Abstract
The case of a young girl with Dengue fever presenting with seizures and bilateral visual loss is presented. At the time of presentation, she had right hemiplegia and dysarthria but was not dysphasic. Fundoscopy revealed presence of macular and disc oedema in the right eye and vitreous haemorrhage in the left eye. Dengue IgM antibody was positive. Magnetic resonance imaging revealed a large intracerebral spontaneous haemorrhage. She had partial recovery of her hemiplegia and speech as well as of her vision on conservative treatment. The relevant literature relating to ocular involvement and strokes in association with Dengue fever has been reviewed.
Keywords
Dengue fever, Expanded Dengue Syndrome, Dengue ocular involvements, Strokes in Dengue fever
Introduction
Dengue is one of the most common arborvirus (Flavivirus group) infections affecting humans in recent times. Four different strains of the virus (DENV 1-4) affect humans causing illnesses varying from asymptomatic individuals to severe disease manifesting as Dengue Hemorrhagic Fever and Dengue Shock Syndrome. Neurological symptoms may occur in as high as 20% of cases with age range varying from infancy to the elderly [1,2]. The two most common forms of CNS infections related to Dengue are Dengue Encephalitis and Dengue Encephalopathy. Stroke is an uncommon complication of Dengue fever and both hemorrhagic and ischemic strokes might occur [1]. Ocular involvement in Dengue is often missed out when patients are admitted in general medical wards. All patients with Dengue need to be examined by ophthalmologists with pupillary dilation for proper visualization of the whole of the retina. Herein we report a case of a young girl with Dengue fever who had developed both hemorrhagic stroke as well as bilateral visual loss due to maculopathy and intraocular hemorrhage. The relevant literature would be briefly reviewed.
Case History
A 16-year-old girl presented with history of having high fever with severe myalgia and arthralgia. She was admitted in a local hospital where she had one episode of a generalized tonic clonic seizure following which she started complaining of loss of vision in both eyes simultaneously but there had been no ocular or peri-ocular pain. She continued to remain drowsy. At that stage, she was transferred to the ICU of a city hospital. Three days prior to her admission in the local hospital, she also had a dizzy spell on her way to school. She possibly had brief period of black out but there was no recollection of fall, tongue bite, involuntary micturition, or defaecation with no eyewitnesses available. On admission her GCS was 10/15; visual acuities in both eyes were down to perception of light, pupils 4 mm non-reactive, and she had no neck stiffness. A dense right hemiplegia was noted with upper motor neuron type right facial weakness. Both planters were upgoing. Fundoscopy revealed macular oedema with star formation and optic disc swelling in the RIGHT eye (Figure 1) and vitreous haemorrhage in the LEFT eye (Figure 2).
Figure 1. Fundoscopy in right eye revealing macular oedema with star formation and optic disc swelling. (Reprinted from Reference 2 with permission).
Figure 2. Fundoscopy in left eye revealing vitreous haemorrhage. (Reprinted from Reference 2 with permission).
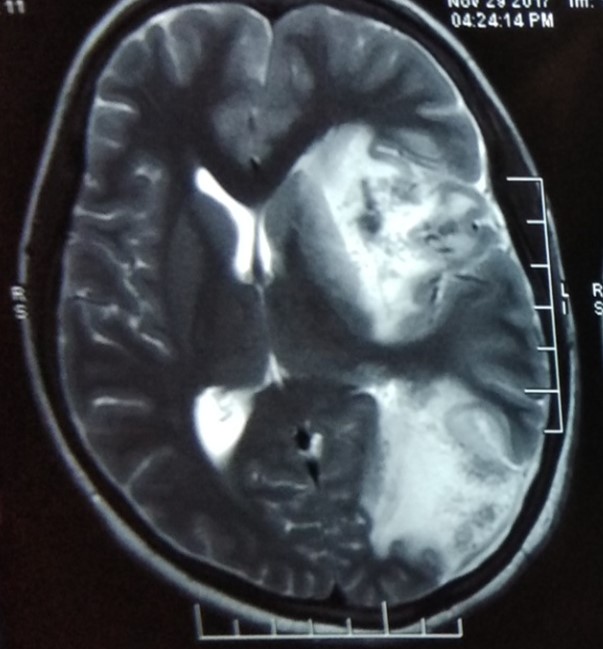
Investigations revealed severe anaemia (Hb 6.2G%), marked thrombocytopenia (varying from 9000 – 21000/cmm on different dates), raised CRP (45mg), negative serology for malaria, hepatitis viruses (B and C) Chikungunya and Japanese encephalitis viruses. Dengue IgM antibody was positive. ANA(Hep2) and ant-iRNP/ sm antibodies were positive in high titres in the serum. MRI brain showed a large left fronto-parietal intracerebral haemorrhage with shift of midline structures to the right (Figure 3).
