Abstract
Early dropout from psychiatric care remains a persistent barrier to effective treatment. To investigate the role of therapeutic alliance and financial burden in contemporary treatment settings, we conducted a retrospective analysis using data from a large national telepsychiatry platform. The study included 796 adults (≥18 years) who completed at least two visits and had working alliance inventory-short revised (WAI-SR) scores within 45 days of their initial appointment. First-visit deductible and copay amounts were defined as financial obligation. Cut-point analyses identified a WAI-SR total score of 50 as the threshold for high vs. low alliance and $40 USD as the threshold for financial obligation. Multivariable logistic regression models, adjusted for age, sex, primary diagnosis, insurance type, generalized anxiety disorder 7-item scale (GAD-7), patient health questionnaire 8-item depression scale (PHQ-8), and timely prescription issuance (within 7 days), estimated the likelihood of early dropout. In fully adjusted models, low alliance (Adjusted odds ratio [aOR]=2.58, 95% confidence interval [CI]: 1.48–4.51) and higher financial obligation (aOR=2.01, 95% CI: 1.14–3.56) were the strongest indicators of dropout. Higher PHQ-8 scores were also associated with increased dropout risk (aOR=1.07, 95% CI: 1.00–1.13). Findings were consistent across secondary analyses, highlighting the central role of therapeutic alliance and financial burden in shaping dropout patterns in real-world tele psychiatric care.
Keywords
Telepsychiatry, Treatment dropout, Therapeutic alliance, Financial burden, Anxiety, Depression, Telehealth
Introduction
Recent years have seen steady increases in mental health care utilization [1,2], which have been fueled in part by the expansion of telehealth services [3]. However, despite increased uptake, early dropout from care remains a persistent challenge. Large-scale studies report between 20% and 30% of individuals who initiate outpatient mental health treatment discontinue care after just one or two visits [4,5]. Early treatment dropout is associated with worse clinical outcomes, including higher rates of symptom persistence, relapse, and increased healthcare utilization compared to patients who remain engaged in care [6–8].
Therapeutic alliance and financial burden have been highlighted as key predictors of patient dropout [9–11]. Patients reporting stronger therapeutic alliance are more likely to experience symptom improvement and are less likely to discontinue treatment across a wide range of mental health disorders, including depression, anxiety, borderline personality, and substance use disorders [12–15]. The protective effect of therapeutic alliance has also been replicated in online therapy programs [16]. Given that majority of therapeutic alliance studies focus on patients receiving care in clinical psychology settings, questions remain as to whether these patterns apply to the field of psychiatry as well. Additionally, the advent of telehealth as an accessible treatment option warrants further investigation into the causes of dropout within the telepsychiatry digital space.
Socioeconomic factors have long been barriers to mental healthcare access, with lower-income individuals reporting greater challenges in receiving care and, in turn, higher rates of dropout [9,17,18]. A large-scale study (N=58,162), conducted using data from a behavioral health technology platform, found that clients who paid higher out-of-pocket fees at their first therapy session were significantly more likely to drop out early of treatment [19]. However, despite consistent evidence that financial obligation contributes to discontinuation, no clear cost thresholds have been established to indicate when treatment becomes unsustainable. The broader dropout literature shows mixed evidence regarding associations between discontinuation and patient characteristics such as illness severity, age, and gender [20,21]. This inconsistency highlights the complexity of dropout and suggests that its predictors may vary across populations, settings, and study designs.
To advance the understanding of dropout in contemporary psychiatric treatment settings, we analyzed data from a large national tele psychiatric practice. We evaluated factors that impact the likelihood of early dropout, with particular emphasis on therapeutic alliance and financial obligation. We further explored potential cut points for these measures. By addressing these gaps, our study aimed to provide new insights into how clinicians and systems can better identify patients at risk of early psychiatric treatment discontinuation.
Methods
Data collection
The following retrospective study analyzed anonymized clinical data extracted from the electronic health records of adults who initiated psychiatric care through a national outpatient telepsychiatry platform. All aspects of care, including initial evaluations, medication prescribing, therapy, and symptom monitoring were delivered remotely by licensed psychiatrists using a unified digital platform. This study was reviewed and granted exempt status by the institutional review board of Advarra (Pro00084942). A waiver of Health Insurance Portability and Accountability Act (HIPAA) authorization was granted under an expedited review process.
Upon initiating care, patients completed an online intake process that included a brief screening form and the opportunity to choose a psychiatrist based on clinician profiles that included clinical focus areas, availability, and biographical information. After selecting a psychiatrist, patients scheduled their first appointment. The first appointment consisted of a comprehensive psychiatric evaluation conducted via a secure, HIPAA-compliant video platform. Patient deductible and copay amounts were obtained from internal billing data and used to compute first visit financial obligation. The initial session was then followed by ongoing care, which included supportive psychotherapy and medication management delivered in 20–30-minute virtual follow-up visits.
