Abstract
Metastatic malignant melanoma of the small bowel is a rare and aggressive disease, without specific symptoms. Due to that, most cases are diagnosed in advanced stages, presenting as an acute abdomen in situations of bowel obstruct ion or perforation.
We present the case of a 56-year-old male who was admitted for generalized edema and developed an acute abdomen secondary to perforation of small bowel malignant melanoma metastasis, with lymph node invasion. Segmental bowel resection was performed with peritoneal lavage. The patient developed another metastasis perforation in the first postoperative week and was later transferred to a palliative care institution. Tumor perforation is a very rare presentation of small bowel metastatic melanoma, being a condition with a difficult diagnosis and poor outcome.
Introduction
Primary tumors of the small bowel are a rare condition, accounting for 2 to 3% of gastrointestinal tumors. Malignant melanoma is the most common metastatic tumor found in the gastrointestinal tract [1]. It can be localized in different sites, from the oral cavity to the anus. It can also be present as a primary lesion.
Malignant melanoma of the small bowel is often asymptomatic. Most common symptoms are non-specific, such as chronic abdominal pain, intestinal bleeding, weight loss, vomiting, and intestinal obstruction. In very rare cases, the initial presentation can be as a perforation [2-4].
The authors present a clinical case of a very rare cause of acute abdomen, secondary to perforation of malignant melanoma small bowel metastasis.
Case Report
A 56-year-old Caucasian male presented to the emergency department with complaints of abdominal discomfort, bilateral edema of the lower limbs and scrotum for the past two days. The patient had heavy alcoholic habits, a history of excision of malignant melanoma of the right ear 5 years earlier, without follow-up, and a craniotomy in the sequence of a subdural hematoma following head trauma.
At the admission, the patient was hemodynamically stable and apyretic. Physical examination revealed marked lymphedema of the scrotum and lower limbs, and a soft, non-tender abdomen.
Laboratory tests revealed anemia (7 g/dL-normal: 13.5- 17.5 g/dL), normal white blood count, low albumin levels (1.6 g/dL-normal: >3.5 g/dL) and elevated C reactive protein (10.1 mg/dL-normal: <0.5 mg/dL). The abdomen ultrasound showed free fluid in hepatic and splenic spaces. Empirical broad-spectrum antibiotic therapy was started, and it was given one unit of red blood cell concentrate. The patient was admitted in the Internal Medicine ward for further studies.
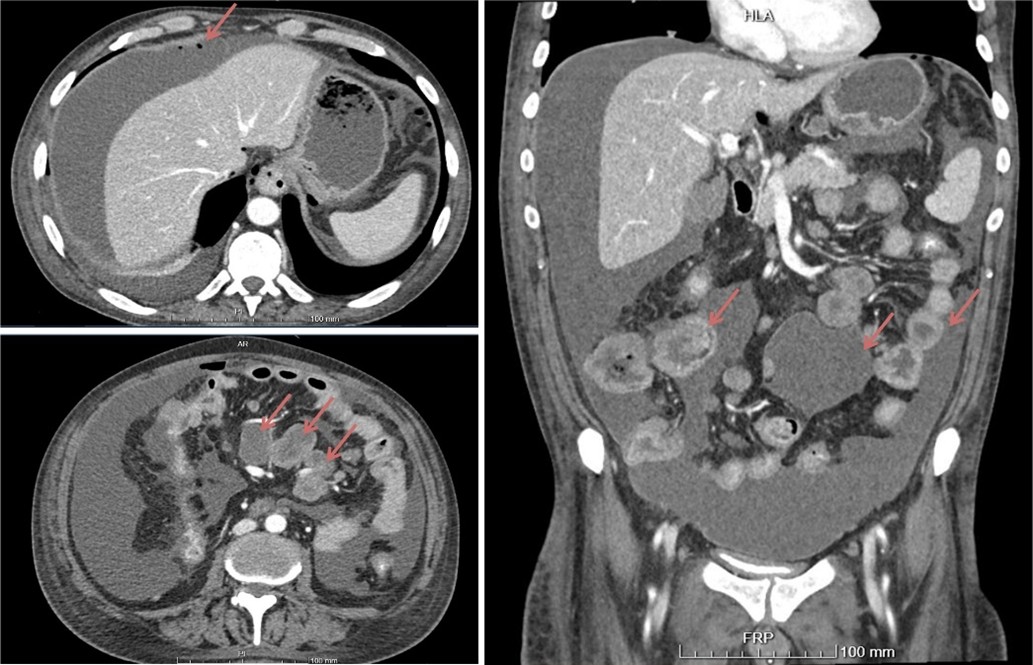
In the fifth day of hospitalization, the patient presented with sudden generalized abdominal pain. Physical examination revealed diffuse abdominal pain with tenderness and rebound pain. Chest X-Ray showed pneumoperitoneum. Due to the patient’s hemodynamic stability, he underwent an abdominal CT, which showed massive peritoneal effusion in all quadrants, pneumoperitoneum, diffuse parietal thickening of part of jejunum and ileum, with some air bubbles in this area (compatible with bowel perforation) and multiple nodes in the lesser sac and in the mesentery, the largest with 4 cm (Figure 1).