She was treated conservatively. Fever subsided after three days, sensorium improved and there had been no recurrence of seizures. Unfortunately, she was left with significant weakness in her right limbs and had no vision in either eye except for finger counting at less than one foot. She remained dysarthric but not dysphasic.
Figure 3. MRI of brain (T2 sequence) showing large left parietal intracerebral haemorrhage and oedema with shift of midline structures to the right (Reprinted from Reference 2 with permission).
Discussion and a Mini Review
This young girl with Dengue fever developed a multisystemic disease. In addition to fever with myalgia and arthralgia, but no rash, she had involvement of hematopoietic system (anaemia, thrombocytopenia); central nervous system (seizures, altered sensorium and haemorrhagic stroke), ocular involvement (macular oedema, optic disc swelling and vitreous haemorrhage) and immune system (raised CRP, presence of autoantibodies). Seizures in the present case may have various etiologies. The neurotropism of Dengue virus is well known. This girl might have developed an encephalopathy related to the Dengue virus or she might have got an encephalitis as well, manifested by seizure and altered sensorium. Furthermore, as she developed a frank intracerebral hemorrhage, it is quite possible that the initial presentation of that haemorrhagic stroke had been the seizure as occurs in about 15% of cases of strokes, majority of which are hemorrhagic ones [2].
Such atypical manifestations involving neurological, gastrointestinal, respiratory, cardiac, renal, and eye involvement are gaining greater recognition in current times and is being designated as the Expanded Dengue Syndrome.
The Expanded Dengue Syndrome (EDS) refers to those manifestations involving multiple organ systems in cases of Dengue fever. Certain high-risk groups such as pregnant women, infants, the elderly, patients with coronary artery disease, hemoglobinopathies, and immune-compromised individuals are particularly susceptible to developing EDS Multi-organ involving features include the following [1,3].
Cardiac
Sinus bradycardia or tachycardia, atrio-ventricular block, sino-atrial exit block, ventricular bigeminy and/or trigeminy, paroxysmal supraventricular tachycardia, atrial fibrillation, myocarditis, pericarditis, and pericardial effusion.
Neurological
Encephalopathy, encephalitis, seizures, strokes (both ischemic and hemorrhagic), acute disseminated encephalomyelitis, cranial nerve palsies, acute transverse myelitis, Guillain Barre syndrome, myalgias, myositis and rhabdomyolysis.
Gastrointestinal
Acute liver failure, acalculous cholecystitis, acute pancreatitis, and bleeding gastric ulcers.
Renal
Acute kidney injury.
Respiratory
Adult respiratory distress syndrome, pneumonitis/ bronchiolitis, and pulmonary haemorrhages.
Haematological
Splenomegaly, hemophagocytic lympho-histiocytosis, aplastic anaemia, and thrombotic thrombocytopenic purpura.
Ocular involvement in Dengue
Ocular involvement in Dengue had been recognized as far back as in the 1940s. But such involvements are currently being recognized more frequently and are being studied more thoroughly due the availability of such techniques as OCT and Infrared fundus photography. Kapoor et al. retrospectively assessed 134 Dengue fever patients, among whom up to 40% had ocular manifestations [4]. In the present case two different types of pathologies have been noted in the two eyes – macular and disc oedema in the right eye and vitreous haemorrhage in the left. In both eyes very significant visual loss resulted.