Patients were prompted to complete standardized symptom assessments of depression (Patient health questionnaire 8-item depression scale [PHQ-8]) and anxiety (Generalized anxiety disorder 7-item scale [GAD-7]) seven days before their initial visit, as part of routine clinical documentation. After completing their second visit, all patients aged 18 and older were asked to complete the working alliance inventory-short revised (WAI-SR) [22, 23]. The WAI-SR is a 12-item instrument that evaluates the patient’s rating of their therapeutic alliance with their psychiatrist based on shared goals, tasks, and interpersonal bonds. The WAI-SR total score, which is calculated as the sum of all items, ranges from 12–60, with higher values indicating higher therapeutic alliance. We made minor adaptations to the instrument, replacing the word ‘therapist’ with ‘psychiatrist’ and replacing the word ‘therapy’ with ‘treatment’ to more accurately describe the care being provided.
The final study sample was composed of patients who: (1) completed at least two psychiatry sessions within the study time frame, (2) were at least 18 years of age, and (3) completed a WAI-SR questionnaire no more than 45 days after their first visit. Patients who completed the WAI-SR more than 45 days after their first visit were excluded to mitigate a potential survival bias. We defined early dropout as a patient who satisfied two criteria: (1) No completed or scheduled visits at least 90 days after their second visit, and (2) Had a recorded psychiatrist-confirmed treatment discharge due to non-adherence or patient decision. The study’s timeframe was restricted to patients who completed their second psychiatric evaluation between August 14, 2024, and April 14, 2025. Data collection completed on July 3, 2025.
Statistics
We fit multivariable logistic regression models and report unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CIs) to estimate the likelihood of early dropout as a function of total therapeutic alliance and first visit financial obligation. The primary model used binary classifications of WAI-SR total score and financial obligation, based on empirically derived thresholds identified using the cutpointr package in R (v1.2.1) [13]. Optimal cut points were selected by maximizing Youden’s J statistic (J=sensitivity + specificity – 1), which balances sensitivity and specificity to identify the most discriminative thresholds. To quantify uncertainty and produce 95% CIs for cut point estimates, we performed 1,000 in-bag bootstrap runs. Models were also adjusted for age, sex, primary diagnosis (anxiety, depression, attention-deficit/hyperactivity disorder [ADHD], and Other), US Region (Midwest, Northeast, South, or West), insurance type (commercial or non-commercial), GAD-7, PHQ-8, and whether a timely prescription was issued (within 7 days of first visit). Supplementary analyses report estimates using continuous variables for WAI-SR subscales and total score. We further investigated whether having any financial obligation at the initial visit was associated with an increased likelihood of early dropout compared to those with zero out-of-pocket costs.
GAD-7 and PHQ-8 scores were missing for 29.4% of patients, and financial obligation data was missing for 10 individuals, resulting in a notable reduction in sample size in our primary analyses. We examined the association between missing symptom severity data and study variables and found no significant patterns, supporting the assumption that data were missing at random (Supplementary Table 1). Accordingly, for our secondary analyses, we used the mice (v3.18.0) package in R to apply multiple imputation by chained equations (MICE) to address missing values and assess whether the missingness in our primary dataset created biases within our analysis. The MICE algorithm iteratively predicts missing data for each variable based on the others, generating multiple complete datasets to account for uncertainty in the imputed values. Results from these datasets are then pooled to produce overall estimates and standard errors that incorporate imputation variability. Multiple imputation is a well-established approach for addressing missing data and has been shown to reduce statistical bias even when a large proportion of data is missing [24]. All variables included in the primary analysis were used in the imputation model. The data set was imputed five times, and final estimates were derived using Rubin’s rules to combine results across imputations. We then re-ran the primary analysis on the imputed datasets. All analyses were conducted using statistical software R version 4.1.1.
Results
We identified 796 patients who met our inclusion criteria (females: 75.4%, mean (standard deviation [SD]) age: 45.1 (14.2) years). 105 patients were early dropouts, giving us an early dropout rate of 13.2%. The mean interval between the first visit and WAI-SR completion was 24.6 days (SD=8.9), with an average WAI-SR total score of 52.1 (SD=9.8) and excellent internal consistency (Cronbach’s α=0.96). The distribution of WAI-SR subscales and total scores are visualized in Figure 1. Our median patient obligation was $25 (Interquartile Range [IQR]=$0–$50), with 30.9% of patients having no financial obligation.
Figure 1. Distribution of Working Alliance Inventory-Short Revised (WAI-SR) total score and subscales.
