Commentary
Anticentromere antibodies (ACA) are considered an important diagnostic marker of scleroderma or systemic sclerosis (SSc), being CENP-B the major centromere auto-antigen recognized by sera from SSc patients [1]. However, ACA can also be detected in patients with other connective tissue diseases [2]. Significantly the prevalence of organ-specific antibodies in SSc patients is relatively high [3]. Thus, primary biliary cirrhosis (PBC) is the most frequent autoimmune liver disease described in SSc patients and more often complicated specifically with limited cutaneous SSc (lcSSc) [4]. It is also well recognized that PBC is an overlapping condition between the autoimmune hepatology and rheumatology [5].
In PBC patients anti-mitochondrial auto-antibodies (AMA) are considered a hallmark of the disease and usually occurred in 80-95% of them [6]. In an original report, the AMA and ACA autoantibodies were demonstrated not presented any cross-reactivity between mitochondrial and centromere autoantigens [7]. Both AMA and ACA present discrete autoantibody populations which may coexist in the same patient, although the coexistence of primary biliary cirrhosis and systemic sclerosis is rare [8].
During past years, many studies have described the presence of PBC antibodies in SSc. Illustrative examples of recent studies are: in a large cohort of Italian patients with systemic sclerosis, PBC antibodies were detected in 20% of patients [9]. The prevalence of AMAs was higher in patients with lcSSc than in those with diffuse cutaneous SSc (dcSSc) and is strongly associated with the presence of ACAs. Interestingly, higher prevalence of both PBC-associated autoantibodies and PBC in the Japanese SSc population was found than in the Caucasian SSc population [10]. In a Belgian population, a wide range of PBC-Ab is detectable in SSc in the absence of cholestatic liver enzyme elevations [11]. Further, autoantibodies to Nt-CENPB in patients with scleroderma and AMA positive were found in a Spanish population [12], and a recent report in a Moroccan population, SSc patients with positive Nt-CENPB antibodies also showed reactivity against AMA-M2 antibodies [13]. Thus, the co - appearance of anti-centromere antibodies with others in SSc patients at different stages of disease may suggest some putative significance for the evaluation and development of this disorder [14].
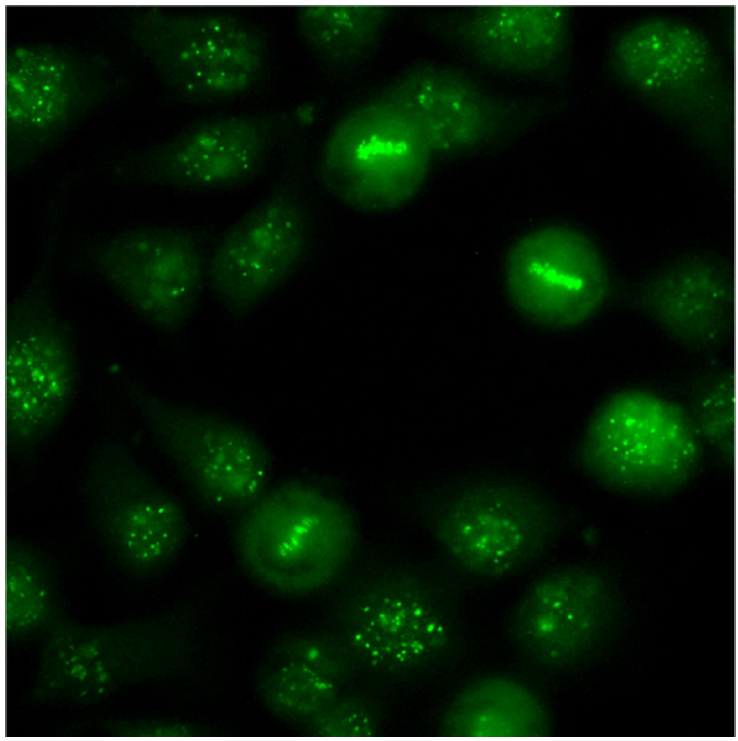
Although a significant number of reports in the bibliography suggest that SSc and PBC may have a common immunological or pathophysiological link it needs to be properly investigated [4-7,15]. Testing for autoantibodies against centromeric antigens (Figure 1) and the AMA may help to define the prognosis of both autoimmune disorders. Base for the balance of both types of autoantibodies, a distinct weight could be given to the anti-CENPB and anti-mitochondria specificities in the SS classification criteria and the development of PBC in SSc patients [16,17]. Besides all previous clinical evidences, it remains to be established if AMA could be a serological marker to suspect the occurrence and development of PBC disease in patients with scleroderma. In any case, a large cohort of systemic sclerosis and PBC patients should be studied to establish any significant immunological link between both autoimmune disorders.