The ocular involvements described so far include maculopathy, blurred vision, scotoma, floaters, subconjunctival haemorrhage, uveitis, vitritis, retinal haemorrhaging, retinal venular widening, higher retinal vascular dimension, retinal vascular sheathing, retinal pigment epithelium mottling, tortuous blood vessels, acute macular neuro-retinopathy, macular/ intra-retinal haemorrhages [1,2]. The exact pathogenetic mechanisms for all the ocular manifestations are not fully understood. While the often associated thrombocytopenia may be contributory in the hemorrhagic lesions, there indeed are other factors operating. Some suggested ones include: Dengue associated vasculopathy, proinflammatory cytokines, and immune mechanisms [1].
Symptoms of ocular involvement are suggested by visual loss, ocular pain, redness, metamorphopsia, impaired colour vision, diplopia, eye flashes and floaters, haloes, and photophobia. Lesions located in the peripheral retina may be asymptomatic and difficult to visualize. Hence, ocular involvement in Dengue is often under-reported [5].
Dengue eye disease can be unilateral or bilateral and the onset of ocular symptoms range from 2 to 5 days after the onset of fever and most ocular symptoms have been noted within one day after the peak of thrombocytopenia [6].
However, some complications, e.g., uveitis, can occur 3–5 months after Dengue infection [7]. Significant predictors of ocular symptoms included leukopenia and hypoalbuminemia, which could predispose patients to an opportunistic infection of ocular tissues and hyper permeability [8].
Ocular complications involve: (1) the anterior segment of the eye, e.g., subconjunctival haemorrhage, uveitis, or a shallow anterior chamber (2) the posterior segment of the eye, e.g., maculopathy, macular oedema, optic neuropathy, or vitreous haemorrhage [9].
Study by Kapoor et al. accounted for most cases of Dengue-related subconjunctival haemorrhage of which majority had petechial haemorrhages present in the conjunctivae. Only a few had diffuse haemorrhages noted in one to four quadrants [4].
Anterior uveitis without evidence of posterior segment involvement can happen rarely and be associated with progressive loss of vision [7].
Dengue maculopathy is the most recognized and studied ocular complications of Dengue. It has been found to be serotype and geography related. There is only one study relating maculopathy to be serotype specific with DENV-1 epidemic causing 10% incidence while there were no cases during DENV-2 epidemic [10]. Macular oedema and macular haemorrhage were common findings in symptomatic patients with maculopathy [10]. Blurring of vision and central scotoma are the most frequent visual complaints in patients of Dengue related maculopathy. Exudative maculopathy and small haemorrhages located in the optic nerve fibre layer can produce reduced visual acuity [11].
Haemorrhages associated with dengue-related maculopathy are mostly intraretinal and can take the form of dot, blot, or flame-shaped haemorrhages. These haemorrhages are also found to be associated with venous sheathing [12].
Vascular sheathing and vasculitis were often found in association with macular haemorrhage [13].
Dengue-related foveolitis refers to the yellow-orange lesion at the fovea of patients with Dengue maculopathy which corresponds to a disruption of the outer neurosensory retina in optical coherence tomography (OCT). Dengue-related maculopathy commonly presents with macular oedema. Teoh et al. [11] further categorized macular oedema in three types based on their appearance on OCT. The three patterns of macular oedema on OCT can be described as - in type 1, where there is diffuse oedema, type 2, which is cystoid oedema, and type 3, which is cystic foveolitis.
Central serous chorioretinopathy (CSCR) is a poorly understood phenomenon and more so when it occurs in Dengue viral infection. Several factors like stress related to a viral infection, catecholamine release, steroid therapy, and genetic factors may be operative in its generation [1].
