Abstract
A 30-year-old woman who wears scleral contact lenses for keratoconus was brought to the emergency room after a motor vehicle collision where a deployed airbag hit her left eye. The patient was taken to the operating room for globe exploration and found to have two large scleral lacerations (one superiorly and one temporally) with significant uveal prolapse. After primary repair, she developed a retinal detachment with proliferative vitreoretinopathy, vitreous hemorrhage and a full hyphema. She underwent a vitrectomy, retinal detachment repair and penetrating keratoplasty corneal transplant. We believe the extent of her trauma is due to a unique mechanism of injury in which the scleral lens acted like a punch, creating two scleral lacerations, and expulsing the ciliary body. To our knowledge, this is the first report of scleral lens induced open globe trauma.
Keywords
Scleral lens, Open globe, Scleral laceration
Introduction
The first contact lenses date back to 1888 and were reported by Adolf Eugen Fick [1]. They have proven beneficial for a number of different indications such as keratoconus, ocular surface disease, atopic keratoconjunctivitis, exposure keratopathy, and more [1]. Previous literature has detailed complications associated with wearing both soft and scleral contact lenses (SCL), but relatively little has been reported regarding cases of trauma while wearing SCL.
Motor vehicle crashes (MVC) are responsible for approximately 3.8 million emergency room visits annually in the US [2]. Not infrequently there can be ocular trauma sustained during the MVC from blunt, penetrating, or chemical injury. During airbag deployment, the cornea is the most frequently affected structure with injuries such as alkali burns, abrasions, and decompensation [3,4]. While these generally have good visual recovery, much more devastating injuries can occur. For instance, corneal lacerations and open globe injuries comprise up to 4.2% of airbag-related ocular injuries [3]. While both SCL use and ocular trauma are both relatively common, to the best of the authors’ knowledge, there has not been a report in the literature of a case of an open globe from a MVC while wearing a SCL. Detailed here is a case of an open globe injury sustained during an airbag deployment to an eye with a SCL.
Case Report
A 30-year-old woman presented to the emergency room after a MVC where she was the driver, and the car hit the center guardrail. The airbag deployed on impact, hitting her left eye; she reported that her vision immediately went black in that eye. The patient has a history of keratoconus for which she wears SCL in both eyes, which she was wearing at the time of the accident. Her vision was 20/25 in the right eye with her scleral lens present and light perception in the left eye with no scleral lens in place. Her extraocular movements were full, and she had an afferent pupillary defect by reverse. Measurement of intraocular pressure (IOP) was deferred given the concern for an open globe injury. The anterior segment exam was notable for superior hemorrhagic chemosis, superior scleral laceration, a flat anterior chamber, and a total hyphema. There was no view of the lens or posterior segment. A non-contrast CT scan of the orbits demonstrated an intraocular hematoma and ruptured globe.