Acknowledgements
I like to thank Plan Andaluz de Investigación, Junta de Andalucía for their support.
References
2. Mahler M, You D, Baron M, Taillefer SS, Hudson M, Canadian Scleroderma Research Group (CSRG); et al. Anti-centromere antibodies in a large cohort of systemic sclerosis patients: comparison between immunofluorescence, CENP-A and CENP-B ELISA. Clinica Chimica Acta. 2011 Oct 9;412(21-22):1937-43.
3. Wielosz E, Majdan M, Koszarny A, Dryglewska M, Tabarkiewicz J. Presence of organ-specific antibodies in patients with systemic sclerosis. Polskie Archiwum Medycyny Wewnetrznej. 2016 Oct 5;126(11):862-69.
4. Parveen S, Morshed SA, Nishioka M. High prevalence of antibodies to recombinant CENP-B in primary biliary cirrhosis: nuclear immunofluorescence patterns and ELISA reactivities. Journal of Gastroenterology and Hepatology. 1995 Jul-Aug;10(4):438-45.
5. Assassi S, Fritzler MJ, Arnett FC, Norman GL, Shah KR, Gourh P, et al. Primary biliary cirrhosis (PBC), PBC autoantibodies, and hepatic parameter abnormalities in a large population of systemic sclerosis patients. Journal of Rheumatology. 2009 Oct;36(10): 2250-56.
6. Ceribelli A, Isailovic N, De Santis M, Generali E, Satoh M, Selmi C. Detection of Anti-Mitochondrial Antibodies by Immunoprecipitation in Patients With Systemic Sclerosis. Journal of Immunological Methods. 2018 Jan;452:1-5.
7. Liberal R, Grant CR, Sakkas L, Bizzaro N, Bogdanos DP. Diagnostic and clinical significance of anti-centromere antibodies in primary biliary cirrhosis. Clinical and Research in Hepatology and Gastroenterology. 2013 Dec;37(6):572-85.
8. Whyte J, Hough D, Maddison PJ, McHugh NJ. The association of primary biliary cirrhosis and systemic sclerosis is not accounted for by cross reactivity between mitochondrial and centromere antigens. Journal of Autoimmunity. 1994 Jun;7(3):413-24.
9. Cavazzana I, Ceribelli A, Taraborelli M, Fredi M, Norman G, Tincani A, et al. Primary biliary cirrhosisrelated autoantibodies in a large cohort of italian patients with systemic sclerosis. Journal of Rheumatology. 2011 Oct;38(10):2180-85.
10. Imura-Kumada S, Hasegawa M, Matsushita T, Hamaguchi Y, Encabo S, Shums Z, et al. High prevalence of primary biliary cirrhosis and disease-associated autoantibodies in Japanese patients with systemic sclerosis. Modern Rheumatology. 2012 Nov;22(6):892-98.
11. Florin L, Rubben K, Vanhaecke A, Devreese K, De Keyser F, Smith V, et al. Evaluation of the primary biliary cholangitis-related serologic profile in a large cohort of Belgian systemic sclerosis patients. Clinical Chemistry and Laboratory Medicine. 2020 Feb 25;58(3):416-23.
12. Hamdouch K, Rodríguez C, Pérez-Venegas J, Rodríguez I, Astola A, Ortiz M, et al. Anti-CENPI autoantibodies in scleroderma patients with features of autoimmune liver diseases. Clinica Chimica Acta. 2011 Nov;412(23-24):2267-71.
13. Ziana Z, Bennani M, Hamdouch K, Maamarc M, Barakata A, Nouroutia NG, et al. Proteomics characterization of CENP-B epitope in Moroccan scleroderma patients with anti-centromere autoantibodies. Immunology Letters. 2020 May;221:1-5.
14. Liaskos C, Marou E, Simopoulou T, Gkoutzourelas A, Barmakoudi M, Efthymiou G, et al. Multiparametric Autoantibody Profiling of Patients With Systemic Sclerosis in Greece. Mediterranean Journal of Rheumatology 2018 Sep27;29(3):120-6.
15. Ohira H, Watanabe H. Pathophysiology and recent findings of primary biliary cirrhosis complicated by systemic sclerosis. Hepatology Research. 2014 Apr;44(4):377-83.
16. Hamaguchi, Y. Autoantibody profiles in systemic sclerosis: predictive value for clinical evaluation and prognosis. The Journal of Dermatology. 2010 Jan; 37(1):42-53.
17. Czaja AJ. Autoantibodies as prognostic markers in autoimmune liver disease. Digestive Diseases and Sciences. 2010 Aug;55(8):2144-61.