Optic neuropathy is relatively uncommon compared to other dengue-related ocular pathologies. The series by Teoh et al. [11] reported disc swelling in only 3.1% of eyes with Dengue related ophthalmic complications. Optic disc swelling, hyperaemia, and disc haemorrhages are common presentations of Dengue-related optic neuropathy. The intrinsic pathology in the affected optic nerves is not known but it is likely to be different from that encountered in demyelinating optic neuritis [14].
Bilateral visual loss secondary to pituitary adenoma and bilateral vitreous haemorrhage associated with Dengue fever have also been reported [15,16].
Most patients recover spontaneously to their best-corrected visual acuity without specific treatment between 1 week and 3 months after onset [17].
Nevertheless, some people might complain of persistent scotoma, and visual impairment could remain in cases of severe exudative maculopathy and retinal haemorrhage [7,18].
Fundus fluorescein and indocyanine green angiography (FFA), optical coherence tomography, and visual field testing are useful tools in the diagnosis of ophthalmic complication of Dengue.
Ophthalmic investigations were performed mostly for posterior segment pathology. A relative central scotoma is demonstrated on the Amsler chart in most patients both of which correspond to visual field testing by an automated Humphrey field analyzer [6,11]. Amsler grid test abnormalities are more likely to occur in patients with Dengue maculopathy [17].
Fundus fluorescein angiography (FFA) demonstrates mainly vascular occlusion or leakage and helps in the diagnosis of vein occlusions and vasculitis [19].
FFA may show leakage of the optic disc and retinal vessels, retinal pigment epithelium defects, and macular nonperfusion [12]. Blocked fluorescence, venular occlusion, and venular leakage can be found on FFA in Dengue maculopathy. Optical coherence tomography may show diverse patterns of maculopathy including diffuse retinal thickening, cystoid macular oedema, and foveolitis [14].
Most Dengue-related ocular conditions resolve spontaneously. Steroids may be helpful when an autoimmune mechanism is suspected, but they should be avoided in the stage of acute viremia. The prognosis of Dengue-related ophthalmic complications is favorable. Almost all patients become normal or report improvement in vision [9].
The mechanisms underlying Dengue infection-related ocular signs remain unclear, but could involve immune processes with possible association with dengue serotyping [6,12].
Stroke in Dengue
The incidence of Dengue-associated cerebrovascular complications is unknown, although haemorrhagic stroke seems more common than ischemic stroke. During an epidemic in India, 1148 laboratory-confirmed dengue patients were admitted to hospital and three had a stroke (0?26%) [20]. Most patients have intracranial bleeding a week after fever onset [21].
Acute intracranial bleeding can arise without other (visible) hemorrhagic manifestations. It may occur during the convalescence period and can be potentially fatal [21,22].
Although commonly hemorrhagic features in severe Dengue include ecchymosis, petechial hemorrhage, epistaxis, and gastrointestinal bleed, acute intracranial bleeding can occur in absence of these systemic hemorrhagic manifestations. Clinical presentation includes fever, moderate to severe headache, vomiting, acute hemiparesis, and loss of consciousness [1].
Intracranial hemorrhage is an uncommon complication of severe Dengue, but the exact prevalence had not been studied. Intracranial bleeds may be localized or diffuse involving commonly cerebrum, ventricles, and less commonly cerebellum [20]. Subdural [23,24], extradural, as well as subarachnoid hemorrhages [25] were also reported. Basal ganglia hemorrhages and multiple lobar hemorrhages have been described [26].Less common clinical forms of intracranial bleeding include multiple acute subdural hematomas [21], pituitary apoplexy [27], subarachnoid hemorrhage, and focal subarachnoid hemorrhage associated with transient thrombocytopenia [28].
Ischemic strokes may occur as watershed infarctions, cortical infarctions, and lacunar infarctions. In cases with ischemic stroke, meningo-vasculitis, or a transient hypercoagulable state during Dengue infection was postulated as the pathogenetic mechanism [22,29].
