudzinski AP, Thompson EV, Ayscue JM. Acute colonic pseudoobstruction. Clinics in Colon and Rectal Surgery. 2015 Jun;28(2):112-7.
3. Tenofsky PL, Beamer RL, Smith RS. Ogilvie Syndrome as a Postoperative Complication: Archives of Surgery. 2000;135:682-687.
4. Johnson CD, Rice RP, Kelvin FM, Foster WL, Williford ME. The Radiologic Evaluation of Gross Cecal Distension: Emphasis on Cecal Ileus. AJR. American Journal of Roentgenology. 1985;145:1211- 1217. 10.2214/ajr.145.6.1211
5. Sloyer AF, Panella VS, Demas BE, Shike M, Lightdale CJ, Winawer SJ, Kurtz RC. Ogilvie's syndrome. Successful management without colonoscopy. Digestive Diseases and Sciences. 1988 Nov;33(11):1391-6.
6. De Giorgio R, Barbara G, Stanghellini V, Tonini M, Vasina V, Cola B, et al. Review article: the pharmacological treatment of acute colonic pseudo-obstruction. Alimentary Pharmacology & Therapeutics. 2001 Nov;15(11):1717-27.
7. Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for The Treatment of Acute Colonic Pseudo-Obstruction. New England Journal of Medicine. 1999;341:137-41.
8. Ogilvie H. Large-Intestine Colic due to Sympathetic Deprivation. British Medical Journal. 1948;2:671-3.
9. Khan MW, Ghauri SK, Shamim S. Ogilvie's Syndrome. Journal of the College of Physicians and Surgeons Pakistan. 2016;26:989-91.
10. Camilleri M. Acute colonic pseudo-obstruction (Ogilvie's syndrome). 2020. Accessed: https://www.uptodate.com/contents/acute-colonic-pseudo-obstruction-ogilvies-syndrome?search=acute-%20colonic-pseudo-obstruction-ogilvies-syndrome&source=search_result&selectedTitle=1~33&usage_type=default&display_rank=1
11. Intestinal Pseudo-Obstruction Treatment & Management. 2018. Accessed: 09/01/2021: https://emedicine.medscape.com/article/2162306-treatment
12. Gordon P, Nivatvongs S. The Principles and Practice of Surgery for the Colon, Rectum, and Anus. 3rd ed. New York: CRC Press; 2007.