Our cut point analysis determined a WAI-SR total score of 50 (95% CI: 41–50) to be the optimal threshold to divide our “low” and “high” alliance categories. 26.9% of patients were classified in the low alliance category (Dropouts: 47.6%; Non-dropouts: 23.7%). Using the same cut point methodology, financial obligation was divided into patients with first visit payments less than forty dollars (95% CI: $20–$375) and those with payments of over 40 dollars. In our overall sample, 31.2% of patients were in the higher financial obligation category (Dropouts: 45.2%; Non-Dropouts: 29.0%). The comparative demographic and clinical characteristics of the early dropout and non-dropout groups are presented in Table 1.
|
|
Dropout |
Non-Dropout |
|
Female |
82 (78.1%) |
518 (75.0%) |
|
Age |
45.5 (13.90) |
45.0 (14.26) |
|
Commercial Insurance |
83 (79.0%) |
569 (82.3%) |
|
Region |
||
|
South |
42 (40.0%) |
287 (41.5%) |
|
Northeast |
31 (29.5%) |
212 (30.7%) |
|
Midwest |
14 (13.3%) |
108 (15.6%) |
|
West |
18 (17.1%) |
84 (12.2%) |
|
First Visit Patient Obligation ($) |
30.00 (10.00, 112.00) |
25.0 (0.00, 50.00) |
|
No Patient Obligation |
23 (22.1%) |
220 (32.3%) |
|
40+ Patient Obligation |
47 (45.2%) |
198 (29.0%) |
|
Diagnosis |
||
|
Depression |
30 (28.6%) |
201 (29.1%) |
|
Anxiety |
36 (34.3%) |
223 (32.3%) |
|
ADHD |
13 (12.4%) |
145 (21.0%) |
|
Other |
26 (24.8%) |
122 (17.7%) |
|
Timely Prescription Issued |
65 (61.9%) |
524 (75.8%) |
|
WAI-SR Bond |
16.0 (4.72) |
18.1 (2.89) |
|
WAI-SR Task |
14.3 (5.17) |
16.7 (3.36) |
|
WAI-SR Goal |
15.8 (5.17) |
18.2 (2.93) |
|
WAI-SR Total |
46.2 (14.51) |
53.0 (8.48) |
|
Low Alliance Category |
50 (47.6%) |
164 (23.7%) |
|
PHQ-8 |
13.5 (5.46) |
10.9 (5.77) |
|
GAD-7 |
11.9 (5.35) |
10.3 (5.15) |
|
Abbreviations: WAI-SR: Working Alliance Inventory-Short Revised; PHQ-8: Patient Health Questionnaire-8; GAD-7: Generalized Anxiety Disorder-7. an (%); Mean (SD); Median (Q1, Q3). |
||
In our univariate analysis (Table 2), patients in the low alliance group and those with higher financial obligations were more likely to drop out of psychiatric care. Higher PHQ-8 and GAD-7 scores were also associated with higher dropout likelihood, and patients with prescriptions issued within 7 days of their first visit had lower rates of dropout than patients who did not. Neither primary diagnostic group nor any other measured covariates were independently associated with early dropout.
|
|
OR - Primary |
aOR - Primary |
OR - Imputed |
aOR - Imputed |
|
Sex: Male¹ |
0.84 (0.5, 1.35); |
0.87 (0.43, 1.69); |
0.84 (0.51, 1.38); |
0.9 (0.53, 1.55); |
|
Age |
1 (0.99, 1.02); |
1.01 (0.98, 1.03); |
1 (0.99, 1.02); |
1.01 (0.99, 1.03); |
|
Commercial Insurance² |
0.81 (0.49, 1.37); |
0.72 (0.34, 1.59); |
0.81 (0.49, 1.35); |
0.86 (0.47, 1.58); |
|
Region: Northeast³ |
1 (0.6, 1.64); |
0.74 (0.37, 1.45); |
1 (0.61, 1.64); |
0.94 (0.55, 1.61); |
|
Region: Midwest³ |
0.89 (0.45, 1.65); |
1.01 (0.43, 2.2); |
0.89 (0.46, 1.69); |
0.9 (0.46, 1.79); |
|
Region: West³ |
1.46 (0.79, 2.64); |
1.4 (0.59, 3.13); |
1.46 (0.8, 2.68); |
1.83 (0.96, 3.51); |
|
$40+ Patient Obligation4 |
2.02 (1.32, 3.07); |
2.01 (1.14, 3.56); |
2.03 (1.33, 3.09); |
2.3 (1.45, 3.66); |
|
Diagnosis: Anxiety5 |
1.08 (0.64, 1.83); |
1.03 (0.52, 2.06); |
1.08 (0.64, 1.82); |
1.39 (0.78, 2.48); |
|
Diagnosis: ADHD5 |
0.6 (0.29, 1.17); |
0.72 (0.28, 1.72); |
0.6 (0.3, 1.19); |
0.96 (0.46, 2.03); |
|
Diagnosis: Other5 |
1.43 (0.8, 2.53); |
1.03 (0.46, 2.24); |
1.43 (0.81, 2.53); |
1.8 (0.96, 3.38); |
|
Timely Prescription Issued6 |
0.52 (0.34, 0.8); |
0.55 (0.3, 1.01); |
0.52 (0.34, 0.8); |
0.49 (0.31, 0.8); |
|
Low Alliance7 |
2.92 (1.91, 4.45); |
2.58 (1.48, 4.51); |
2.92 (1.92, 4.45); |
2.65 (1.7, 4.13); |
|
PHQ8 |
1.08 (1.03, 1.13); |
1.07 (1, 1.13); |
1.09 (1.04, 1.14); |
1.08 (1.01, 1.15); |
|
GAD7 |
1.06 (1.01, 1.12); |
1.01 (0.95, 1.08); |
1.06 (1.01, 1.11); |
1.01 (0.94, 1.07); |
|
Abbreviations: WAI-SR: Working Alliance Inventory-Short Revised; PHQ-8: Patient Health Questionnaire-8; GAD-7: Generalized Anxiety Disorder-7. 1Compared to female, 2Compared to non-commercial, 3Compared to South, 4Compared to <$40 patient obligation, 5Compared to depression, 6Compared to no prescription issued within 7 days of first visit, 7Compared to high alliance (WAI-SR total >50). |
||||
All patients with missing values were excluded from the multivariate analysis, bringing the total sample size in the complete-case analysis to 554 patients, with a 12.9% dropout rate (65 patients). Model fit indices for the fully adjusted model indicated modest explanatory power (McFadden R²=0.093; Nagelkerke R²=0.126). The model fit significantly better than the null (G²=37.28). Low alliance and higher financial burden remained significantly associated with increased odds of dropout. After adjusting for covariates, GAD-7 was no longer a significant measure of dropout, while PHQ-8 remained marginally significant. Timely prescription issuance trended towards significance after covariate-adjustment but did not reach the significance threshold. All other variables were not significant.