Increased vascular permeability, plasma leakage, vasculitis, prolonged prothrombin time, severe thrombocytopenia, hepatic dysfunction, and mild degree of disseminated intravascular coagulation may contribute to the pathogenesis of Dengue-associated hemorrhagic strokes [30].
It had been demonstrated that platelet counts did not correlate with the incidence of ICH; this would raise the possibility of interplay of multiple factors in stroke pathogenesis. Such factors may include vasculopathy, coagulopathy, platelet dysfunction, and thrombocytopenia [30]. Presence of immune markers in CSF suggests break down of blood–brain barrier and blood–CSF barrier in patients with severe Dengue inducing an immune mediated vasculopathy. The NS1 antigen may also activate conversion of plasminogen to plasmin and thereby induce fibrinolysis. Thrombocytopenia and platelet dysfunction are well known components of severe Dengue infection. All these would promote development of intracranial bleeding.
No guidelines for management of Dengue related intracranial hemorrhage exists and this contributes to increased mortality and morbidity.
Concluding Remarks
Ocular involvement in Dengue is often missed out when patients are admitted in general medical wards. All patients with Dengue need to be examined by ophthalmologists with pupillary dilation for proper visualization of the whole of the retina. Symptomatic patients should have OCT for proper assessment. Treatment of Dengue fever with ocular complication is largely supportive, however, administration of steroid may be considered in case of macular and/or optic nerve involvement, poor presenting visual acuity, and evidence of progression of the ocular disease. It would be unwise to subject Dengue patients with altered sensorium to lumbar puncture without proper evaluation of their coagulation profile and a brain imaging, as they may be harboring a space occupying lesion like a large hematoma, intracerebral or extracerebral, related to their thrombocytopenia and other factors, because of the risk of precipitating brain herniation.
References
2. Chakravarty A. The dengue maladies (case series 1.2). In neurology & internal medicine – a case-based study. In: Chakravarty A, editor. New Delhi London: Jaypee BrothersMedical Publishers; 2021. p. 40-55.
3. Puccioni-Sohler M, Orsini M, Soares CN. Dengue: a new challenge for neurology. Neurology International. 2012 Oct;4(3):e15.
4. Kapoor HK, Bhai S, John M, Xavier J. Ocular manifestations of dengue fever in an East Indian epidemic. Canadian Journal of Ophthalmology. 2006 Dec 1;41(6):741-6.
5. Kumar R, Mathur A, Singh KB, Sitholey P, Prasad M, Shukla R, et al. Clinical sequelae of Japanese encephalitis in children. The Indian Journal of Medical Research. 1993 Jan 1;97:9-13.
6. Teoh SC, Chee CK, Laude A, Goh KY, Barkham T, Ang BS. Eye Institute dengue-related Ophthalmic Complications Work group. Optical coherence tomography patterns as predictors of visual outcome in dengue-related maculopathy. Retina. 2010;30(3):390-8.
7. Gupta A, Srinivasan R, Setia S, Soundravally R, Pandian DG. Uveitis following dengue fever. Eye. 2009 Apr;23(4):873-6.
8. Seet RC, Quek AM, Lim EC. Symptoms and risk factors of ocular complications following dengue infection. Journal of Clinical Virology. 2007 Feb 1;38(2):101-5.
9. Yip VC, Sanjay S, Koh YT. Ophthalmic complications of dengue fever: a systematic review. Ophthalmology and Therapy. 2012 Dec;1(1):1-9.
10. Chee E, Sims JL, Jap A, Tan BH, Oh H, Chee SP. Comparison of prevalence of dengue maculopathy during two epidemics with differing predominant serotypes. American Journal of Ophthalmology. 2009 Dec 1;148(6):910-3.
11. Teoh SC, Chee CK, Laude A, Goh KY, Barkham T, Ang BS, Eye Institute Dengue-related Ophthalmic Complications Workgroup. Optical coherence tomography patterns as predictors of visual outcome in dengue-related maculopathy. Retina. 2010 Mar 1;30(3):390-8.