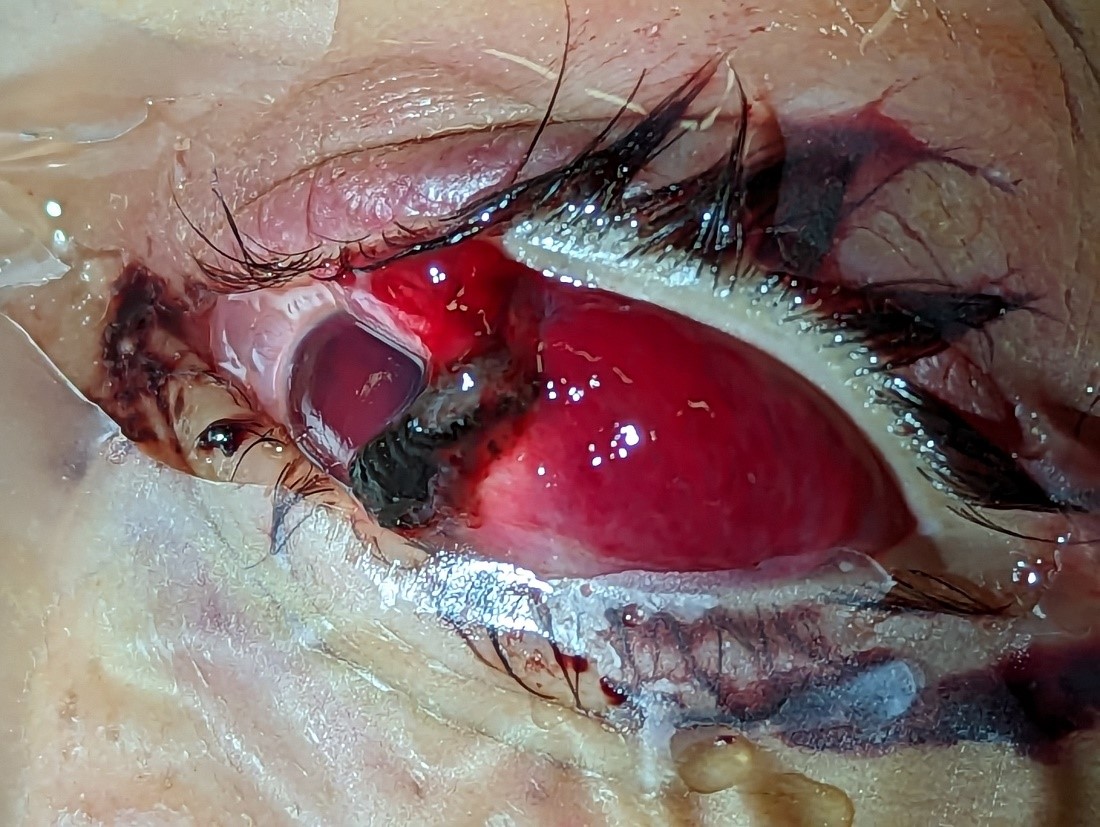
The patient was taken to the operating room for exploration and globe repair. The eye was noted to have 360° of subconjunctival hemorrhage, an 8-ball hyphema, and a scleral laceration approximately 3 mm superior to the limbus and extending 9 mm posteriorly (Figures 1 and 2). After further exploration, a second scleral laceration was located temporally and measured 8 mm. There was vitreous protruding from both lacerations as well as ciliary body, choroid, possibly retina and possibly iris. Primary closure of the globe was performed.
Figure 1. Intraoperative photograph taken of patient’s left eye (OS) demonstrating significant subconjunctival hemorrhage, total hyphema, and a scleral laceration approximately 3 mm superior to the limbus with uveal prolapse.
Figure 2. Intraoperative photograph taken of the patient’s left eye (OS) after a suture was placed in the superior tarsus to provide better exposure. Of note, there was 360° of subconjunctival hemorrhage, an 8-ball hyphema, and a scleral laceration approximately 3 mm superior to the limbus with uveal prolapse.
On post-op day 1, her vision remained light perception, and the intraocular pressure was 4 mm Hg. At follow up a few days later, a B-scan ultrasound showed vitreous hemorrhage and an attached retina. She developed proliferative vitreoretinopathy with a subsequent retinal detachment on repeat B-scan 3 weeks after the initial injury. This progressed to a repeat total hyphema with corneal blood staining. Her vision was barely light perception at this time, and the patient elected to pursue surgery with a penetrating keratoplasty corneal transplant, vitrectomy, and retinal detachment repair. Two months later, her vision was hand motion, and the patient decided to pursue further care in a state closer to her home.
Discussion
SCL use has been established as safe and effective for several corneal diseases [1]. Despite this, there is a paucity of literature regarding ocular trauma with concurrent SCL use. One case report describes a case of corneal perforation due to removal of a scleral lens in the setting of prior radial keratotomy [5]. Another documents an instance in which a scleral lens protected an eye from a projectile, possibly preventing an open globe injury [6]. In the case presented here, the patient sustained an open globe injury during a motor vehicle accident, and the severity of the open globe injury is believed to be attributable to the presence of a SCL at the time of impact. It is hypothesized that the force of the airbag’s impact on the scleral lens was distributed to induce the 2 lacerations given their size, location approximately 3 clock hours apart, and the absence of the SCL in the left eye. Additionally, it is hypothesized that the SCL acted like a punch causing the extent of expulsion of the ciliary body and uvea.