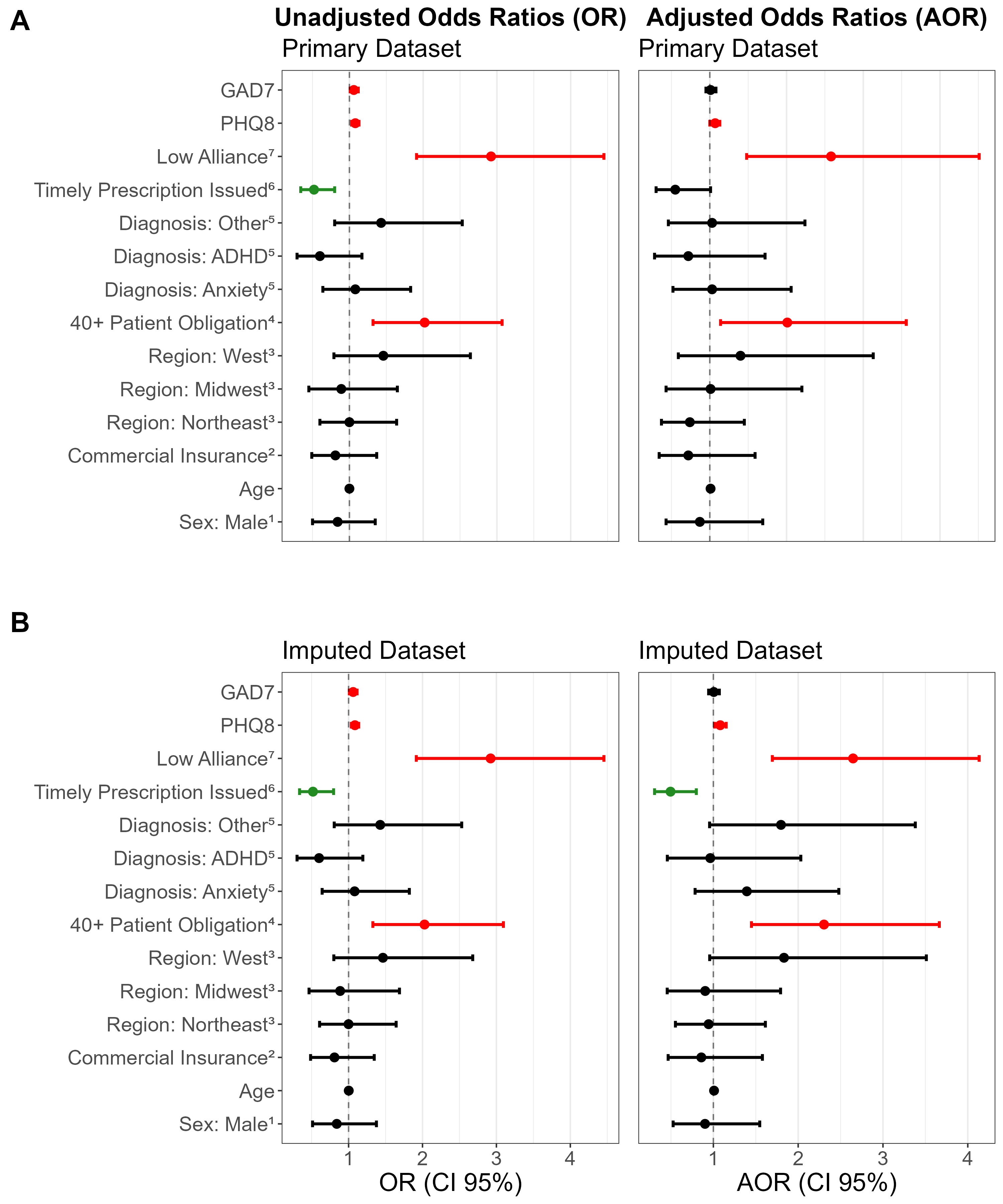
The secondary analysis used imputed datasets and yielded results consistent with the primary analysis—low therapeutic alliance, patient financial obligation, and PHQ-8 scores remained significantly associated with dropout in both unadjusted and adjusted models. Timely prescription was an independent factor and retained statistical significance in the imputed multivariate estimates. The unadjusted and adjusted ORs and p values for all variables in the primary and imputed analyses can be found in Table 2 and are visually represented in Figure 2.