Figure 1. Abdomen CT showing free peritoneal fluid, bubbles of pneumoperitoneum, multiple lymph nodes in the retroperitoneum and thickening of the small bowel.
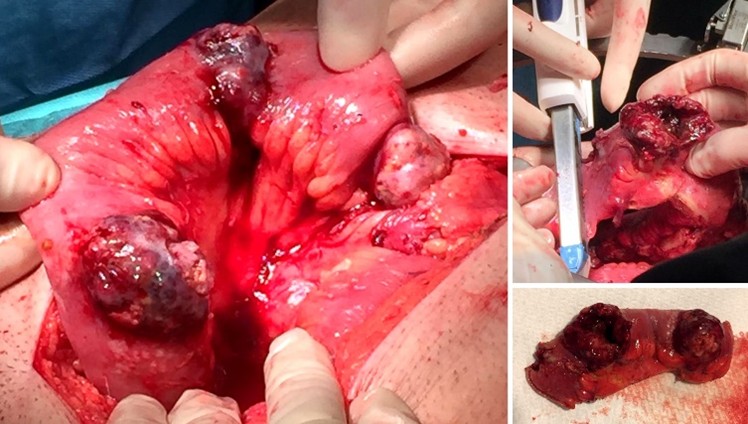
An exploratory laparotomy was performed, revealing purulent peritoneal effusion (3.5 liters) and multiple pigmented exofitic lesions in the small bowel, two of them perforated. Multiple lymph nodes conglomerates were present in the mesentery. Segmental bowel resection was performed with anisoperistaltic mechanical anastomosis and peritoneal lavage (Figure 2). A multitubular drain was left in the pelvic space.
Figure 2. Segmental enterectomy with mechanical anastomosis.
In the third postoperative day, there was drainage of fecal content through the drain. The patient was taken to the operating room, where another perforated metastatic lesion was identified; the previous anastomosis did not have signs of leakage. Due to the impossibility of surgical resection or curative procedures and the bad prognostic outcome, a jejunostomy with a Pezzer catheter and peritoneal lavage were performed. On the fifth postoperative day, the patient was transferred to a palliative care institution, and died a week later.
The histological exam confirmed the presence of small bowel metastatic malignant melanoma, and six of seven lymph nodes with metastasis.
Discussion
The digestive malignant melanoma represents an aggressive tumor, often with delayed diagnosis as an emergency presentation, due to its non-specific symptoms. The small bowel represents the preferential site of skin malignant melanoma metastases [2-4]. Through both the lymphatic and hematogenous pathways, malignant melanoma can also metastasize to the liver, colon, stomach, lungs, bone and brain.
When melanoma spreads to the small bowel, it generally appears in multiple localized lesions. Due to that, the tumors usually grow to a considerable size before the patient develops any symptoms. Berger’ et al. demonstrated that when there are digestive metastases of melanoma, the incidence of multiple lesions is 90% [5-12].