12. Bacsal KE, Chee SP, Cheng CL, Flores JV. Dengue-associated maculopathy. Archives of Ophthalmology. 2007 Apr 1;125(4):501-10.
13. Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations of dengue fever. Ophthalmology. 2004 Nov 1;111(11):2057-64.
14. Teoh SC, Chee CK, Laude A, Goh KY, Barkham T, Ang BS. Eye Institute dengue-related Ophthalmic Complications Work group. Optical coherence tomography patterns as predictors of visual outcome in dengue-related maculopathy. Retina. 2010;30(3):390-8.
15. Sanjay S, Au Eong KG. Bilateral vitreous haemorrhage associated with dengue fever. Eye. 2007 Jan;21(1):144-5.
16. Kumar V, Kataria R, Mehta V. Dengue hemorrhagic fever: a rare cause of pituitary tumor hemorrhage and reversible vision loss. Indian Journal of Ophthalmology. 2011 Jul 1;59(4):311-312.
17. Su DH, Bacsal K, Chee SP, Flores JV, Lim WK, Cheng BC, et al. Dengue Maculopathy Study Group. Prevalence of dengue maculopathy in patients hospitalized for dengue fever. Ophthalmology. 2007 Sep 1;114(9):1743-7.
18. Siqueira RC, Vitral NP, Campos WR, Oréfice F, de Moraes Figueiredo LT. Ocular manifestations in dengue fever. Ocular Immunology and Inflammation. 2004 Jan 1;12(4):323-7.
19. Quek DT, Barkham T, Teoh SC. Recurrent bilateral dengue maculopathy following sequential infections with two serotypes of dengue virus. Eye. 2009 Jun;23(6):1471-2.
20. Mathew S, Pandian JD. Stroke in patients with dengue. Journal of Stroke and Cerebrovascular Diseases. 2010 May 1;19(3):253-6.
21. Kumar R, Prakash O, Sharma BS. Intracranial hemorrhage in dengue fever: management and outcome: a series of 5 cases and review of literature. Surgical Neurology. 2009 Oct 1;72(4):429-33.
22. Verma R, Sahu R, Singh A, Atam V. Dengue infection presenting as ischemic stroke: An uncommon neurological manifestation. Neurology India. 2013 May 1;61(3):317.
23. Kumar R, Prakash O, Sharma BS. Dengue hemorrhagic fever: a rare presentation as atypical acute subdural hematoma. Pediatric Neurosurgery. 2008;44(6):490-2.
24. Jain N, Gutch M, Kumar V, Naik A. A fatal combo of dengue shock syndrome with acute subdural hematoma. Neurology India. 2012;60(1):105.
25. Ferreira ML, Cavalcanti CG, Coelho CA, Mesquita SD. Neurological manifestations of dengue: study of 41 cases. Arquivos de Neuro-psiquiatria. 2005;63:488-93.
26. Nimmannitya S, Thisyakorn U, Hemsrichart V. Dengue haemorrhagic fever with unusual manifestations. The Southeast Asian Journal of Tropical Medicine and Public Health. 1987 Sep 1;18(3):398-406.
27. Kumar V, Kataria R, Mehta V. Dengue hemorrhagic fever: a rare cause of pituitary tumor hemorrhage and reversible vision loss. Indian Journal of Ophthalmology. 2011 Jul 1;59(4):311.
28. Patey O, Ollivaud L, Breuil J, Lafaix C. Unusual neurologic manifestations occurring during dengue fever infection. The American Journal of Tropical Medicine and Hygiene. 1993 Jun 1;48(6):793-802.
29. Liou LM, Lan SH, Lai CL. Dengue fever with ischemic stroke: a case report. The Neurologist. 2008 Jan 1;14(1):40-2.
30. Basu A, Chaturvedi UC. Vascular endothelium: the battlefield of dengue viruses. FEMS Immunology & Medical Microbiology. 2008 Aug 1;53(3):287-99.