Figure 2. Adjusted and unadjusted odds ratios for factors associated with early dropout. (A) Primary dataset with N=796 for univariate analyses (unadjusted odds ratios: OR) and N=554 for complete case multivariate (adjusted odds ratios: aOR). (B) Imputed dataset with N=796 for both univariate and multivariate analyses. 1Compared to female, 2Compared to non-commercial, 3Compared to South, 4Compared to <$40 patient obligation, 5Compared to depression, 6Compared to no prescription issued within 7 days of first visit, 7Compared to high alliance (WAI-SR total >50).
We evaluated whether having no financial obligation at the first visit influenced the likelihood of early dropout. Among patients who dropped out, 22.1% had no financial obligation, compared to 32.2% of those who remained in treatment. In the univariate analysis, the absence of financial obligation was associated with significantly lower odds of dropout (OR 0.60; 95% CI: 0.36–0.96). However, this association was no longer statistically significant in the multivariate model after adjusting for covariates, adjusted odds ratios (aOR) (95% CI): 0.62 (0.31–1.18).
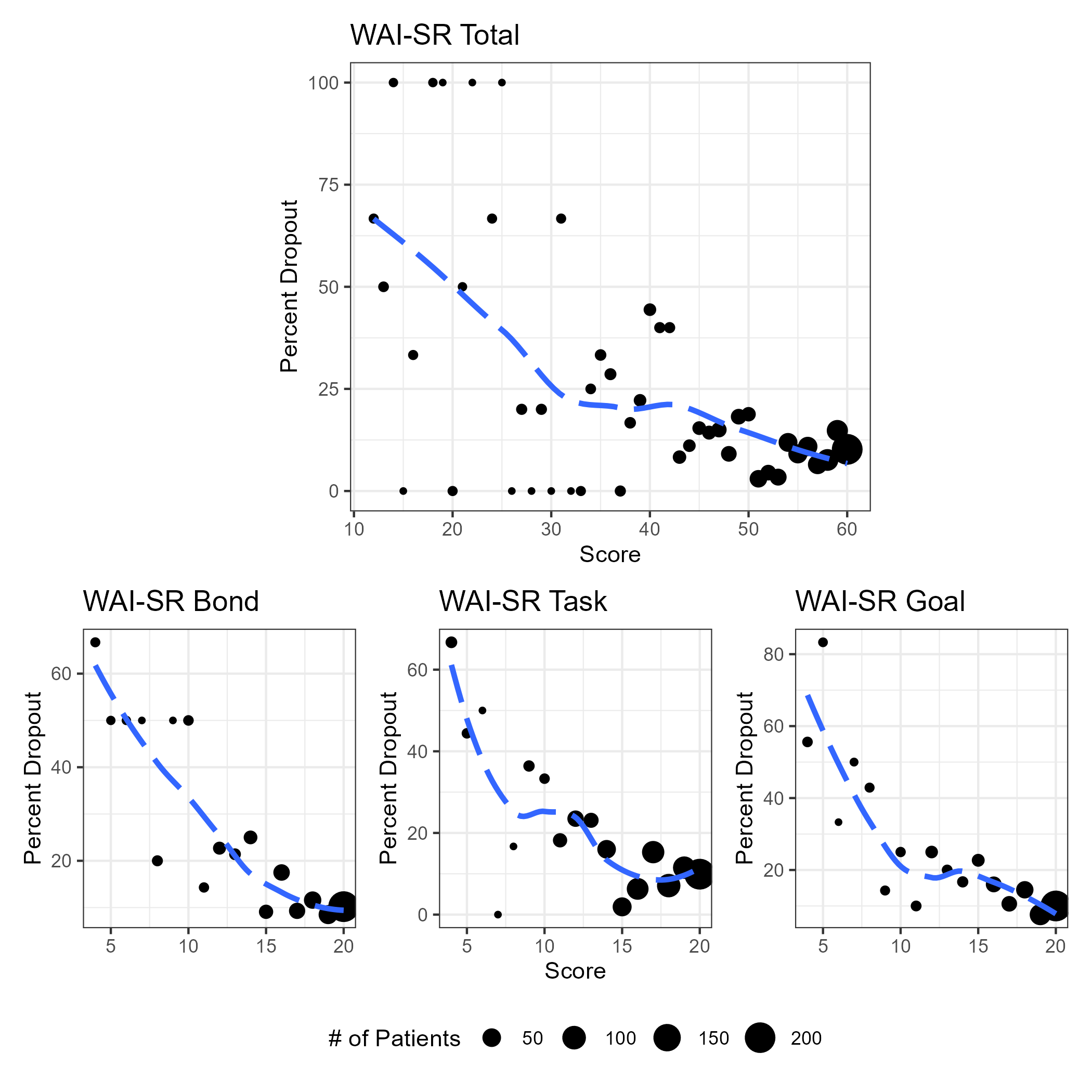
Additional analyses examined continuous versions of the WAI-SR total score and WAI-SR subscales in both univariate and multivariate models. The relationships between WAI-SR components and dropouts are visualized in Figure 3. Results from these supplementary models were consistent with our primary and secondary analyses and are reported in Supplementary Table 2.