Tumor perforation represents a very rare presentation of this condition, with high risk of postoperative mortality. A limited number of cases of small bowel perforation secondary to metastatic melanoma have been described so far in literature [8-15].
The diagnosis of this condition is difficult, and in several cases, it is only done by exploratory laparotomy. Small bowel metastatic melanoma should be considered in the differential diagnosis in a patient with an acute abdomen and with previous history of skin melanoma.
Imaging exams that can help in the diagnosis are capsule endoscopy, CT scan, magnetic resonance imaging, and positron emission tomography. The definitive diagnosis can be made after histological evaluation.
Surgery must be offered whenever possible, even for metastatic lesions. Segmental enterectomy remains the method that gives the best palliation. In cases of obstruction, hemorrhage or perforation, as in this case, emergency surgery is mandatory [8-15]. Intestinal malignant melanoma carries a poor prognosis, with high recurrence, and a median survival of 4 to 6 months [3].
Author’s Contribution Statement
FA collected the data, performed the literature search and wrote the manuscript. CC and AR collected the data and reviewed the manuscript. MM and JGT reviewed the final version of the manuscript.
References
2. Blecker D, Abraham S, Furth EE, Kochman ML. Melanoma in the gastrointestinal tract. The American journal of gastroenterology. 1999 Dec 1;94(12):3427-33.
3. Wysocki WM, Komorowski AL, Darasz Z.Gastrointestinal metastases from malignant melanoma: report of a case. Surgery today. 2004 Jun 1;34(6):542-6.
4. Gutman H, Hess KR, Kokotsakis JA, Ross MI, Guinee VF, Balch CM. Surgery for abdominal metastases of cutaneous melanoma. World journal of surgery. 2001 Jun 1;25(6):750-8.
5. Berger AC, Buell JF, Venzon D, Baker AR, Libutti SK. Management of symptomatic malignant melanoma of the gastrointestinal tract. Annals of surgical oncology. 1999 Mar 1;6(2):155-60.
6. Lens M, Bataille V, Krivokapic Z. Melanoma of the small intestine. The lancet oncology. 2009 May 1;10(5):516-21.
7. Vilcea ID, Vasile I, Vîlcea AM, Mirea CS, Popescu CF, Mitrut P. Intestinal perforated malignant melanoma: diagnostic and therapeutic difficulties. Chirurgia (Bucur). 2012 Jul 1;107(4):529-33.
8. Chao TC, Chao HH, Jan YY, Chen MF. Perforation through small bowel malignant tumors. Journal of gastrointestinal surgery. 2005 Mar 1;9(3):430.
9. Liang KV, Sanderson SO, Nowakowski GS, Arora AS. Metastatic malignant melanoma of the gastrointestinal tract. InMayo Clinic Proceedings 2006 Apr 1 (Vol. 81, No. 4, pp. 511-516). Elsevier.
10. Gupta TD, BRASFIELD RD. Metastatic melanoma of the gastrointestinal tract. Archives of Surgery. 1964 Jun 1;88(6):969-73.
11. Ollila DW, Essner R, Wanek LA, Morton DL.Surgical resection for melanoma metastatic to the gastrointestinal tract. Archives of surgery. 1996 Sep 1;131(9):975-80.
12. Schuchter LM, Green R, Fraker D. Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Current opinion in oncology. 2000 Mar 1;12(2):181-5.
13. Patti R, Cacciatori M, Guercio G, Territo V, Di Vita G. Intestinal melanoma: a broad spectrum of clinical presentation. International journal of surgery case reports. 2012 Jan 1;3(8):395-8.
14. Spiridakis KG, Polichronaki EE, Sfakianakis EE, Flamourakis ME, Margetousakis TH, Xekalou AS, Lianeris GK, Giannikaki ES, Christodoulakis MS. Primary small bowel melanoma. A case report and a review of the literature. Il Giornale di chirurgia. 2015 May;36(3):128.
15. Gill SS, Heuman DM, Mihas AA. Small intestinal neoplasms. Journal of Clinical Gastroenterology 2001;33:267-82.