High IOP could theoretically contribute to expulsion of intraocular contents during an open globe injury, but there is conflicting data regarding the effect of the scleral contact lens and elevating IOP [7]. However, there is a documented phenomenon of “scleral cling,” wherein a scleral contact lens exerts a suction effect on the cornea [8]. This negative pressure is presumably what caused the corneal perforation in the setting of corneal thinning secondary to previous radial keratotomy [5], and it could have contributed to a more devastating injury in the setting of this airbag trauma. A review article by Wang et al. highlights that the anterior sclera has the highest rigidity and requires the greatest amount of force to penetrate [9]. The proximity of the patient’s lacerations to the limbus where the sclera is thickest and most durable potentially further implicates the SCL as this is close to where the edge of the SCL would rest. Given the patient’s history of keratoconus and corneal thinning, it is somewhat surprising that the patient did not sustain a corneal laceration from the trauma. This could be due to the distribution of the impact to the sclera as opposed to the cornea and possibly providing some protection for the cornea as was seen in the case of a SCL being struck with a projectile [6].
Conclusions
SCLs provide a known benefit for a variety of ophthalmic conditions while maintaining a relatively low risk profile. However, there has been little published on the SCL in the setting of blunt ocular trauma. Based on the case described above, it is believed by the authors that in the extreme case of significant blunt ocular trauma, the rigid SCL may play a role in distributing the force to the sclera and potentially acting as a punch causing further expulsion of uveal tissues and exacerbating an already severe injury.
Conflicts of Interest
The authors attest that they have no conflicts of interest in the presented case.
Funding Statement
No funding was required or obtained for the production of this manuscript.
Acknowledgements
No further acknowledgements.
Author Contribution Statement
MK Wilson and CR Blake performed the primary surgery; CR Blake proposed the original idea that the SCL exacerbated the severity of the injury. JK Hu proposed the mechanism that the SCL acted as a punch, inducing the lacerations and causing expulsion of intraocular contents. MK Wilson and LP Bowman wrote and edited the manuscript. All authors reviewed, discussed, and agreed upon the final manuscript.
References
2. Davis D, Cairns C. Emergency Department Visit Rates for Motor Vehicle Crashes by Selected Characteristics: United States, 2019-2020. NCHS Data Brief. 2023;(466):1-8.
3. Ball DC, Bouchard CS. Ocular morbidity associated with airbag deployment: a report of seven cases and a review of the literature. Cornea. 2001;20(2):159-63.
4. Pearlman JA, Au Eong KG, Kuhn F, Pieramici DJ. Airbags and eye injuries: epidemiology, spectrum of injury, and analysis of risk factors. Surv Ophthalmol. 2001;46(3):234-42.
5. Weber SP, Jorge BCM, Mourão ABG, Hofling-Lima AL. Late Spontaneous Postradial Keratotomy Corneal Perforation After Scleral Contact Lens Use-Case Report. Eye Contact Lens. 2022;48(12):534-36.
6. Ritzmann M. Blunt trauma with scleral lens [Internet]. Global Insight; 2020 Mar 31 [cited 2023 Oct 10]. Available from:
7. https://www.contamac-globalinsight.com/case-reports/blunt-trauma-scleral-lens/
8. Schornack MM, Vincent SJ, Walker MK. Anatomical and physiological considerations in scleral lens wear: Intraocular pressure. Cont Lens Anterior Eye. 2023;46(1):101535.
9. Miller D, Carroll JM, Holmberg A. Scleral lens cling measurement. Am J Ophthalmol.1968;65:929-30.
10. Wang S, Li F, Jin S, Zhang Y, Yang N, Zhao J. Biomechanics of open-globe injury: a review. Biomed Eng Online. 2023;22(1):53.