Figure 3. Dropout percentage for Working Alliance Inventory-Short Revised (WAI-SR) total score and subscales.
Discussion
In a nationwide telepsychiatry practice, we found that therapeutic alliance and patient financial obligation were leading indicators of early dropout. Specifically, a WAI-SR total score below 50 and an out-of-pocket financial obligation exceeding $40 emerged as potential thresholds associated with elevated dropout risk.
There is considerable variation in reported rates of early mental health treatment discontinuation, with studies from the National Comorbidity Survey Replication (NCS-R) and the World Health Organization (WHO) estimating dropout rates of 22.4% and 30%, respectively [4,25]. Rates within the digital health space have been broadly accordant, ranging from 20% to 27.8% [5,19,26]. In contrast, our study had an early discontinuation rate of 13.2%, which is notably lower than the rates typically reported in prior dropout research [27]. The telehealth format may be a contributor to the low attrition rates observed, as one clinical trial found that participants treated via telehealth completed more visits than their in-person counterparts [28]. This effect may be explained by the removal of some traditional barriers in virtual care delivery, such as travel distance, transportation difficulties, and other logistical challenges [29].
In our analysis, patients with low alliance were more than 2.5 times as likely to discontinue treatment early compared to those in the high-alliance group. This association was robust, persisting across univariate, multivariate, and imputed models. We also examined each WAI-SR subscale independently and found that all three were strongly associated with dropout, with no single domain solely driving the effect. Although similar findings have been consistently reported in the broader literature, most prior studies have examined total alliance solely using continuous alliance scores and have not proposed practical thresholds that could help flag patients at elevated risk for dropout in a clinical setting [13,30,31]. We identified a WAI-SR total score of 50 as a cutoff point, consistent with a systematic scoping review that defined scores above 50 as indicative of good therapeutic alliance [32]. This finding serves as a preliminary estimate that future work can build upon to help address the current gap in actionable knowledge.
In accordance with evidence from the existing dropout literature, financial obligation was also identified as a key factor in early dropout [19,33]. Our cut point analysis identified $40 as the optimal threshold for first visit payment responsibility. This estimate should be interpreted with caution, as the confidence interval was very wide ($20–$375). The upper-bound of $375 likely reflects the right-skewed distribution of financial obligation data (Supplemental Figure 1). Although approximately 85% of the sample had first-visit payments of $100 or less, the higher end of the payment distribution extended to $710, which inflated the upper estimate of the confidence interval. Nonetheless, this association was pronounced—patients with out-of-pocket first-visit costs above $40 were more than twice as likely to drop out early, even after adjusting for potential covariates. It is also noteworthy that our empirically derived $40 cut point aligns with one of the most common copay amounts for outpatient mental health and specialist visits [34]. Additionally, we examined whether having no financial obligation affected the likelihood of attenuation. Although it was a significant independent feature in the univariate analysis, this effect was no longer significant after adjusting for variables such as therapeutic alliance and illness severity. This suggests that patients may tolerate some level of payment responsibility, provided it is modest and does not impose an excessive financial burden.
Other variables of interest in our analyses included illness severity measures (PHQ-8 and GAD-7) and whether the patient had been issued a prescription within seven days of their first visit. In the original, non-imputed dataset, only PHQ-8 remained significant after multivariate adjustment, whereas GAD-7 reached significance only in univariate analyses, and timely prescription issuance was significant in both the univariate and imputed models. Across all analyses, however, therapeutic alliance and financial obligation were more influential indicators of early dropout than illness severity and timely prescription issuance.
Limitations
Due to the retrospective observational nature of our study design, causality cannot be established. Moreover, clinical modality and therapeutic context may heavily influence dropout patterns. Therefore, generalizability of our findings to other domains and practices may be limited, underscoring the need for further exploration and replication. Limited generalizability is especially applicable to the $40 financial obligation cut point, which was derived from a highly skewed distribution and exhibited a large degree of uncertainty. As noted in the methods section, illness severity metrics were missing for 29.4% of our sample. Although these data were likely missing at random and our imputation analyses produced results consistent with the primary dataset, indicating minimal bias from missingness in the complete-case analysis, this nonetheless represents a substantial degree of missingness. Even with this limitation, after excluding patients with missing values, our complete-case sample of 554 compares favorably with the sample sizes reported in many prior dropout studies [22,29,35].
Conclusion
Our findings demonstrate that both therapeutic alliance and financial obligation are key determinants of early dropout in tele psychiatric care. Future prospective longitudinal research is needed to expand upon our findings, refine threshold estimates, and evaluate the impact of therapeutic alliance on long-term symptom improvement. Psychiatrists can operationalize these results by: (1) identifying patients with low early therapeutic alliance in order to schedule an alliance-repair session, offer supervisory consult, or reassign when indicated; and (2) flagging high first-visit copays to trigger financial navigation—cost review, generic prescribing, payment plans, insurance/benefit checks, lower-cost modalities, or spacing visits. Larger studies may seek to stratify analyses by primary diagnosis to refine estimates for diagnosis-specific patient profiles. In addition, there is considerable opportunity for future studies to leverage machine learning approaches towards the development of robust predictive models to identify those at risk for dropout at the outset of psychiatric treatment. Nevertheless, our study serves as a preliminary but important contribution to the dropout literature, laying the groundwork for the development of actionable thresholds to better identify and support patients at risk of early discontinuation.
References
2. Panchal N, Lo J. Exploring the Rise in Mental Health Care Use by Demographics and Insurance Status [Internet]. KFF; 2024 [cited 2025 Aug 27]. Available from: https://www.kff.org/mental-health/exploring-the-rise-in-mental-health-care-use-by-demographics-and-insurance-status/.
3. McBain RK, Schuler MS, Qureshi N, Matthews S, Kofner A, Breslau J, Cantor JH. Expansion of Telehealth Availability for Mental Health Care After State-Level Policy Changes From 2019 to 2022. JAMA Netw Open. 2023 Jun 1;6(6):e2318045.
4. Olfson M, Mojtabai R, Sampson NA, Hwang I, Druss B, Wang PS, et al. Dropout from outpatient mental health care in the United States. Psychiatric Services. 2009 Jul;60(7):898–907.
5. Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: a meta-analysis. J Consult Clin Psychol. 2012 Aug;80(4):547–59.
6. Werbart A, Oasi O. Unsuccessful Psychotherapies: When and How do Treatments Fail?. Lausanne: Frontiers Media SA; 2021. 154 p.
7. Barrett MS, Chua WJ, Crits-Christoph P, Gibbons MB, Casiano D, Thompson D. EARLY WITHDRAWAL FROM MENTAL HEALTH TREATMENT: IMPLICATIONS FOR PSYCHOTHERAPY PRACTICE. Psychotherapy (Chic). 2008 Jun 1;45(2):247–67.
8. Pentaraki AD. Treatment outcomes in depression: reducing drop-out rates in cognitive therapy. BJPsych Advances. 2018 Mar;24(2):101–9.
9. Sharf J, Primavera LH, Diener MJ. Dropout and therapeutic alliance: a meta-analysis of adult individual psychotherapy. Psychotherapy (Chic). 2010 Dec;47(4):637–45.
10. Waumans RC, Muntingh AD, Batelaan NM, van Balkom AJ. Understanding and preventing nonadherence and treatment dropout in adolescents and young adults with anxiety and depressive disorders. Front Psychiatry. 2023 Nov 22;14:1174285.
11. Khazaie H, Rezaie L, Shahdipour N, Weaver P. Exploration of the reasons for dropping out of psychotherapy: A qualitative study. Evaluation and program planning. 2016 Jun 1;56:23–30.
12. Cournoyer LG, Brochu S, Landry M, Bergeron J. Therapeutic alliance, patient behaviour and dropout in a drug rehabilitation programme: The moderating effect of clinical subpopulations. Addiction. 2007 Dec;102(12):1960–70.
13. Murphy ST, Garcia RA, Cheavens JS, Strunk DR. The therapeutic alliance and dropout in cognitive behavioral therapy of depression. Psychotherapy Research. 2022 Nov 17;32(8):995–1002.
14. Yeomans FE, Gutfreund J, Selzer MA, Clarkin JF, Hull JW, Smith TE. Factors related to dropouts by borderline patients: Treatment contract and therapeutic alliance. J Psychother Pract Res. 1994;3(1):16–24.
15. Haug T, Nordgreen T, Öst LG, Tangen T, Kvale G, Hovland OJ, et al. Working alliance and competence as predictors of outcome in cognitive behavioral therapy for social anxiety and panic disorder in adults. Behaviour Research and Therapy. 2016 Feb 1;77:40–51.
16. Pihlaja S, Stenberg JH, Joutsenniemi K, Mehik H, Ritola V, Joffe G. Therapeutic alliance in guided internet therapy programs for depression and anxiety disorders–a systematic review. Internet Interv. 2018 Mar 1;11:1–10.
17. Sareen J, Jagdeo A, Cox BJ, Clara I, Ten Have M, Belik SL, et al. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr Serv. 2007 Mar;58(3):357–64.
18. Mojtabai R. Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States: 1997–2002. Am J Public Health. 2005 Nov;95(11):2009–14.
19. Bugatti M, Owen J, Reese RJ, Coleman J, Richardson Z, Rasmussen W, et al. Access to care and cost as predictors of early psychotherapy dropout: Findings from a technology-enabled practice research group. Pract Innov (Wash D C). 2023 Mar;8(1):62–74.
20. Gmeinwieser S, Schneider KS, Bardo M, Brockmeyer T, Hagmayer Y. Risk for psychotherapy drop-out in survival analysis: The influence of general change mechanisms and symptom severity. J Couns Psychol. 2020 Nov;67(6):712–22.
21. Gersh E, Hallford DJ, Rice SM, Kazantzis N, Gersh H, Gersh B, et al. Systematic review and meta-analysis of dropout rates in individual psychotherapy for generalized anxiety disorder. J Anxiety Disord. 2017 Dec 1; 52:25–33.
22. Hanevik E, Røvik FM, Bøe T, Knapstad M, Smith OR. Client predictors of therapy dropout in a primary care setting: a prospective cohort study. BMC psychiatry. 2023 May 24;23(1):358.
23. Munder T, Wilmers F, Leonhart R, Linster HW, Barth J. Working Alliance Inventory‐Short Revised (WAI‐SR): psychometric properties in outpatients and inpatients. Clin Psychol Psychother. 2010 May;17(3):231–9.
24. Madley-Dowd P, Hughes R, Tilling K, Heron J. The proportion of missing data should not be used to guide decisions on multiple imputations. J Clin Epidemiol. 2019 Jun 1;110:63–73.
25. Fernandez D, Vigo D, Sampson NA, Hwang I, Aguilar-Gaxiola S, Al-Hamzawi AO, et al. Patterns of care and dropout rates from outpatient mental healthcare in low-, middle-and high-income countries from the World Health Organization's World Mental Health Survey Initiative. Psychol Med. 2021 Sep;51(12):2104–16.
26. Linardon J, Fuller-Tyszkiewicz M. Attrition and adherence in smartphone-delivered interventions for mental health problems: A systematic and meta-analytic review. J Consult Clin Psychol. 2020 Jan;88(1):1–13.
27. Linardon J, Fitzsimmons-Craft EE, Brennan L, Barillaro M, Wilfley DE. Dropout from interpersonal psychotherapy for mental health disorders: A systematic review and meta-analysis. Psychother Res. 2019 Oct 8;29(7):870–81.
28. Hernandez-Tejada MA, Zoller JS, Ruggiero KJ, Kazley AS, Acierno R. Early treatment withdrawal from evidence-based psychotherapy for PTSD: telemedicine and in-person parameters. Int J Psychiatry Med. 2014 Jul;48(1):33–55.
29. McGovern C, Athey A, Beale EE, Overholser JC, Gomez SH, Silva C. Who will stay and who will go? Identifying risk factors for psychotherapy dropout. Couns Psychother Res. 2024 Jun 17.
30. Stefana A, Fusar-Poli P, Vieta E, Youngstrom EA. Effectiveness of a Novel Web-Based Intervention to Enhance Therapeutic Relationships and Treatment Outcomes in Adult Individual Psychotherapy: Randomized Controlled Trial and Analysis of Predictors of Dropouts. JMIR Ment Health. 2024 Nov 27;11(1):e63234.
31. Steuwe C, Berg M, Driessen M, Beblo T. Therapeutic alliance and dropout in patients with borderline pathology receiving residential dialectical behavior therapy. BMC psychiatry. 2023 Aug 18;23(1):605.
32. van Lotringen CM, Jeken L, Westerhof GJ, Ten Klooster PM, Kelders SM, Noordzij ML. Responsible relations: a systematic scoping review of the therapeutic alliance in text-based digital psychotherapy. Front Digit Health. 2021 Jul 9;3:689750.
33. Ryan E. The therapeutic alliance in cognitive therapy for depression in combination with antidepressant medication: relations to subsequent symptom change and treatment retention. Master's thesis, The Ohio State University. 2009. p. 53.
34. Pollitz K, Lo J, Wallace R. Standardized Plans in the Health Care Marketplace: Changing Requirements [Internet]. KFF. 2023 [cited 2025 Sep 1]. Available from: https://www.kff.org/private-insurance/standardized-plans-in-the-health-care-marketplace-changing-requirements/.
35. De Salve F, Rossi C, Messina I, Grecucci A, Falgares G, Infurna MR, et al. Predicting dropout and non-response to psychotherapy for personality disorders: A study protocol focusing on therapist, patient, and the therapeutic relationship. BMC psychology. 2024 Nov 5;12(1):625.